Purpose
To compare the outcomes of laser in situ keratomileusis (LASIK) performed with a femtosecond laser vs a mechanical microkeratome for the correction of low to moderate hyperopia.
Design
Retrospective, nonrandomized, interventional, comparative case series.
Methods
settings: Vissum Santa Hortensia, Madrid, Spain. study population and procedures: Patients who had undergone LASIK to correct their hyperopia using the 60-kHz IntraLase femtosecond laser were compared to age- and refraction-matched patients in whom the Moria M2 microkeratome was used. Visual and refractive results 3 months postoperatively were compared between both groups.
Results
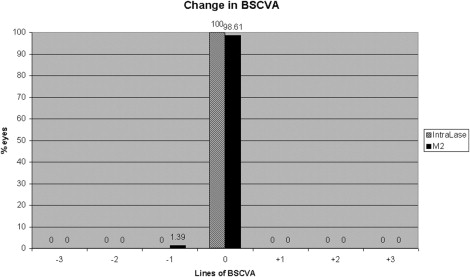
A total of 144 eyes were analyzed (72 in each group). Mean preoperative sphere was +3.45 ± 1.0 diopters (D) in the IntraLase group vs +3.18 ± 1.3 D in the M2 group ( P = .1). Results 3 months postoperatively were: mean residual sphere, +0.44 ± 0.6D vs +0.72 ± 0.8 D ( P = .02), respectively; uncorrected visual acuity (UCVA), 0.89 ± 0.2 vs 0.80 ± 0.2 ( P = .04); best spectacle-corrected visual acuity (BSCVA), 0.96 ± 0.2 vs 0.92 ± 0.2 ( P = .2); safety index, 0.97 ± 0.1 vs 0.98 ± 0.1 ( P = .5); efficacy index, 0.89 ± 0.2 vs 0.84 ± 0.2 ( P = .3).
Conclusions
Hyperopic LASIK performed with the IntraLase femtosecond laser seems to achieve better refractive results 3 months after the surgery compared to the M2 microkeratome, without significant differences in safety between both procedures.
Compared to the outcomes obtained with laser in situ keratomileusis (LASIK) for the correction of myopia, the results of this procedure for the treatment of hyperopia are not as satisfactory, mainly because of the lower range of diopters susceptible of laser correction, the greater tendency to regression, and the higher risk of loss of best spectacle-corrected visual acuity (BSCVA). Nevertheless, it is still the preferred method for correction of low to moderate hyperopia.
The femtosecond laser has been shown to create a more predictable and planar corneal flap compared with the meniscus-shaped flaps obtained with a mechanical microkeratome. It has been reported that flap creation with a femtosecond laser induces a lower change in corneal curvature compared with a mechanical microkeratome flap, and that the change in corneal biomechanics is more predictable and more strongly correlated to the ablation depth after a femtosecond laser flap than after a mechanical microkeratome flap. These differences between the characteristics of the flaps obtained with both technologies may have some influence on the refractive and visual outcomes of the surgical procedure, especially when correcting hyperopia, but we could not find in the literature any study specifically designed to compare both techniques in the treatment of this refractive error.
Therefore, we decided to compare the outcomes of LASIK performed with a femtosecond laser or a mechanical microkeratome for the correction of low to moderate hyperopia.
Patients and Methods
We performed a retrospective study of consecutive patients who had undergone LASIK to correct their hyperopic error in our institution. Patients who had undergone LASIK using the 60-kHz IntraLase FS laser (IntraLase Corp, Irvine, California, USA)—IntraLase group—were compared to age- and refraction-matched patients in whom the Moria M2 microkeratome (Moria SA, Antony, France) was used to create the flap (M2 group). For this study, we excluded patients in whom the difference between manifest refraction and cycloplegic refraction was higher than 1 diopter (D). In all patients the laser was programmed to correct their full cycloplegic refraction. Once the characteristics of mechanical microkeratome and femtosecond laser flap creation were explained to the patients, they freely chose between one and the other technique.
When evaluating for surgery, we excluded patients with unstable refraction, previous ocular surgery (refractive or other surgical procedures), suspicion of keratoconus, ocular disease, and systemic diseases that could alter the wound-healing process such as diabetes and connective tissue disorders. All study patients had a full ophthalmologic examination preoperatively that included measurement of uncorrected visual acuity (UCVA); BSCVA, including manifest and cycloplegic refractions; slit-lamp biomicroscopy; tonometry (CT-80; Topcon, Tokyo, Japan); corneal pachymetry (DGH 5100 contact pachymeter; DGH Technology, Inc, Exton, Pennsylvania, USA); keratometry and corneal topography (CSO; Compagnia Strumenti Oftalmici, Firenze, Italy); mesopic pupil measurement (Colvard pupillometer; Oasis, Glendora, California, USA); and funduscopy.
Surgical Technique
Two surgeons (M.A.T., L.B.L.) performed all the procedures. A 5% povidone-iodine solution was applied to the skin and the conjunctiva, and a sterile surgical drape and a rigid eyelid speculum were positioned. Surgery was performed using topical anesthesia with lidocaine 2%.
In the M2 group, the Moria M2 microkeratome was used to create the flap. The suction rings (+2, +1, 0, or −1) and the cutting heads (90 μm, 110 μm, or 130 μm) were selected depending on the preoperative corneal curvature and following the manufacturer’s nomogram. In the IntraLase group, the 60-kHz IntraLase was used to create the flap, using the following parameters: raster pattern, a bed energy level of 0.90 μJ, a side-cut energy of 0.90 μJ, a spot separation of 7 μm, a 70-degree side cut, a hinge angle of 50 degrees, an attempted flap depth of 120 μm, and a flap diameter of 9 mm.
In both groups, once the flap was created with either method, it was raised with a spatula, the stromal bed was dried with a sponge, and the ablation was performed using the Esiris Schwind excimer laser (Schwind Eye Tech Solutions, Kleinostheim, Germany) using a conventional treatment algorithm. We used the same nomogram for both groups. The stroma was then rinsed with balanced salt solution and the flap was gently put back in place with a cannula. Antibiotic drops (ofloxacin 3 mg/mL) and nonsteroidal anti-inflammatory drops (ketorolac trometamol 5 mg/mL) were applied.
Postoperative Follow-Up
Postoperatively, all patients used preservative-free artificial tears as needed and were instructed to apply topical antibiotic drops (ofloxacin 3 mg/mL) 4 times daily for 1 week. Steroid drops (dexamethasone alcohol 1 mg/mL) were used 4 times daily in the M2 group and 8 times daily in the IntraLase group during the first postoperative week, based on the expected higher risk of diffuse lamellar keratitis (DLK) after femtosecond laser surgery reported in the literature.
Routine clinical examinations were performed at 1 day, 1 week, and 3 months postoperatively. Visual and refractive results 3 months postoperatively were compared between both groups.
Statistical Analysis
Statistical analysis was performed using the Statview SE + Graphics software (Abacus Concepts Inc., Piscataway, New Jersey, USA). Statistical comparisons were done with the unpaired 2-tailed Student t test . P ≤ .05 was considered statistically significant. Visual acuity was converted to logarithm of the minimal angle of resolution (logMAR) from the decimal notation for statistical analysis, using a visual acuity conversion chart. Continuous data are expressed as the mean ± standard deviation.
Results
One hundred and forty-four eyes (72 eyes in each group) were included in the study. Preoperative data are shown in Table 1 . There were no statistically significant differences between both groups preoperatively.
| IntraLase (n = 72) | M2 (n = 72) | P Value | |
|---|---|---|---|
| Age (years) | 37.7 ± 8.5 (18 to 53) | 39.2 ± 10.2 (18 to 56) | .3 |
| Preop sphere (D) | +3.45 ± 1.0 (+1.00 to +6.25) | +3.18 ± 1.3 (+1.25 to +6.50) | .1 |
| Preop cylinder (D) | −2.0 ± 1.5 (0 to −5.25) | −1.28 ± 1.5 (0 to −5.50) | .1 |
| Preop spherical equivalent (D) | +2.45 ± 1 (+0.12 to +4.25) | +2.54 ± 1.1 (+0.87 to +5.00) | .6 |
| Preop BSCVA (decimal notation) | 0.98 ± 0.2 (0.25 to 1.25) | 0.94 ± 0.2 (0.15 to 1.25) | .6 |
| Optical zone (mm) | 6.1 ± 0.6 (6 to 6.5) | 6.1 ± 0.3 (6 to 7.5) | .1 |
The postoperative UCVA ( Figure 1 ) was significantly better in the IntraLase group 3 months after surgery, with no significant differences in the previous visits. Despite this difference, the efficacy index, although slightly higher in the IntraLase group, did not reach statistical significance ( Table 2 ). Table 2 shows the visual and refractive results 3 months after surgery in both groups. The residual refractive error was in both groups slightly hyperopic, but it was statistically significantly lower in the IntraLase group. The tendency to undercorrection in the M2 group is more clearly appreciated in Figure 2 : none of the 72 eyes in the IntraLase group vs 5 of the 72 eyes (6.94%) in the M2 group showed residual spherical equivalent equal or higher than +2.00 D. Fifty-three eyes (73.6%) after IntraLase compared to 43 eyes (59.7%) in the M2 group were within 0.50 D of emmetropia. Sixty-seven eyes (93.0%) and 58 eyes (80.5%), respectively, were within 1.00 D of emmetropia 3 months after the surgery.
| IntraLase (n = 72) | M2 (n = 72) | P | |
|---|---|---|---|
| Sphere (D) | +0.44 ± 0.6 (−0.25 to +2.5) | +0.72 ± 0.8 (0 to +2.75) | .02 c |
| Cylinder (D) | −0.41 ± 0.5 (0 to −2.50) | −0.31 ± 0.5 (0 to −2.75) | .3 |
| Spherical equivalent (D) | +0.24 ± 0.4 (−0.62 to +1.75) | +0.57 ± 0.7 (−0.37 to +2.75) | .002 c |
| UCVA (decimal notation) | 0.89 ± 0.2 (0.15 to 1.25) | 0.80 ± 0.2 (0.05 to 1.25) | .04 c |
| BSCVA (decimal notation) | 0.96 ± 0.2 (0.15 to 1.25) | 0.92 ± 0.2 (0.15 to 1.25) | .2 |
| Safety index a | 0.97 ± 0.1 | 0.98 ± 0.1 | .5 |
| Efficacy index b | 0.89 ± 0.2 | 0.84 ± 0.2 | .3 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


