 Eyelid Miscellaneous Conditions Simulating Neoplasms
Eyelid Miscellaneous Conditions Simulating NeoplasmsEyelid Amyloidosis
General Considerations
There are several tumors and pseudotumors that are difficult to classify. Examples discussed in this chapter include amyloidosis, lipoid proteinosis, granular cell tumor, malakoplakia, calcinosis cutis, and phakomatous choristoma.
Amyloidosis is characterized by deposition of a variety of abnormal proteins in many parts of the body. The eyelid is a preferred site in patients with primary systemic amyloidosis (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19). There is a frequent association of eyelid amyloidosis and multiple myeloma.
Clinical Features
Eyelid involvement typically appears as multiple bilateral confluent papules that have a waxy pink or yellow color. The lesions tend to bleed spontaneously or following slight trauma. In many cases, there is blepharoptosis and thickening of the eyelid owing to diffuse involvement of the palpebral conjunctiva (10,13). In most instances, bilateral eyelid amyloidosis is associated with systemic amyloidosis, but amyloid deposition can also occur as an isolated phenomenon on the eyelids (9,14).
Pathology
Management
Treatment of eyelid amyloidosis is controversial and difficult and should be directed toward the symptoms. Some lesions apparently remain stable for months and require no active treatment (15). Surgical excision of larger, cosmetically unacceptable eyelid lesions is appropriate (18). Some surgeons have reported successful removal of eyelid amyloid by meticulous dissection, leaving the anatomic planes of the eyelid intact (11). Although controversial, irradiation has been reported to cause regression of the lesions (8).
Selected References
1. Finer JT, Wigs JL, Jakobiec FA. Eyelid manifestations of systemic disease. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology. 2nd ed. Philadelphia: WB Saunders; 2000:4984-4994.
2. Chotzen VA, Kenyon KR. Amyloidosis. In: Mannis MJ, Macsai MS, Huntley AC, eds. Eye and Skin Disease. Philadelphia: Lippincott-Raven; 1996: 71-77.
3. Font RL. Eyelids and lacrimal drainage system. In: Spencer WH, ed. Ophthalmic Pathology. An Atlas and Textbook. 4th ed. Philadelphia: WB Saunders; 1996:2367-2370.
4. Smith ME, Zimmerman LE. Amyloidosis of the eyelid and conjunctiva. Arch Ophthalmol 1966;75:42-50.
5. Natelson EA, Duncan WC, Macossay C, et al. Amyloidosis palbebrum. Arch Intern Med 1979;125:304-305.
6. Halasa AH. Amyloid disease of the eyelid and conjunctiva. Arch Ophthalmol 1965;74:298-301.
7. Brownstein MH, Elliott R, Helwig EB. Ophthalmologic aspects of amyloidosis. Am J Ophthalmol 1970;69:423-430.
8. Pecora JL, Sambursky JS, Vargha Z. Radiation therapy in amyloidosis of the eyelid and conjunctiva: a case report. Ann Ophthalmol 1982;14:194-196.
9. Fett DR, Putterman AM. Primary localized amyloidosis presenting as an eyelid margin tumor. Arch Ophthalmol 1986;104:584-585.
10. Iijima S. Primary systemic amyloidosis: a unique case complaining of diffuse eyelid swelling and conjunctival involvement. J Dermatol 1992;19:113-118.
11. Patrinely JR, Koch DD. Surgical management of advanced ocular adnexal amyloidosis. Arch Ophthalmol 1992;110:882-885.
12. Olsen KE, Sandgren O, Sletten K, et al. Primary localized amyloidosis of the eyelid: two cases of immunoglobulin light chain-derived proteins, subtype lambda V respectively lambda VI. Clin Exp Immunol 1996;106:362-366.
13. Hill VE, Brownstein S, Jordan DR. Ptosis secondary to amyloidosis of the tarsal conjunctiva and tarsus. Am J Ophthalmol 1997;123:852-854.
14. Pelton RW, Desmond BP, Mamalis N, et al. Nodular cutaneous amyloid tumors of the eyelids in the absence of systemic amyloidosis. Ophthalmic Surg Lasers 2001;32:422-424.
15. Rodrigues G, Sanghvi V, Lala M. A rare cause of unilateral upper and lower eyelid swelling: isolated conjunctival amyloidosis. Korean J Ophthalmol. 2001;15:38-40.
16. Goldstein DA, Schteingart MT, Birnbaum AD, et al. Bilateral eyelid ecchymosis and corneal crystals: an unusual presentation of multiple myeloma. Cornea 2005;24:757-758.
17. Landa G, Aloni E, Milshtein A, et al. Lid bleeding and atypical amyloidosis. Am J Ophthalmol 2004;138:495-496.
18. Stack RR, Vote BJ, Evans JL, et al. Bilateral ptosis caused by localized superficial eyelid amyloidosis. Ophthalmol Plast Reconstr Surg 2003;19: 239-240.
19. Brownstein MH, Elliott R, Helwig EB. Ophthalmologic aspects of amyloidosis. Am J Ophthalmol 1970;69:423-430.
Eyelid Amyloidosis
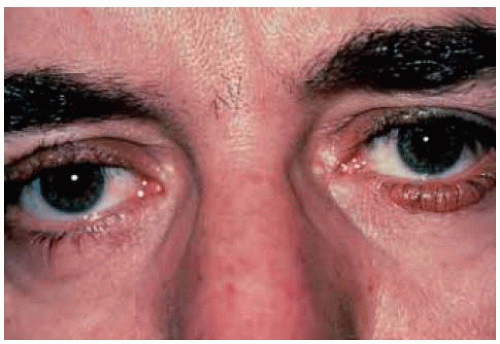
 Figure 13.2. Eyelid amyloidosis in a 59-year-old man with multiple myeloma. (Courtesy of Myron Yanoff, MD.) |
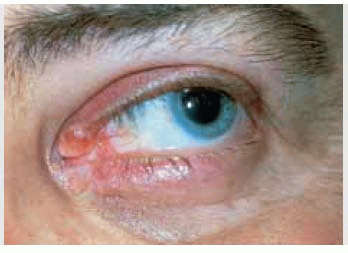
 Figure 13.4. Closer view of lesion on left lower eyelid in patient shown in Figure 13.3. (Courtesy of David Barsky, MD, and Thomas Spoor, MD.) |
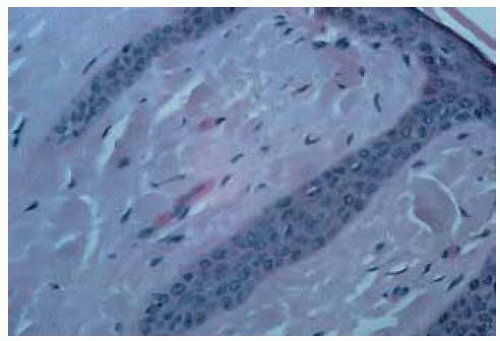 Figure 13.5. Photomicrograph of lesion shown in Figure 13.3 showing relatively acellular lightly eosinophilic material in the derm is. (Hematoxylin-eosin 25.) (Courtesy of David Barsky, MD, and Thomas Spoor, MD.) |
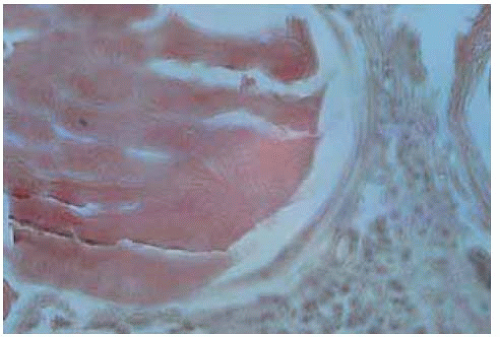 Figure 13.6. Photomicrograph of lesion shown in Figure 13.3 showing positive reaction to Congo Red. (Congo red 25.) (Courtesy of David Barsky, MD, and Thomas Spoor, MD.) |
Eyelid Lipoid Proteinosis (Urbach-Wiethe Disease)
General Considerations
Lipoid proteinosis (Urbach-Wiethe disease) is an uncommon autosomal-recessive condition characterized by numerous beaded papules and nodules that develop in the skin and mucous membranes and bilateral sickle-shaped skull calcifications on imaging studies (1,2,3,4,5,6,7,8,9,10,11,12). The eyelid lesions can occur in siblings and are believed to be pathognomonic (10).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree