Eyelid Lymphoid, Plasmacytic, and Metastatic Tumors
Eyelid Lymphoid, Plasmacytic, and Metastatic TumorsEyelid Lymphoma
General Considerations
The eyelids, as well as most other ocular structures, can be involved with benign and malignant lymphoid tumors (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15). The classification of extranodal lymphoid tumors in the ocular region is complex and confusing. The Revised European American Lymphoma classification is currently the most popular (4,5,11). Ophthalmic pathologists have traditionally classified lymphoid tumors into benign (lymphoid hyperplasia), intermediate, and malignant forms. Clinical differentiation of these forms is not usually possible, and biopsy and histopathologic assessment are necessary to make a specific diagnosis. Lymphoma can also be divided into Hodgkin’s and non-Hodgkin’s types and B-cell or T-cell types (cutaneous lymphoma; mycosis fungoides) depending on the type of lymphocyte that comprises most of the lesion.
Sezary syndrome is a variant of T-cell lymphoma that consists of a triad of erythroderma, leukemia, and large peripheral lymph nodes. It generally affects elderly men and is characterized by a more fulminating course. It often shows atypical mononuclear cells in the blood (Sezary cells). The skin lesions are identical clinically and histopathologically to typical mycosis fungoides and they can rarely involve the eyelids.
Eyelid lymphoid tumors tend to parallel those of the orbit in their degree of malignancy and their clinical behavior. Orbital lymphoid tumors are more common and are discussed in more detail in the Atlas of Orbital Tumors. Lymphoma can be confined to the eyelid, but is more often associated with systemic lymphoma. It is generally a disease of elderly patients, but it can occur in younger individuals, particularly those with AIDS. In contrast with conjunctival lymphoma, eyelid lymphoma tends to have a greater association with systemic lymphoma, particularly if it is bilateral (1,7).
Clinical Features
B-cell lymphoma of the eyelid generally occurs as a smooth, rather firm subcutaneous mass. Ulceration of eyelid B-cell lymphoma is rare (10). Although it may be confined to the eyelid, it is more often continuous with anterior orbital disease.
In contrast, the less common T-cell lymphoma has a tendency to affect the skin more superficially and to exhibit papules, plaques, or ulceration (mycosis fungoides). The lesions can be solitary or multiple. It can often masquerade as other conditions before the diagnosis is realized (6). A severe form of this condition, called adult T-cell leukemia/lymphoma, has recently been recognized to exhibit simultaneous involvement of the eyelid, orbit, and uveal tract (9).
Pathology
Lymphoma of the eyelids is identical histopathologically to lymphoma in other parts of the body. It is composed of abnormal lymphocytes that range from low grade to intermediate to clearly malignant. Immunohistochemical techniques and flow cytometry are necessary to categorize the specific type of lymphoma (1,8). Most eyelid lymphomas are of B-cell lineage.
Management
When either B-cell or T-cell lymphoma are suspected in the eyelid, the affected patient should usually undergo a biopsy of the lesion and study of the cells with immunohistochemistry and flow cytometry to accurately categorize the lesion. It is important that the clinician communicate with the pathologist ahead of time to ensure that the tissue is handled properly. It is often wise to send the fresh material immediately to thepathologist rather than placing it in formaldehyde. If systemic evaluation reveals more widespread lymphoma, then chemotherapy is generally given to control the systemic disease and the eyelid lesion can be followed for regression. If the disease seems to be confined to the eyelid area, then radiotherapy can be considered. The dose of irradiation can vary from 2000 cGy for benign lymphoma to 4000 cGy for malignant lymphoma (1,2,3). The prognosis varies widely with the severity of the disease.
Selected References
1. Jakobiec FA, Bilyk JR, Font RL. Orbit. In: Spencer WH, ed. Ophthalmic Pathology. An Atlas and Textbook. 4th ed. Philadelphia: WB Saunders; 1996:2686-2736.
2. Jakobiec FA, Knowles DM. An overview of ocular adnexal lymphoid tumors. Trans Am Ophthalmol Soc 1989;87:420-444.
3. Sullivan TJ, Whitehead K, Williamson R, et al. Lymphoproliferative disease of the ocular adnexa: a clinical and pathologic study with statistical analysis of 69 patients. Ophthal Plast Reconstr Surg 2005;21:177-188.
4. Lauer SA. Ocular adnexal lymphoid tumors. Curr Opin Ophthalmol 2000; 11:361-366.
5. McKelvie PA, McNab A, Francis IC, et al. Ocular adnexal lymphoproliferative disease: a series of 73 cases. Clin Exp Ophthalmol 2001;29:387-393.
6. Game JA, Davies R. Mycosis fungoides causing severe lower eyelid ulceration. Clin Exp Ophthalmol 2002;30:369-371.
7. Jenkins C, Rose GE, Bunce C, et al. Clinical features associated with survival of patients with lymphoma of the ocular adnexa. Eye 2003;17:809-820.
8. Sharara N, Holden JT, Wojno TH, et al. Ocular adnexal lymphoid proliferations: clinical, histologic, flow cytometric, and molecular analysis of forty-three cases. Ophthalmology 2003;110:1245-1254.
9. Mori A, Deguchi HE, Mishima K, et al. A case of uveal, palpebral, and orbital invasions in adult T-Cell leukemia. Jpn J Ophthalmol 2003;47:599-602.
10. Huerva V, Canto LM, Marti M. Primary diffuse large B-cell lymphoma of the lower eyelid. Ophthal Plast Reconstr Surg 2003;19:160-161.
11. Coupland SE, Krause L, Delecluse HJ, et al. Lymphoproliferative lesions of the ocular adnexa. Analysis of 112 cases. Ophthalmology 1998;105: 1430-1441.
12. Ostler HB, Maibach HI, Hoke AW, et al. Hematological disorders. In: Diseases of the Skin and the Eye. Philadelphia: Lippincott Williams & Wilkins; 2004:211.
13. Lugassy G, Rozenbaum D, Lifshitz L, et al. Primary lymphoplasmacytoma of the conjunctiva. Eye 1992;6:326-327.
14. Onesti MG, Mazzocchi M, De Leo A, et al. T-cell lymphoma presenting as a rapidly enlarging tumor on the lower eyelid. Acta Chir Plast 2005;47:65-66.
15. Ing E, Hsieh E, Macdonald D. Cutaneous T-cell lymphoma with bilateral full thickness eyelid ulceration. Can J Ophthalmol 2005;40:467-468.
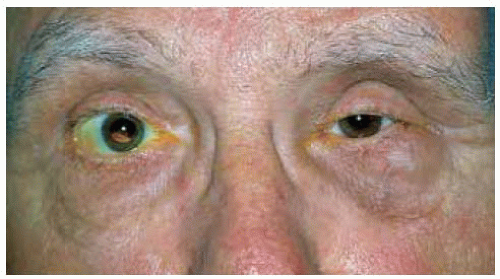
Eyelid Involvement: B-Cell Lymphoma
 Figure 9.5. B-cell lym phom a of eyelid margin in 62-year-old man. (Courtesy of Zeynel Karcioglu, MD.) |
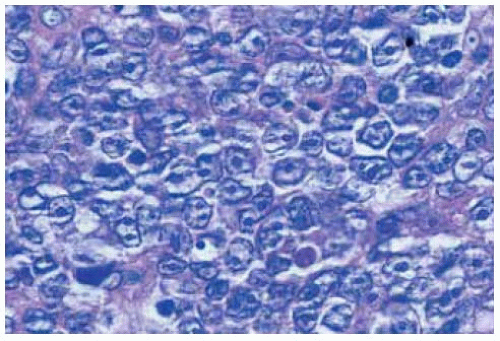 Figure 9.6. Histopathology of lesion shown in Figure 9.5. Note the large malignant lymphocytes. (Hematoxylin-eosin 200.) (Courtesy of Zeynel Karcioglu, MD.) |
Eyelid Involvement: B-Cell Lymphoma
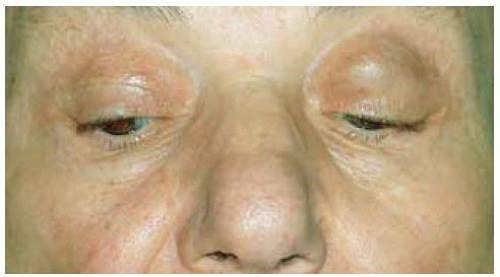
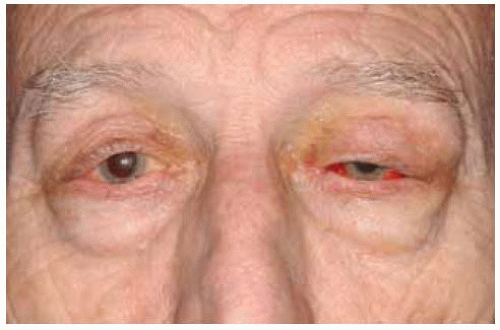 Figure 9.7. Blepharoptosis of left upper eyelid owing to deep eyelid involvement by lymphoma. The hemorrhage was due to prior biopsy to confirm the diagnosis. |
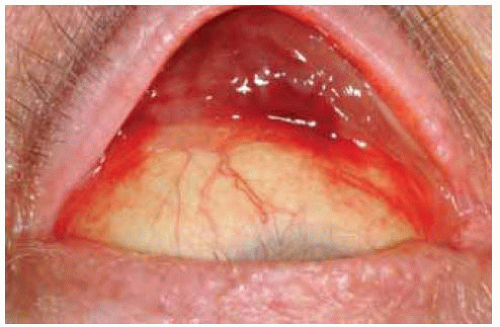 Figure 9.8. Elevation of eyelid in patient shown in Figure 9.7 reveals infiltration of palpebral conjunctiva by the neoplasm. |
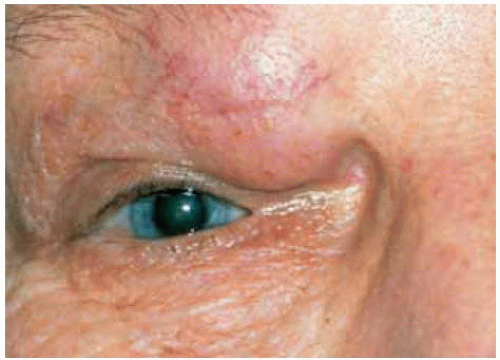
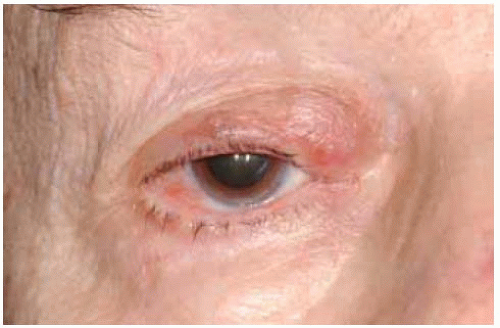 Figure 9.10. Close up view of lesion shown in Figure 9.9. |
 Figure 9.12. Close up view of lesion shown in Figure 9.11.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|