Eyelid Melanocytic Tumors
Eyelid Melanocytic TumorsEyelid Melanocytic Nevus
General Considerations
Melanocytic nevus (1,2,3,4,5,6,7,8) consists of melanocytes derived from the neural crest that migrate to the skin during embryonic development (1,2). An eyelid nevus can be acquired or congenital. The acquired type begins in childhood in the basal epithelium (junctional nevus), gradually migrates into the dermis in young adults (compound nevus), and later in life resides entirely in the dermis (dermal nevus). The average young adult has about 15 cutaneous nevi and the eyelid is occasionally affected (2). Multiple nevi should raise suspicion of the dysplastic nevus syndrome, in which there is a familial tendency toward development of cutaneous melanoma (2).
Clinical Features
The clinical features vary with patient age and stage of the disease. It usually appears between ages 5 and 15 years as a small macule that gradually evolves through the stages listed above. Eyelid nevus can range from deeply pigmented to amelanotic. An eyelid margin nevus can extend onto the palpebral conjunctiva. It can surround the lacrimal punctum (peripunctal nevus; 3). The surface can be smooth or verrucous (3,4). It does not generally produce loss of cilia. A variant of congenital nevus is deeply pigmented and larger than an acquired nevus (2). It is slightly elevated and frequently has excess hairs. As opposed to the junctional nevus, this lesion has a greater chance of malignant transformation, perhaps as high as 5% (2,8). A variant of congenital nevus is the divided nevus of the upper and lower eyelids (“kissing nevus”) that develops before embryologic separation of the eyelid and divides when the eyelids separate.
Pathology
Melanocytic nevi are divided into junctional, compound, and intradermal types (1,2). These are not entirely separate categories, but rather represent stages in the “life cycle” of nevus, as discussed above.
The diagnosis of nevus is often made by the arrangement of its cells in nests rather than by cellular characteristics (2). A junctional nevus has well-circumscribed nests of cells at the basal level of the epidermis. A compound nevus possesses features of both a junctional and an intradermal nevus. It can have considerable fibrous tissue and may resemble a neurofibroma or other neural tumors.
Management
Cutaneous nevi on the trunk and extremities are frequently excised because of their malignant potential. There is a greater tendency to observe those on the eyelid until growth is documented, partly because of cosmetic considerations. Management is generally periodic observation, with excision of more suspicious lesions. If the lesion is superficial, an elliptical resection is recommended. If it is present on the eyelid margin only, it can be shaved parallel to the eyelid margin. More extensive tumors require anterior lamellar or full-thickness eyelid resection (7).
Some congenital nevi can occasionally involve most of the eyelid area and their management is complex. The clinician must weigh the chances of malignant transformation with the consequences of radical removal and cosmetic surgery.
Selected References
1. Font RL. Eyelids and lacrimal drainage system. In: Spencer WH, ed. Ophthalmic Pathology. An Atlas and Textbook. 4th ed. Philadelphia: WB Saunders; 1996:2263-2270.
2. Elder D, Elenitsas R. Benign pigmented lesions and malignant melanoma. In: Elder D, Elenitsas R, Jaworsky C, et al., eds. Lever’s Histopathology of the Skin. 8th ed. Philadelphia: Lippincott-Raven; 1997:633-640.
3. Scott KR, Jakobiec FA, Font RL. Peripunctal melanocytic nevi. Distinctive clinical findings and differential diagnosis. Ophthalmology 1989;96:994-998.
4. Putterman AM. Intradermal nevi of the eyelid. Ophthalmic Surg 1980;11: 584-587.
5. McDonnell PJ, Mayou BJ. Congenital divided naevus of the eyelids. Br J Ophthalmol 1988;72:198-201.
6. Margo CE, Habal MB. Large congenital melanocytic nevus. Light and electron microscopic findings. Ophthalmology 1987;94:9760-9765.
7. Margo CE, Rabinowicz IM, Hagal MB. Periocular congenital melanocytic nevi. J Pediatr Ophthalmol Strabismus 1986;23:222-226.
8. Lorentzen M, Pers M, Bretteville-Jenssen G. The incidence of malignant transformation in giant pigmented nevi. Scand J Plast Reconstr Surg 1977;11:163.
Eyelid Melanocytic Nevus: Pigmented Types
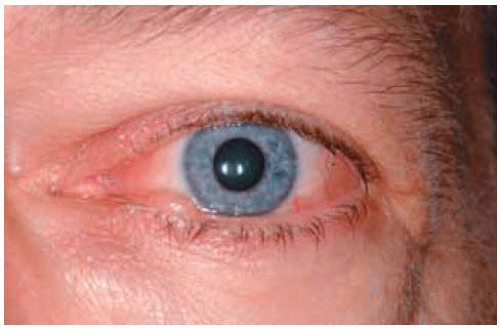
Many acquired nevi become clinically apparent in childhood and remain relatively dormant for the remainder of the patient’s life. Examples are shown of flat and minimally elevated lesions on eyelid margin.
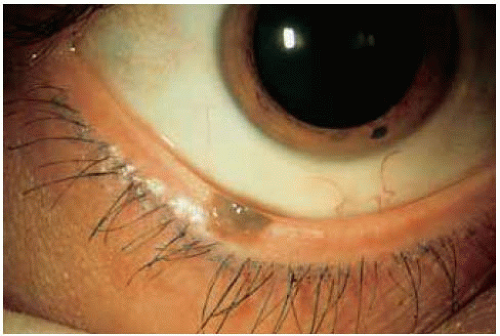
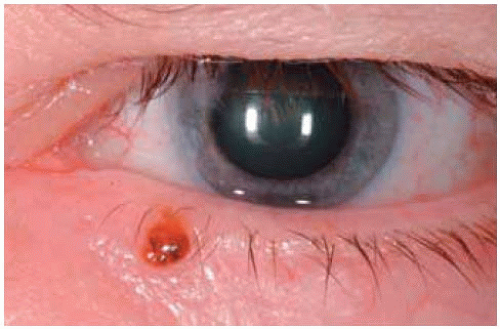
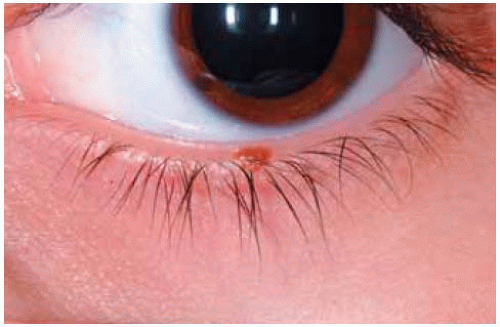 Figure 6.1. Small pigmented melanocytic nevus of left lower eyelid of a child. Note that this benign lesion has not caused loss of cilia. |
Eyelid Melanocytic Nevus: Age and Race Variations
Although it is classically found in Caucasians in the first decade of life, eyelid nevus can be initially diagnosed at any age and in patients of any race.
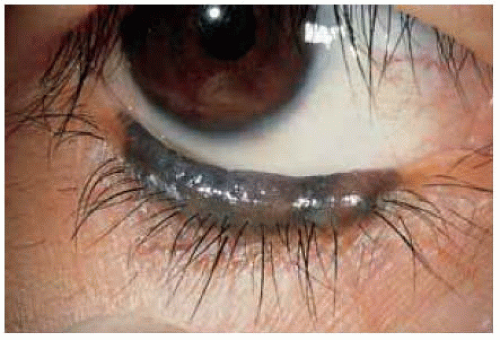
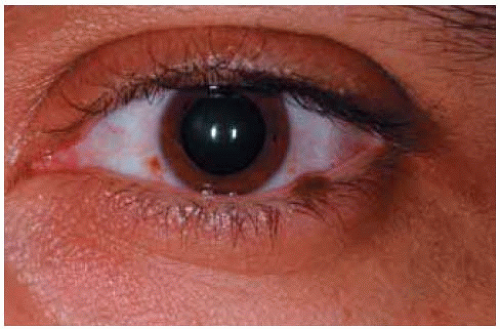 Figure 6.10. Eyelid margin nevus in Middle Eastern man. Note the complexion-related melanosis of conjunctiva, best seen near the limbus. |
 Figure 6.11. Slightly pedunculated eyelid margin nevus in an African American man. Note again the complexion-related melanosis of the conjunctiva. |
Eyelid Melanocytic Nevus: Nonpigmented Types
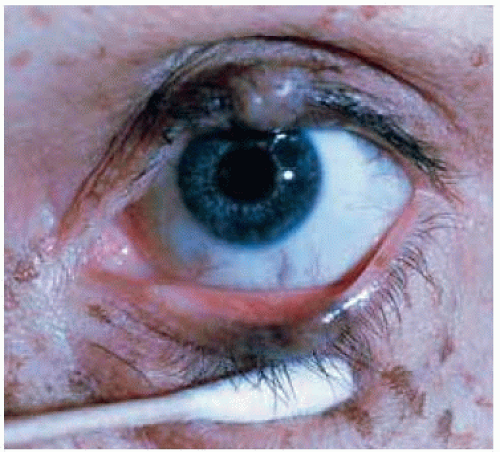
An eyelid nevus can be nonpigmented, thus resembling a papilloma, basal cell carcinoma, or other amelanotic lesion.
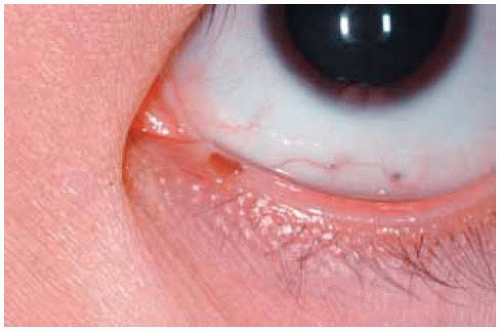
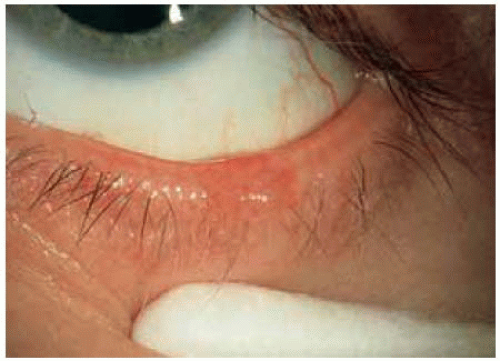 Figure 6.14. Lesion seen in Figure 6.13, with slight eversion of the eyelid, showing that it extends around the eyelid margin to the palpebral conjunctiva. |
 Figure 6.15. Slightly vascular nonpigmented melanocytic nevus of lower eyelid. Such a lesion may be difficult to differentiate clinically from sessile papilloma or nodular basal cell carcinoma. |
 Figure 6.16. Nonpigmented melanocytic nevus of upper eyelid associated with slight loss of cilia in a 59-year-old woman. Such a lesion can resemble basal cell carcinoma. |
 Figure 6.18. Closer view of lesion shown in Figure 6.17. |
Eyelid Melanocytic Nevus: Clinical Variations of Nonpigmented Type
In some instances, typical eyelid margin nevus can be associated with loss of cilia. It can sometimes be first recognized in middle-aged or older patients.
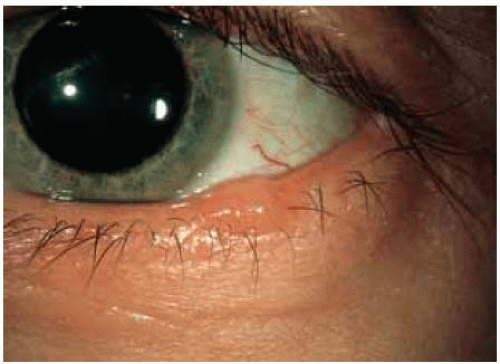
 Figure 6.20. Minimally pigmented, slightly vascular lesion on left lower eyelid. Note the sparsity of cilia near the base of the lesion. |
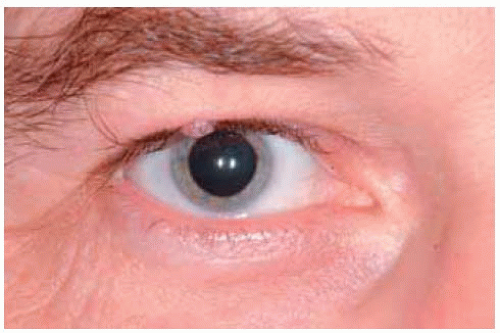 Figure 6.21. Nevus of right upper eyelid margin in adult man. As in the other cases, there is sparsity of cilia in the lesion. |
 Figure 6.22. Patient shown in Figure 6.21, looking down. Note again the sparsity of cilia. |
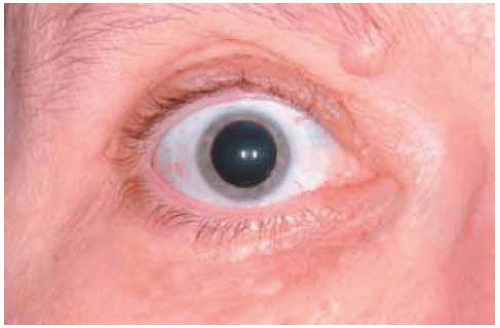 Figure 6.23. Infrabrow nevus in a middle-aged woman. Note the single hair protruding from the lesion. |
Eyelid Melanocytic Nevus: Excision Technique and Pathology of Small Lesions
Suspicious or growing lesions near the eyelid margin can be removed by an elliptical or shaving technique. These methods are illustrated in Chapter 15.
 Figure 6.25. Melanocytic nevus of skin of lower eyelid of a 69-year-old man. The lesion had slowly enlarged. |
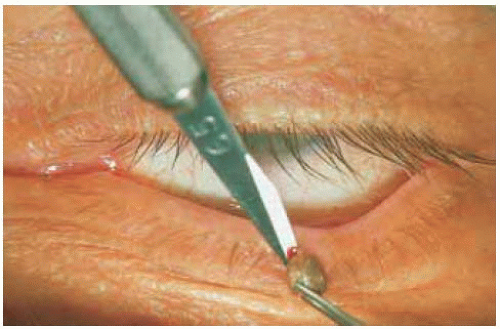 Figure 6.26. Removal of lesion in Figure 6.25 by shaving elliptical excision. The wound was closed with two vertical interrupted skin sutures. |
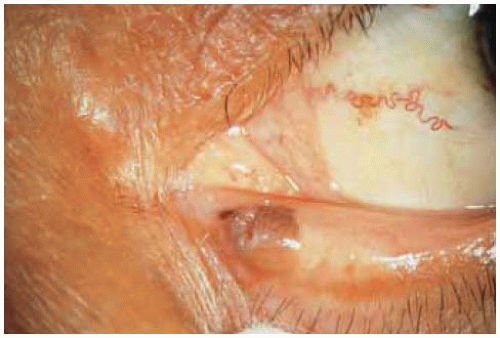
 Figure 6.27. Melanocytic nevus on margin of lower eyelid. Local anesthesia is being injected beneath the lesion through a 25-gauge needle and a protective scleral shell is in place. |
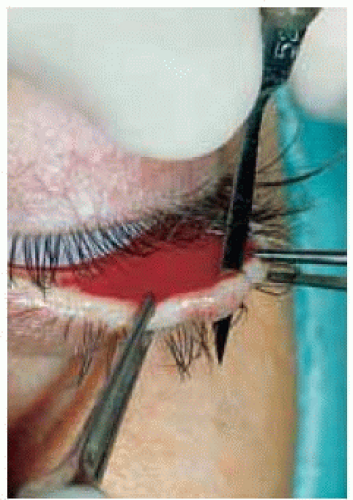 Figure 6.28. Removal of lesion in Figure 6.27 by shaving excision only. Light cautery was applied after removal. No sutures were necessary. |
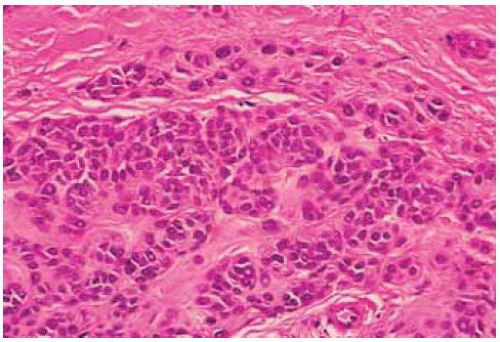
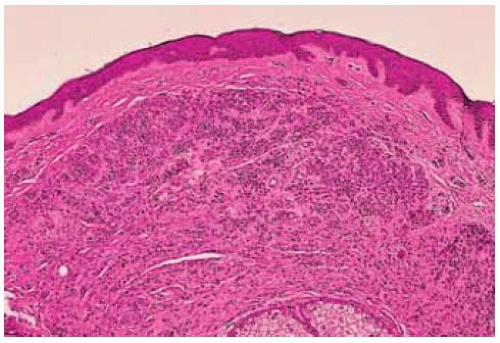 Figure 6.29. Photomicrograph showing dermal nevus. Note the confluent nests of cells in the dermis, deep to the epithelium. (Hematoxylin-eosin 50.) |
Eyelid Melanocytic Nevus: Congenital Divided (“Kissing”) Nevus
Divided nevus of the eyelid can assume any of several configurations.
Margo CE. Pigmented lesions of the eyelid. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology. Philadelphia: W B Saunders; 1994:1797-1812.
 Figure 6.32. More subtle nevus on upper eyelid of patient is shown in Figure 6.31. These upper and lower eyelid lesions touched one another when the eyelids were closed. |
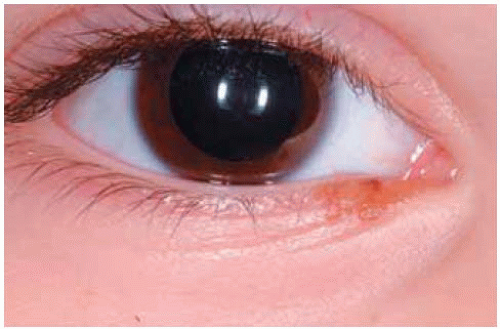
 Figure 6.33. Divided nevus involving medial aspect of eyelids. (Courtesy Armed Forces Institute of Pathology, Washington, DC.) |
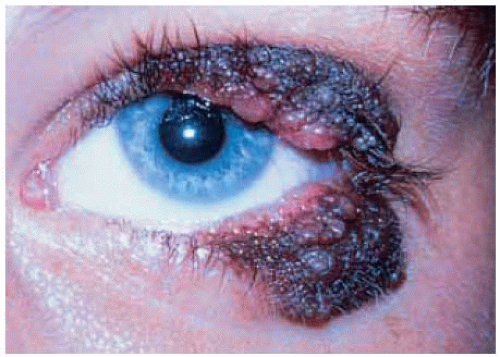 Figure 6.34. Irregular, verrucouslike divided nevus affecting lateral aspect of eyelids. (Courtesy of Curtis Margo, MD.) |
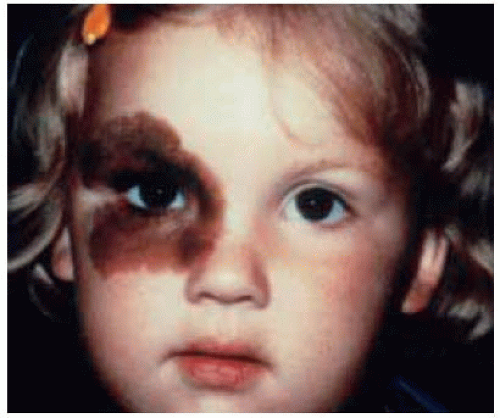
Eyelid Melanocytic Nevus: Large Congenital Periocular Type
In some instances, congenital periocular nevus can be very extensive, raising difficult management problems.
Margo CE. Pigmented lesions of the eyelid. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology. Philadelphia: W B Saunders; 1994:1797-1812.
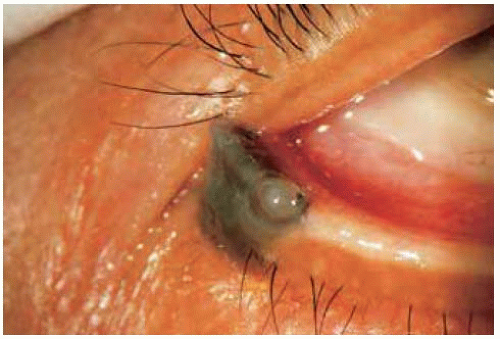
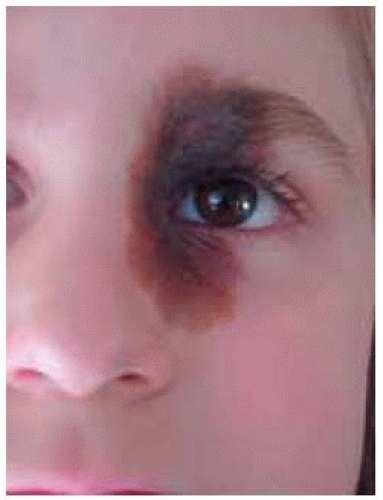 Figure 6.40. Large congenital nevus affecting both eyelids, medial canthal skin, and eyebrow. The indurated lesion was covered with hair. (Courtesy of Curtis Margo, MD.) |
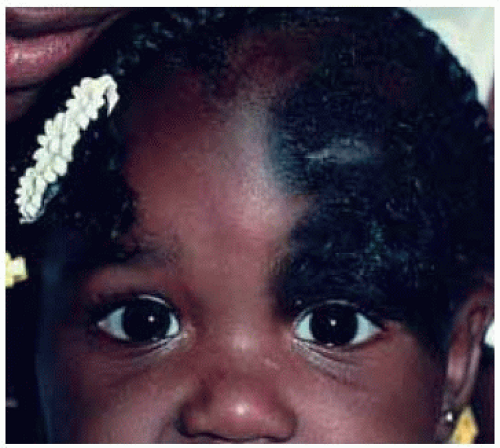 Figure 6.41. Large congenital nevus affect eyelids and scalp. The indurated lesion was covered with hair. (Courtesy of Curtis Margo, MD.) |
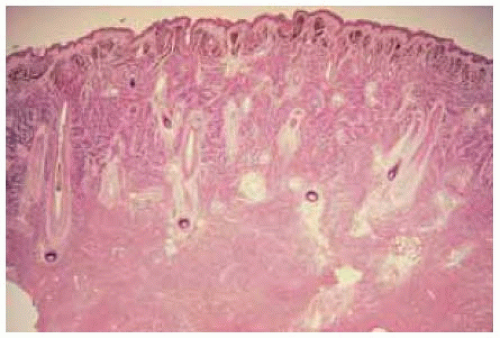 Figure 6.42. Histopathology of biopsy taken from lesion in Figure 6.41, showing heavily pigmented nests of nevus cells in the dermis. (Courtesy of Curtis Margo, MD.) |
Oculodermal Melanocytosis (Nevus of Ota)
General Considerations
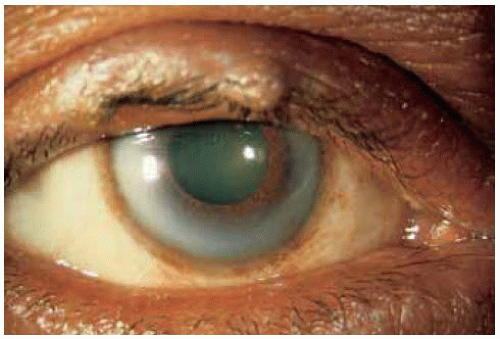
Oculodermal melanocytosis is a congenital pigmentation of periocular skin, uveal tract, and sometimes the orbit, ipsilateral meninges, and ipsilateral hard palate (1,2,3,4,5,6,7,8,9,10,11,12,13). Its incidence has been estimated to be about 0.04% in Caucasians (4). The excess melanocytes can spawn malignant melanoma of the uvea, orbit, and brain (1). Malignant transformation of the eyelid component into cutaneous melanoma is rare (2,3,4). Although oculodermal melanocytosis is generally diagnosed in Caucasians, it occurs in African Americans and Asians, in whom it is also associated with a higher incidence of uveal melanoma (9). This section on eyelid lesions considers mainly the periocular cutaneous lesion as part of the spectrum of oculodermal melanocytosis. The associated uveal melanoma is discussed in the atlas of intraocular tumors.
Clinical Features
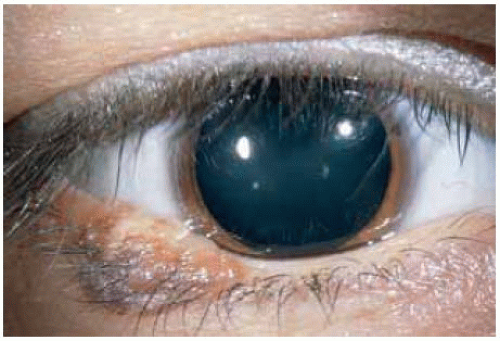
Clinically, the cutaneous lesion is a flat, tan to gray pigmentation that affects the facial and periocular skin, including the eyelids. Although it may be somewhat irregular, it tends to follow the distribution of the first and second divisions of the trigeminal nerves. It is bilateral in about 10% of cases. Interesting variations include involvement of the temporal skin and hard palate. Another association is iris mammillations, which are irregular, confluent, dome-shaped elevations on the iris surface. This can be the predominant feature when the episcleral and posterior uveal pigmentation is subtle or absent (11). Oculodermal melanocytosis can rarely occur in association with other phakomatoses, such as Sturge-Weber syndrome and phakomatosis pigmentovascularis IIa (12).
Pathology
Histopathologically, nevus of Ota is characterized by excess scattered dendritic melanocytes in the dermis. It is not as cellular as a true blue nevus.
Management
A patient with these clinical findings should be evaluated for evidence of ocular melanocytosis and undergo periodic fundus examination to detect early malignant melanoma of the uveal tract. Uveal melanoma usually occurs in adult Caucasians, but has been recognized in children (6) and African American patients (7) with congenital melanocytosis, underscoring the need to follow affected patients who would otherwise be at low risk to develop uveal melanoma. The incidence of uveal melanoma in patients with ocular or oculodermal melanocytosis is estimated to be 1:400 cases (5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree