General Ophthalmic Problems
13.1 Acquired Cataract
Symptoms
Slowly progressive visual loss or blurring, usually over months to years, affecting one or both eyes. Glare, especially in bright sun or from oncoming headlights while driving at night, and altered color perception may occur, but not to the same degree as in optic neuropathies. The characteristics of the cataract determine the particular symptoms.
Signs
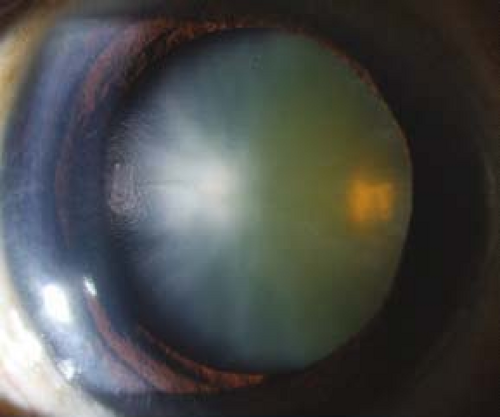
(See Figure 13.1.1.)
Critical. Opacification or discoloration of the normally clear crystalline lens.
Other. Blurred view of the retina with dimming of red reflex on retinoscopy. Myopic shift from nuclear sclerosis may cause increased near vision—so-called “second sight.” A cataract alone does not cause a relative afferent pupillary defect (RAPD).
Etiology
Age-related: Most common. Advanced forms include mature, hypermature, and morgagnian.
Presenile: Diabetes, myotonic dystrophy, and atopic dermatitis.
Trauma: Penetrating, concussion (vossius ring), and electric shock.
Toxic: Steroids in any form, miotics, antipsychotics (e.g., phenothiazines), and others.
Secondary.
Chronic anterior uveitis. SEE 12.1, ANTERIOR UVEITIS (IRITIS/IRIDOCYCLITIS).
History of vitrectomy.
Ionizing radiation.
Tumor (ciliary body).
Acute angle closure glaucoma: Glaucomflecken. SEE 9.4, ACUTE ANGLE CLOSURE GLAUCOMA.
Degenerative ocular disease: Retinitis pigmentosa, Leber congenital amaurosis, gyrate atrophy, Wagner and Stickler syndromes associated with posterior subcapsular cataracts, and others.
Endocrine/metabolic/chromosomal.
Diabetes: Juvenile form characterized by rapidly progressing white “snowflake” opacities in the anterior and posterior subcapsular locations. Age-related cataracts form earlier than in nondiabetics.
Hypocalcemia: Small, white, iridescent cortical changes, usually seen in the presence of tetany.
Wilson disease: Red-brown pigment deposition in the cortex beneath the anterior capsule (a “sunflower” cataract). SEE 13.9, WILSON DISEASE.
Myotonic dystrophy: Multicolored birefringent opacities, “Christmas-tree” cataract behind the anterior capsule.
Others: Down syndrome, neurofibromatosis type 2 (posterior subcapsular cataract), etc.
Types
Nuclear: Yellow or brown discoloration of the central lens. Typically blurs distance vision more than near (myopic shift).
Posterior subcapsular: Plaque-like opacity near the posterior aspect of the lens. Best seen with retroillumination as a dark shadow against the red reflex. Glare and difficulty reading are common complaints. Symptoms may improve postdilation. Associated with ocular inflammation, steroid use, diabetes, trauma, or radiation. Classically occurs in patients <50 years of age.
Cortical: Vacuoles and radial or spoke-like opacities in the periphery that expand to involve the anterior and posterior lens. Glare is the most common complaint. Often asymptomatic until central changes develop.
Work-Up
Determine the etiology, whether the cataract is responsible for the decreased vision, and whether surgical removal would improve vision.
History: Medications (e.g., tamsulosin and other drugs used for urinary retention [alpha-1 antagonists] strongly associated with intraoperative floppy iris syndrome)? Systemic diseases? Trauma? Ocular disease or poor vision before the cataract?
Complete ocular examination, including distance and near vision, pupillary examination, and refraction. When best corrected acuity is 20/30 or better, glare testing is helpful to demonstrate decreased vision. A dilated slit lamp examination using both direct and retroillumination techniques is required to view the cataract properly. Fundus examination, concentrating on the macula, is essential in ruling out other causes of decreased vision.
For preoperative planning, note the degree of pupil dilation, density of the cataract, and presence or absence of pseudoexfoliation, phacodonesis (quivering of the lens indicating zonular damage or weakness), or cornea guttae.
B-scan ultrasonography (US) if the fundus is not visible to rule out detectable posterior segment disease.
The potential acuity meter (PAM) or laser interferometry can be used to estimate the visual potential when cataract extraction is considered in an eye with posterior segment disease.
 NOTE: PAM and laser interferometry often overestimate the eye’s visual potential in the presence of macular holes or macular pigment epithelial detachments. Interferometry also overestimates visual potential in cases of amblyopia. Near vision is often the most accurate manner of evaluating macular function if the cataract is not too dense. Nonetheless, both PAM and laser interferometry are useful clinical tools.
NOTE: PAM and laser interferometry often overestimate the eye’s visual potential in the presence of macular holes or macular pigment epithelial detachments. Interferometry also overestimates visual potential in cases of amblyopia. Near vision is often the most accurate manner of evaluating macular function if the cataract is not too dense. Nonetheless, both PAM and laser interferometry are useful clinical tools.
Keratometry readings and measurement of axial length are required for determining the power of the desired intraocular lens (IOL). Corneal pachymetry or endothelial cell count is occasionally helpful if corneal guttae are present.
Treatment
Cataract surgery may be performed for the following reasons:
To improve visual function in patients with symptomatic visual disability.
As surgical therapy for ocular disease (e.g., lens-related glaucoma or uveitis).
To facilitate management of ocular disease (e.g., to allow a view of the fundus to monitor or treat diabetic retinopathy or glaucoma)
Correct any refractive error (e.g., prescription of corrective lenses) if the patient declines cataract surgery.
A trial of mydriasis (e.g., cyclopentolate 1% b.i.d. to t.i.d.) may be used successfully in some patients who desire nonsurgical treatment. The benefits of this therapy are only temporary. Most useful for posterior subcapsular cataracts.
Follow-Up
Unless there is a secondary complication from the cataract (e.g., glaucoma), a cataract itself does not require urgent action. Patients who decline surgical removal are reexamined annually or sooner if symptoms worsen.
If congenital, SEE 8.8, PEDIATRIC CATARACT.
13.2 Subluxed or Dislocated Crystalline Lens
Definition
Subluxation: Partial disruption of the zonular fibers. Lens is decentered but remains partially visible through the pupil.
Dislocation: Complete disruption of the zonular fibers. Lens is fully displaced out of the pupillary aperture.
Symptoms
Decreased vision, double vision that persists when covering one eye (monocular diplopia).
Signs
(See Figure 13.2.1.)
Critical. Decentered or displaced lens, iridodonesis (quivering of the iris), phacodonesis (quivering of the lens).
Other. Change in refractive error, marked astigmatism, cataract, angle closure glaucoma as a result of pupillary block, acquired high myopia, vitreous in the anterior chamber, asymmetry of the anterior chamber depth.
Etiology
Trauma: Most common. Results in subluxation if >25% of the zonular fibers are ruptured. Need to rule out a predisposing condition (see other etiologies).
Pseudoexfoliation: Flaky material seen as scrolls in a “target pattern” on anterior lens capsule; associated with glaucoma and poor pupillary dilation; higher risk of complications during cataract surgery due to weak zonular fibers (SEE 9.11, PSEUDOEXFOLIATION SYNDROME/EXFOLIATIVE GLAUCOMA).
Marfan syndrome: Bilateral lens subluxation, classically superiorly and temporally. Increased risk of retinal detachment. Autosomal dominant with cardiomyopathy, aortic aneurysm, aortic dissection, tall stature with long extremities, and kyphoscoliosis.
Homocystinuria: Bilateral lens subluxation, classically inferiorly and nasally. Increased risk of retinal detachment. Autosomal recessive often with mental retardation, skeletal deformities, high incidence of thromboembolic events (particularly with general anesthesia). Lens subluxation may be the first manifestation in patients with mild disease.
Weill–Marchesani syndrome: Small lens can dislocate into the anterior chamber, causing reverse pupillary block. Usually autosomal recessive with short fingers and stature,
seizures, microspherophakia (small, round lens), myopia, no mental retardation.
Others: Acquired syphilis, congenital ectopia lentis, simple ectopia lentis, aniridia, Ehlers–Danlos syndrome, Crouzon syndrome, hyperlysinemia, sulfite oxidase deficiency, high myopia, chronic inflammation, hypermature cataract, etc.
Work-Up
History: Family history of the disorders listed? Trauma? Systemic illness (e.g., syphilis)? Neurologic symptoms (e.g., seizures)?
Determine whether the condition is unilateral or bilateral. Determine direction of lens displacement and evaluate for subtle phacodonesis by observing the lens during back and forth saccadic eye movements. Check for pseudoexfoliation. Evaluate for acute or remote signs of ocular trauma including hyphema, angle recession, iridodialysis, cyclodialysis, retinal tears, and detachments.
Systemic examination: Evaluate stature, extremities, hands, and fingers; often in conjunction with an internist, including blood and urine tests to rule out homocystinuria and echocardiography to rule out aortic aneurysms in patients with possible Marfan syndrome. Consider genetic testing when appropriate and available.
Syphilis screening tests (RPR or VDRL and FTA-ABS or treponemal-specific assay).
Treatment
Lens dislocated into the anterior chamber.
Dilate the pupil, place the patient on his or her back, and attempt to replace the lens into the posterior chamber by head manipulation. It may be necessary to indent the cornea after topical anesthesia with a Zeiss gonioprism or cotton swab to reposition the lens. After the lens is repositioned in the posterior chamber, constrict the pupil with pilocarpine 0.5% to 1% q.i.d. and perform a peripheral laser iridotomy to prevent pupillary block.
or
Surgically remove the lens and consider placing an IOL (preferred treatment if significant cataract, corneal decompensation, prior treatment failure, recurrent dislocation, or compliance issues with pilocarpine).
Lens dislocated into the vitreous.
Lens capsule intact, patient asymptomatic, no signs of inflammation: Observation versus pars plana lensectomy and possible IOL placement.
Lens capsule broken with intraocular inflammation: Pars plana lensectomy with possible IOL placement.
Subluxation.
Asymptomatic: Observe.
Uncorrectable astigmatism, unstable refractive errors, or monocular diplopia: Surgical removal of the lens and possible IOL placement.
Symptomatic cataract: Options include surgical removal of the lens, mydriasis (e.g., atropine 1% daily) and aphakic correction (i.e., contact lens if other eye is phakic or pseudophakic to prevent anisometropia), pupillary constriction (e.g., pilocarpine 4% gel q.h.s.) and phakic correction, or a large optical iridectomy (away from the lens) with aphakic correction.
Pupillary block: Treatment is identical to that for aphakic pupillary block. SEE 9.16, POSTOPERATIVE GLAUCOMA.
If Marfan syndrome suspected: Refer the patient to a cardiologist for an annual echocardiogram and management of any cardiac-related abnormalities. Prophylactic systemic antibiotics may be needed if the patient undergoes surgery (or a dental procedure) to prevent endocarditis.
If homocystinuria is suspected: Refer to an internist. The usual therapy consists of:
Pyridoxine (vitamin B6) daily oral supplementation and a methionine-restricted, cysteine-supplemented diet.
Avoid surgery if possible because of the risk of thromboembolic complications. If surgical intervention is necessary, anticoagulant therapy is indicated in conjunction with internist.
Follow-Up
Depends on the etiology, degree of subluxation or dislocation, and symptoms.
13.3 Pregnancy
Anterior Segment Changes
Transient loss of accommodation and increased corneal thickness/edema and curvature. Refractive change likely results from a shift in fluid or hormonal status and will likely normalize after delivery. Defer prescribing new glasses until several weeks postpartum. Rigid contact lens wearers may experience contact lens intolerance due to corneal changes.
Preeclampsia/Eclampsia
A worldwide leading cause of maternal/fetal/neonatal morbidity and mortality. Occurs in 2% to 5% of pregnancies but may approach 10% in developing countries. Occurs after 20 weeks of gestation; most commonly in primigravids.
Symptoms
Headaches, blurred vision, photopsias, diplopia, and scotomas.
Signs
Systemic
Preeclampsia or pregnancy-induced hypertension: Hypertension and proteinuria in previously normotensive women. Other signs include peripheral edema, liver failure, renal failure, and HELLP syndrome (hemolysis, elevated liver enzymes, and low platelet counts).
Eclampsia: Preeclampsia with seizures.
Ocular. Focal retinal arteriolar spasm and narrowing, peripapillary or focal areas of retinal edema, retinal hemorrhages, exudates, nerve fiber layer infarcts, vitreous hemorrhage secondary to neovascularization, serous retinal detachments in 1% of preeclamptic and 10% of eclamptic patients, acute nonarteritic ischemic optic neuropathy, and bilateral occipital lobe infarcts (preeclampsia–eclampsia hypertensive posterior encephalopathy syndrome, or PEHPES). Differential diagnosis of PEHPES includes posterior circulation stroke, infectious cerebritis, coagulation disorder causing intracranial venous thrombosis, intracranial hemorrhage, occult tumor with secondary bleed, migraines, atypical seizure, or demyelination.
Natural History
Magnetic resonance imaging (MRI) abnormalities resolve 1 to 2 weeks after blood pressure control, at which time complete neurologic recovery can be expected.
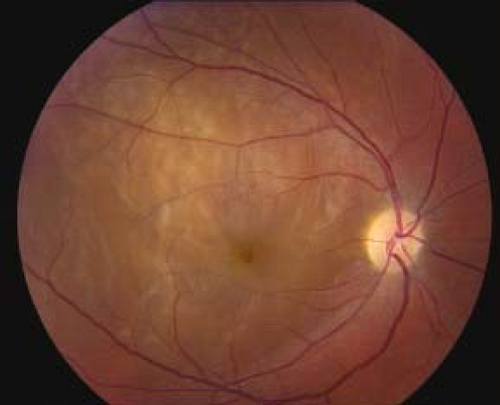
Serous retinal detachments; often bilateral and bullous; resolve postpartum with residual pigment epithelial changes (see Figure 13.3.1).
Retinal vascular changes also normalize postpartum.
Work-Up
Complete neuro-ophthalmologic and fundus examinations. Poor vision with brisk pupils without an RAPD suggests occipital lesions.
MRI findings in PEHPES include bilateral occipital lobe lesions involving subcortical white matter with possible extension into the gray-white junction, cortical surface, external capsule, and basal ganglia. MRI abnormalities are identical in obstetric and nonobstetric hypertensive encephalopathy.
With typical presentation, further invasive studies are discouraged.
Systemic work-up, including blood pressure monitoring and urinalysis, in conjunction with an obstetrics/gynecology specialist.
Occlusive Vascular Disorders
Pregnancy represents a hypercoagulable state possibly resulting in the development of retinal artery and vein occlusions, disseminated intravascular coagulopathy (DIC), and thrombotic thrombocytopenic purpura. Ocular DIC is characterized by widespread small-vessel thrombosis, particularly in the choroid, associated with hemorrhage, tissue necrosis, and serous retinal detachments.
Meningioma of Pregnancy
Meningiomas may have a very aggressive growth pattern during pregnancy that is difficult to manage. They may regress postpartum but may reoccur during subsequent pregnancies.
Other Conditions Influenced by Pregnancy
Multiple conditions can be impacted by pregnancy. SEE 3.20, PURTSCHER RETINOPATHY; 10.10, CAVERNOUS SINUS AND ASSOCIATED SYNDROMES (MULTIPLE OCULAR MOTOR NERVE PALSIES); 10.16, IDIOPATHIC INTRACRANIAL HYPERTENSION/PSEUDOTUMOR CEREBRI; 10.27, MIGRAINE; 11.12, DIABETIC RETINOPATHY; AND 11.15, CENTRAL SEROUS CHORIORETINOPATHY. Remember that medications (e.g., ophthalmic drops) deserve special attention during pregnancy.
13.4 Lyme Disease
Symptoms
Decreased vision, double vision, pain, photophobia, facial weakness. Also may have headache, malaise, fatigue, fever, chills, palpitations, or muscle/joint pains. A history of a tick bite within the previous few months may be elicited.
Signs
Ocular. Optic neuritis, vitritis, iritis, stromal keratitis, choroiditis, exudative retinal detachment, cranial nerve palsy (most often third, fourth, or sixth), bilateral optic nerve swelling, conjunctivitis, episcleritis, exposure keratopathy, and other rare abnormalities (including idiopathic orbital inflammatory syndrome). See specific sections.
Critical Systemic. One or more flat, erythematous or “bull’s-eye” skin lesions, which enlarge in all directions (erythema migrans); unilateral or bilateral facial nerve palsies; polyarticular migratory arthritis. May not be present at the time the ocular signs develop. A high serum antibody titer against Borrelia burgdorferi is often, but not always, present. Western blot testing should always be used for diagnostic confirmation.
Other Systemic. Meningitis, peripheral radiculoneuropathy, synovitis, joint effusions, cardiac abnormalities, or a low false-positive FTA-ABS titer.
Differential Diagnosis
Syphilis: High-positive FTA-ABS titer may produce a low false-positive antibody titer against B. burgdorferi. SEE 12.12, SYPHILIS.
Others: Rickettsial infections, acute rheumatic fever, juvenile idiopathic arthritis, sarcoidosis, tuberculosis, herpes virus infections, etc.
Work-Up
History: Does patient live in endemic area? Prior tick bite, skin rash, facial nerve palsy, joint or muscle pains, flu-like illness? Meningeal symptoms? Prior positive Lyme antibody test?
Complete systemic, neurologic, and ocular examinations.
Two-step diagnosis with a screening assay and confirmatory Western blot for B. burgdorferi.
Serum RPR or VDRL and FTA-ABS or treponemal-specific assay. Consider serum ACE, chest x-ray, and PPD and/or interferon-gamma release assay (IGRA) (e.g., QuantiFERON-TB Gold).
Consider lumbar puncture when meningitis is suspected or neurologic signs or symptoms are present.
Treatment
Early Lyme Disease (Including Lyme-Related Uveitis, Keratitis, or Facial Nerve Palsy)
Doxycycline 100 mg p.o. b.i.d. for 10 to 21 days.
In children, pregnant women, and others who cannot take doxycycline, substitute amoxicillin 500 mg p.o. t.i.d., cefuroxime axetil 500 mg p.o. b.i.d., clarithromycin 500 mg p.o. b.i.d., or azithromycin 500 mg p.o. daily.
Patients with Neuro-ophthalmic Signs or Recurrent or Resistant Infection
Ceftriaxone 2 g intravenously daily for 2 to 3 weeks.
Alternatively, penicillin G, 20 million units intravenously daily for 2 to 3 weeks.
Follow-Up
Every 1 to 3 days until improvement is demonstrated, and then weekly until resolved.
13.5 Convergence Insufficiency
Symptoms
Eye discomfort or blurred vision from reading or near work. Most common in young adults, but may be seen in older people.
Signs
Critical. An exophoria at near in the presence of poor near-fusional convergence amplitudes, a low accommodative convergence/accommodation (AC/A) ratio, and a remote near point of convergence.
Differential Diagnosis
Uncorrected refractive error: Hyperopia or over-minused myopia.
Accommodative insufficiency (AI): Often in prepresbyopia age range from uncorrected low hyperopia or over-minused myopia. While reading, a 4-diopter base-in prism placed in front of the eye blurs the print in AI, but improves clarity in convergence insufficiency (CI). Rarely, adolescents may develop transient paresis of accommodation, requiring reading glasses or bifocals. This idiopathic condition resolves in several years.
Convergence paralysis: Acute onset of exotropia and diplopia on near fixation only; normal adduction and accommodation. Usually results from a lesion in the corpora quadrigemina or the third cranial nerve nucleus, and may be associated with Parinaud syndrome.
Etiology
Fatigue or illness.
Drugs (parasympatholytics).
Uveitis.
Adie tonic pupil.
Glasses inducing a base-out prism effect.
Postexanthematous encephalitis.
Traumatic injury.
Idiopathic.
Work-Up
Manifest (without cycloplegia) refraction.
Determine the near point of convergence: Ask patient to focus on an accommodative target (e.g., a pencil eraser) and to state when double vision develops as you bring the target toward them; a normal near point of convergence is <8 cm.
Check for exodeviations or esodeviations at distance and near using the cover tests (SEE APPENDIX 3, COVER/UNCOVER AND ALTERNATE COVER TESTS) or the Maddox rod test.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree