Eyebrows, Eyelids, and Face: Structure and Function
Weerawan Chokthaweesak
Christine C. Annunziata
Bobby S. Korn
Don O. Kikkawa
Eyebrows and Forehead
Structure
The eyebrows form a critical landmark of the upper facial appearance and provide a unique quality in human facial anatomy.1 Brow position and contour convey emotion and feeling and comprise an important part of body language.2,3,4
At the junction of the forehead and the upper eyelid, the eyebrow is a transverse elevation of hair arched above the superior orbital rim. Technically, the eyebrow is considered part of the scalp and is divided into three anatomic parts: head, body, and tail. The eyebrows are formed by the superciliary ridge (brow ridge or supraorbital ridge) of the frontal bone, which is more prominent in males and often absent or less prominent in females. The lateral brow lacks this extra bony support, because the superciliary ridge extends only over the medial half to two-thirds of the orbit. Laterally, the brow is supported by fascial attachments to the temporalis fascia.
The skin of the eyebrow represents a transition zone between the thinner skin of the eyelids and the thicker skin of the forehead and scalp. The eyebrow skin is thick with a correspondingly thick subcutaneous fibrofatty layer such as that of the scalp, and it consists of more fibrous tissue than fat.
The two eyebrows are mirror images of each other. Eyebrow cilia are directed at different angles in the upper and lower eyebrow.5 The upper rows grow down and laterally at an angle of <30 degrees from the vertical, whereas the lower most cilia grow up and laterally, also at an angle of <30 degrees. An abrupt reversal occurs when these cilia meet in the midline of the eyebrow. However, this reversal does not occur at the medial end of the eyebrow, where the eyebrow cilia sweep superolaterally.
The three types of hair in the eyebrow are (a) fine, vellus hair; (b) the slightly larger and lightly pigmented hair; and (c) the large terminal hair, also known as the supercilia. The fine vellus hairs form an effective moisture barrier to keep sweat from running downward into the eye. The fluid flow is redirected medially and laterally, away from the eye.
The supercilia give the eyebrow its apparent color and configuration. The supercilia are too large and too widely spaced to comprise a good moisture barrier. The horizontal and vertical eyebrow hair angulation should be kept in mind while planning incisions in the eyebrow region. Beveling the incision in a parallel fashion to the shafts of the hair will minimize the number of follicles transected.5 A rich vascular plexus and abundant sensory nerve endings surround the follicle of each supercilium. Shaving or cutting the eyebrow hair does not affect its subsequent growth. In fact, full regrowth of a shaven eyebrow occurs within 6 months.6
The skin of the eyebrow and glabellar region contains numerous sebaceous glands. Eccrine sweat glands are sparse, except for in the tail of the brow. This predominance of sebaceous glands causes an oily skin texture of the eyebrow.
The male and female eyebrows differ in both shape and position.7,8 Male brows have a flat contour with more prominence and fullness laterally and a feathered appearance at the superior margin. Eyebrow hairs tend to get thicker and longer with age. The eyebrow hair in an elderly man is heavier and thicker than in an elderly woman. The female brow tends to be thinner and more arched than the male brow. Typically, the highest point generally occurs at the junction of the body and tail of the eyebrow, which is above the lateral limbus according to Westmore’s classic model.9 Westmore also proposed that the medial extent of the eyebrow should reach a vertical line drawn from the medial canthus, and a tangential line connecting the lateral canthus and the lateral ala of the nose for the lateral extent of the eyebrow. The lateral and medial extent of the eyebrow should fall in the same horizontal plane. Cook et al.10 contend that the arch above the lateral limbus makes the face look surprised and is unnatural. They concluded that the highest arch should lie more laterally in between the lateral limbus and lateral canthus. Several recent studies support this concept.7,11 The female brow has a smoother superior margin of brow hair and rests above the orbital rim, especially in its temporal aspect. The male brow usually rests lower along the edge of the superior orbital rim.8
The eyebrow corresponds to a specialized area of the superficial muscle plane of the face where the vertical fibers of the frontalis muscle and the horizontal fibers of the orbicularis oculi muscles interdigitate.12 The position of the eyebrow represents a dynamic interplay between elevating and depressing forces.13 The frontalis muscle is the main eyebrow elevator or retractor, and the depressors or protractors are the orbicularis oculi, corrugator supercilii, and the procerus
Eyebrow Depressors
Orbicularis oculi muscle.
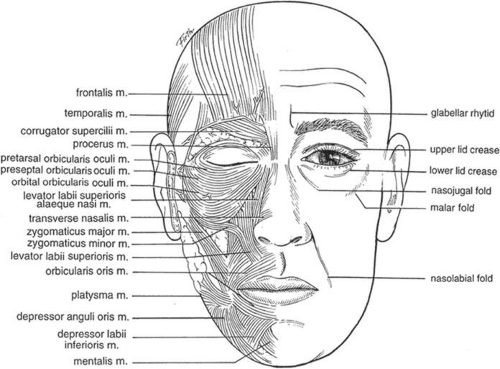
Contraction of the orbicularis oculi muscle closes the eye and pulls the eyebrow down (Fig. 1.1).
Corrugator supercilii muscle
The corrugator supercilii muscle is composed of two heads (Fig. 1.1). The transverse head originates from the frontal bone near the superomedial orbital rim, anterior and slightly superior to the trochlea. It runs obliquely in a lateral and superior direction and inserts into the subcutaneous tissue superior to the middle third of the eyebrow,13,14 The more medial oblique head of the corrugator muscle is smaller and has vertically oriented fibers that insert into the medial brow. The transition between the transverse and oblique head fibers is indistinct.14 The frontal branch of the temporal division of the facial nerve (corrugator motor nerve) supplies the transverse head of the corrugator muscle, whereas the zygomatic branch of the facial nerve innervates the oblique head.14,15 Stimulation of the transverse head moves the eyebrow medially and pulls the two eyebrows together, making the vertical and oblique furrows of the glabella. The oblique head of the corrugator acts as a depressor of the medial eyebrow and contributes to the formation of the oblique glabellar furrow. Weakening the medial portion of the corrugator contributes to medial brow elevation and can diminish glabellar frown lines.
Procerus muscle
A midline muscle overlying the glabella, the procerus muscle (Fig. 1.1) arises from the nasal bone and the upper nasal cartilage, and travels superiorly to insert on the medial forehead skin.15 Activation of these muscle fibers pulls the head of the brow inferiorly, causing the horizontal furrow of the glabella. The procerus muscle has innervations from the buccal branch of the facial nerve and is a primary brow depressor.16 Weakening of the procerus muscle achieves significant medial brow elevation.
Depressor supercilii muscle
Distinct from the orbicularis oculi and corrugator muscles, the depressor supercilii muscle also acts as a depressor of the eyebrow. It originates as two distinct heads from the frontal process of the maxilla, approximately 1 cm above the medial canthal tendon. It travels superiorly and inserts onto the dermis approximately 13 to 14 mm superior to the medial canthal tendon. The angular vessel passes between the two muscle heads.17,18
Eyebrow Elevators
Frontalis muscle
The frontalis muscle (Fig. 1.1) is a part of the occipitofrontalis musculofascial complex of the scalp, which includes the occipitalis muscle, galea aponeurotica muscle, and frontalis muscle. The vertically oriented fibers of frontalis muscle extend from the broad fibrous tissue of the galea aponeurotica just inferior to the hairline and insert into the supraorbital dermis. Contraction of the frontalis muscle can elevate the eyebrow more than 20 mm and also causes horizontal furrows across the forehead. These furrows do not extend to the temporal hairline because the frontalis muscle thins laterally and does not extend past the temporal fusion line to the tail of the brow. The lack of frontalis pull over the tail of the brow explains the common temporal brow ptosis seen so commonly in older adults. The frontal branch of the facial nerve innervates the frontalis muscle. (The course of the frontal nerve will be discussed later in this chapter.)
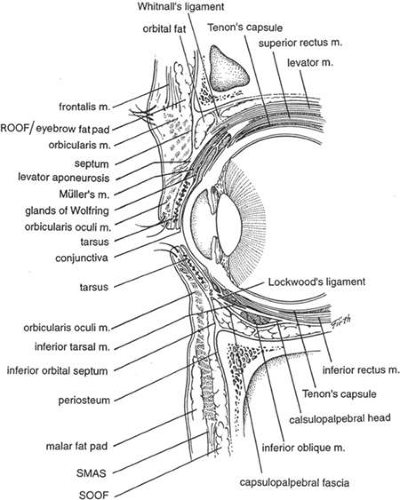
The galea aponeurosis joins the frontalis muscle anteriorly and splits around the frontalis muscle into a superficial and deep galea. The thinner superficial layer continues inferiorly as the anterior muscle sheath of the frontalis and orbicularis muscles, whereas the deep galea becomes the posterior muscle sheath. This deep galea layer divides inferiorly and encompasses the fat pad that lies beneath the interdigitation of the frontalis and orbicularis muscles and is termed the retro-orbicularis oculi fat pad (ROOF) or eyebrow fat pad (Fig. 1.2).
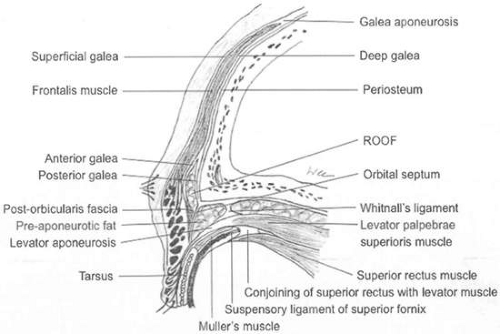 Figure 1.2. Relationship of galea aponeurosis, frontalis muscle, eyebrow fat pad (ROOF), and posterior orbicularis fascia. |
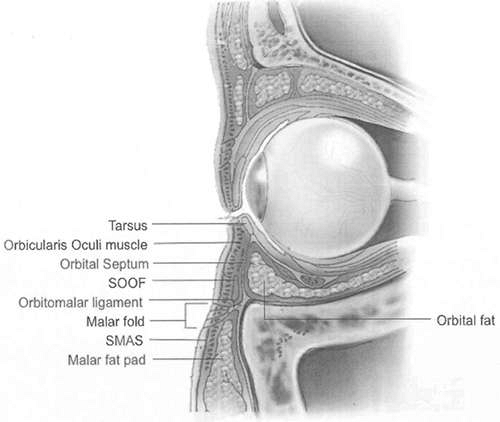
The ROOF is located in the supraorbital area mostly above the supraorbital rim and only a few millimeters below the rim, and it continues into the eyelid as the posterior orbicularis fascia12,19 (Fig. 1.2). This submuscular fat pad should not be confused with the subcutaneous fat, which is anterior to the muscle layer. With aging, involution changes can cause the ROOF to descend and the inferior aspect of the fat can prolapse into the eyelid. When this occurs, the fibrofatty ROOF can be mistaken for the more purely fatty preaponeurotic fat pad. This error in judgment can cause the orbital septum to be misidentified as the levator aponeurosis, which if mistakenly advanced, can result in marked lagophthalmos. Anteriorly, the posterior frontalis-orbicularis muscle fascia bounds the ROOF. Posteriorly, the fascial boundary of the ROOF is dense fibrous tissue, which extends inferiorly to the eyelid as the orbital septum20 (Fig. 1.2). Eyebrow fat contains both fibrous septae with interseptate fat-filled spaces and the branches of the facial nerve. This eyebrow fat pad continues laterally and inferiorly with the subsuperficial musculoaponeurotic system (sub-SMAS) fat in the malar region and the suborbicularis oculi fat (SOOF) of the lower eyelid.21 A recent study by Hwang et al.19 confirmed histologically that ROOF and SOOF were situated deep to the orbicularis oculi muscle and superficial to the orbital septum and periosteum. The group also demonstrated that ROOF and SOOF are distinct structures.
Function
The eyebrows provide several major functions, but the primary function is to protect the eye. The brow position and curvature, in conjunction with the protrusion of the brow ridge, helps shield the eyes from bright light coming from directly above, and is an effective barrier to liquids running from the forehead into the eye. The large hairs of the eyebrow have abundant sensory innervations that provide a sensitive awareness to tactile stimulation and helps detect objects near the eye (e.g., small insects). Accordingly, stimulation of the supercilia results in reflex blinking of both eyelids.
The eyebrows are also an important part of expressing emotion, body language, and human communication. Eyebrow position and contour are critical to facial configuration and are among the strongest indicators of mood and feeling. The emotional signals provided by the eyebrows appear to be universal.22 Elevation of the arched brow with associated forehead furrows tends to indicate surprise. A normally contoured eyebrow arch portrays happiness. Medial downward and lateral upward slanting with associated glabellar wrinkles tends to convey anger or concern. Low, flat eyebrows that hang over the eyes denote fatigue. A drooping of the temporal brow with the highest point medially suggests sadness. Elevation of only one eyebrow portrays a quizzical or questioning expression.23,24 These expressions serve as nonverbal forms of communication to convey emotion.23
Eyebrow position is functionally dependent on the interplay of elevators and depressors.13 Eyebrow elevation helps to clear the visual axis and is a natural compensatory response to the forehead sagging and dermatochalasis that occur with aging. The main elevator for the eyebrow is the frontalis muscle, which elevates the forehead and eyebrows and also serves as an accessory elevator of the upper eyelid. Maximal action of the frontalis will result in an additional 3 to 5 mm of elevation of the upper eyelid.12
Eyebrow depressors (corrugator supercilii, procerus, depressor supercilii, and orbicularis oculi muscles) are recruited during forceful eyelid closure. They are also active during visual concentration.
Injection of botulinum toxin into the glabellar muscles lessens forehead and brow wrinkles, but also impairs brow motility. Frontalis inactivation limits brow elevation, and depressor inactivation limits the ability to bring the brows together in a frown.25 Patients who receive botulinum toxin injection may appear happier and more youthful, but they also experience reduced ability to express emotion (particularly fear, anger, and sadness) or to communicate nonverbally.26,27
Eyelids
Structure
The eyelids are essential to protect the eye and maintain the ocular surface. They also provide an important contribution to the overall appearance of the face. The eyelids have a complex structure to support their various essential functions. Ideally, the distance between the two medial canthi is one horizontal palpebral width. In a normal adult, the palpebral fissure between the eyelid margins measures 9 to 11 mm vertically and 28 to 30 mm horizontally. In children, the upper eyelid margin rests at the superior limbus. In adults, the upper eyelid margin is 1 to 2 mm below the superior limbus. The highest point of the upper eyelid margin is slightly nasal to the central pupillary axis. The lower eyelid margin normally sits at the level of the inferior limbus and the lowest point is slightly temporal to the pupil.
The upper and lower lid margins each consist of both anterior and posterior lamellae. The anterior lamella is composed of skin, sebaceous and sweat glands, and the orbicularis oculi muscle. The posterior lamella includes conjunctiva, the tarsal plate, meibomian glands, and retractor muscles (Fig. 1.3). The anterior and posterior lamellae fuse together at the tarsus and separate from each other at the level of the septum. At the junction between the fused and the separated lamellae is the area where the upper lid crease forms.28
Eyelid Margin
The eyelid margin surfaces appose each other during eyelid closure. Medially, the lid margin is rounded without lashes and includes the lacrimal puncta and canaliculi. The upper and lower puncta are usually located 5 to 7 mm lateral to the medial canthal angle, with the lower punctum located 1 to 2 mm lateral to the upper punctum.
Anteriorly, the most distinguishing feature of the eyelid margin is the lashes. The upper lid contains five or six rows of cilia, whereas the lower lid contains three to four rows. Cilia serve a protective function for the ocular surface. Loss of lashes or madarosis may be indicative of an eyelid neoplasm. Whitening of lashes or poliosis may be a sign of blepharitis, medicamentosis, or Vogt-Koyanagi-Harada syndrome. Several sebaceous glands of Zeis empty into each lash follicle. The sweat glands of Moll also open onto the lid margin.
Posterior to the cilia is the gray line, which represents the terminal extension of the orbicularis muscle of Riolan. This line serves as a dissection guide to split the eyelid into the anterior and posterior lamella.
The tarsus is considered the backbone of the eyelid. It is composed of dense, fibrous connective tissue and houses the meibomian glands, which have their orifices on the lid margin posterior to the gray line. Low-grade inflammation or infection of these glands results in blepharitis, and occlusion of their orifices can lead to hordeola or chalazia. Meibomian glands can also be the site of sebaceous cell carcinoma. The meibomian glands, along with the glands of Zeis (located in the tarsal conjunctiva) produce the exterior, lipid layer of the precorneal tear film. The upper lid tarsus is 10 to 12 mm high, whereas the lower lid tarsus is only 3 to 4 mm high. The tarsal plates of the upper and lower lids contain approximately 30 to 40 and 20 to 30 meibomian glands, respectively. Distichiasis is the abnormal origin of metaplastic eyelashes from the meibomian glands. This may be present congenitally, or in association with Stevens-Johnson syndrome, ocular cicatricial pemphigoid, chemical injury, or other trauma. In contrast, trichiasis is the inward misdirection of eyelashes with normal origin.
Skin
The eyelid skin is the thinnest and most mobile skin in the body.29 This allows the formation of a thin upper eyelid skin fold, and facilitates the spontaneous, quick blinking movement of the eyelid. Adequate skin coverage that is at least 20 mm from upper lid margin to inferior eyebrow border is necessary to permit unrestricted eyelid closure. Beneath the skin is loose areolar tissue with very little subcutaneous fat, and the area between the eyebrow and eyelid margin is almost devoid of subcutaneous fat. The areolar tissue is about 4 to 6 mm thick below the eyebrow and tapers to <0.1 mm thick in the pretarsal eyelid30 (Fig. 1.2). This loose connective tissue plane provides a potential space for accumulation of fluid. The eyelid skin receives its sensory innervation from the first and second divisions of the trigeminal nerve.
Musculature
Protractors
Orbicularis Oculi
The main eyelid protractor is the orbicularis oculi. This superficial muscle lies just deep to the eyelid skin and anterior to the tarsal plate and septum. It is part of the SMAS, and is continuous with other facial muscles in this plane. It circumferentially surrounds the palpebral fissure, and firmly attaches to the tarsal plate. The vertical lateral fibers play a role in the formation of horizontal skin wrinkles at the lateral angle of the eye.12 The orbicularis also attaches to the medial and lateral orbital rim via the medial and lateral canthal tendons and has an additional bony attachment along the orbital rim via the orbitomalar ligament (orbital retaining ligament) 21,31,32,33
Jones34 re-emphasized the division of the orbicularis oculi muscle into three concentric components: pretarsal, preseptal, and orbital components (Fig. 1.1). The innermost component, the pretarsal orbicularis oculi, is anterior to and tightly adherent to the tarsal plate. It is responsible for quick eyelid closure and facilitates eyelid blinking. Loss of these fibers can cause severe functional problems and insufficient blinking. Accordingly, the pretarsal orbicularis muscle should be preserved during blepharoplasty. The pretarsal orbicularis originates medially from the superficial and deep limbs of the medial canthal ligament. The superficial head overlies the punctal ampullae and surrounds the canaliculi. The deep head (Horner’s muscle) inserts on the posterior lacrimal crest.35 Both superficial and deep components of the pretarsal orbicularis are responsible for the lacrimal pump mechanism.36,37 Contraction of Horner’s muscle draws the eyelid medially and posteriorly and assists in the lacrimal excretory pumping function.34
The deep head of the pretarsal orbicularis muscle is also crucial in maintaining globe-eyelid apposition. These muscle fibers will function properly only if the fibers are running parallel to the curvature of the eye’s surface. If the canthal insertions of the muscle are weakened, the muscle can dislocate and induce a floppy eyelid or an upper eyelid ectropion. Inadequate upper eyelid skin causes restriction of the downward movement of the eyelid margin, and the contracted pretarsal orbicularis muscle tends to pull the posterior lamella downward causing an upper lid entropion.
A very small component of the orbicularis muscle, the muscle of Riolan, is a terminal extension of the pretarsal orbicularis to the eyelid margin. It corresponds anatomically to the gray line, and is separated from the orbicularis oculi muscle by the eyelash follicles.38 This muscle is thought to rotate the lashes during eyelid closure, and may also help expel glandular contents from the meibomian glands.
The preseptal orbicularis oculi muscle lies anterior to the orbital septum, between the pretarsal portion and the orbital portion of the orbicularis oculi. Putterman39,40 identified the separation between preseptal orbicularis muscle and orbital septum in both upper and lower eyelids as a structure called the postorbicularis fascia. This fascia is the inferior continuation of the eyebrow fat pad or ROOF (Fig. 1.2). Contraction of these muscle fibers results in involuntary blinking and unforced as well as forced eyelid closure. This portion of the orbicularis oculi muscle is susceptible to involutional changes which cause bunching of the eyelid skin fold and disturbs the formation of the lid crease. Resection of a portion of these muscle fibers during blepharoplasty weakens the muscle but does not generally create a significant functional problem, unless removal is excessive.
The orbital portion of the orbicularis oculi muscle overlies the orbital rim and is separated from orbital rim by the eyebrow fat pad (ROOF) in the upper eyelid and SOOF in the lower eyelid19 (Fig. 1.3).
All components of the orbicularis oculi muscle are innervated by the facial nerve with innervations entering from the underside of the muscle (as with almost all the muscles of facial expression).
Retractors
Levator Palpebrae Superioris Muscle
The levator palpebrae superioris muscle, the primary retractor of the upper eyelid, provides excellent vertical lift. Normal levator excursion from downgaze to upgaze should measure approximately 14 to 17 mm.41
This skeletal muscle arises from the annulus of Zinn at the lesser wing of the sphenoid bone, lateral to the superior oblique muscle and above the superior rectus muscle. In the orbit, the levator lies above the superior rectus muscle where they share a common muscular sheath42 and both are innervated by the superior division of the oculomotor nerve. The muscle then travels anteriorly in the superior orbit until reaching Whitnall’s ligament, where it is redirected inferiorly and anteriorly.
Whitnall’s ligament also serves as a transition zone between the tendinous, distal 14 to 20 mm of the muscle referred to as the levator aponeurosis and the proximal 36 mm muscular portion.43 Whitnall’s ligament is a transverse, fibrous condensation situated immediately behind the superior orbital rim. This ligament extends from the fascia surrounding the lacrimal gland temporally to the trochlea medially. The relationship of Whitnall’s ligament to the levator is fixed, and the levator muscle does not slide through the ligament freely; rather, it acts as a fulcrum and allows the levator muscle to change its direction of pull from anteroposterior to superoinferior.44
The fibrous levator aponeurosis begins at the level of Whitnall’s ligament and extends inferiorly into the eyelid to insert on the anterior surface of the superior tarsal plate. It also sends fibrous extensions through the orbicularis muscle onto the upper eyelid dermis to create the upper eyelid skin crease.45
In addition to the palpebral insertions, the levator aponeurosis expands into a broad, fibrous sheet to insert as horns into the orbital margin at the medial and lateral canthal region. The lateral horn is much thicker and stronger than the medial horn and divides the lacrimal gland into orbital and palpebral lobes.
Mueller’s Muscle
Mueller’s muscle complements the function of the levator muscle. This smooth muscle originates from the undersurface of the levator, 15 mm from the upper tarsal border, and inserts onto the superior border of the upper lid tarsus. Posteriorly, it firmly adheres to the conjunctiva. The muscle fibers contain α2-adrenergic receptors and are innervated by the sympathetic nervous system.
Mueller’s muscle provides 2 mm of additional elevation of the upper eyelid. It can be stimulated by sympathetic responses, such as fear or surprise, or pharmacologically by the instillation of phenylephrine drops.
Recent studies have shown that Mueller’s muscle extends laterally between the orbital and palpebral lobe of the lacrimal gland along with the lateral horn of the levator muscle. Hence, it may accentuate the lateral flare of the palpebral fissure frequently seen in eyelid retraction associated with thyroid-related eye disease.46
Lower Eyelid Retractors
The lower eyelid does not require substantial vertical excursion. Accordingly, the lower eyelid retractors are much less developed, and serve mainly to depress the lower eyelid in downgaze.
The lower lid retractors consist of the capsulopalpebral fascia and the inferior tarsal muscle (Fig. 1.3). The capsulopalpebral head of the inferior rectus originates from the sheath of the inferior rectus muscle. This fascia splits to accommodate the inferior oblique muscle. The anterior portion is the capsulopalpebral fascia, and the posterior aspect is known as the inferior tarsal muscle. The inferior tarsal muscle is composed of sympathetically innervated smooth muscle. The muscles fuse superiorly and insert together onto Tenon’s fascia and the inferior tarsal border. The capsulopalpebral fascia also inserts into the septum, orbicularis, and skin to create the lower eyelid crease.
The lower eyelid retractors are commonly incised during the transconjunctival surgical approach to the orbit. Disinsertion of the lower eyelid retractors leads to vertical lower eyelid instability and is part of the pathophysiology of both involutional ectropion and entropion. Clinically, this manifests as decreased excursion of the lower lid on downgaze and deepening of the inferior fornix. The dehisced lower lid retractors are visible as a white horizontal line in the inferior fornix.47
Lockwood’s Ligament
Lockwood’s ligament arises from the fused fascia of the inferior rectus and inferior oblique muscles. It is a hammocklike suspensory ligament that is strongest anterior to the inferior oblique muscle and supports the globe after orbital floor removal and maxillectomy, provided that its medial and lateral attachments are intact.48
Orbital Septum
The orbital septum defines the anterior extent of the orbit and the posterior extent of the eyelid (Fig. 1.3). This membrane arises from the white, fibrous arcus marginalis and extends circumferentially along the periosteum of the bony orbital margin. In the Caucasian or Occidental upper lid, it joins the levator aponeurosis 2 to 5 mm above the superior tarsal border. In the Asian upper lid, the orbital septum fuses with the levator aponeurosis more inferiorly (Fig. 1.4). In the lower lid, the septum fuses with the lower lid retractors just inferior to the inferior tarsal border.49 The orbital septum serves as a barrier to the posterior extension of preseptal fluid and a partial barrier to the spread of preseptal infection.
Skin Crease
Upper Skin Crease
The upper eyelid skin crease separates the upper eyelid skin fold from the flat pretarsal component; it is formed by the insertion of the levator aponeurosis extending through the orbicularis oculi muscle into the skin. Typically, the upper eyelid crease measures 10 to 12 mm in women and 7 to 8 mm in men. Asians typically have a low or ill-defined eyelid crease, owing to variable fusion distances of the aponeurosis below the superior tarsal border (Fig. 1.4). This inferior extension of the septum allows the preaponeurotic fat to descend anterior to the tarsal plate. A pretarsal fat pad can often be identified in the Asian eyelid but not in the Caucasian eyelid. This fat pad prevents levator fibers from extending toward the skin. Accordingly, the primary fusion of the levator aponeurosis into the orbicularis muscle and skin occurs closer to the eyelid margin, resulting in the absent or lower crease of the Asian upper eyelid.50,51 Other unique features of the Asian eyelid include vertically narrow palpebral fissures, lash ptosis, a full appearance to the upper lids and sulci, and a relatively common occurrence of epicanthal folds.52
Lower Skin Crease
The lower eyelid skin crease is formed by cutaneous insertions of the lower eyelid retractors. The lower eyelid crease is commonly seen in children, but is usually not visible in adults.
Orbitomalar Ligament
The orbitomalar ligament is one of the major supporting structures of the midface. Kikkawa et al.21 first characterized the anatomic connections of the orbitomalar ligament in 1996. It extends from the thickened periosteum along the inferior orbital rim and fans out in lamellar fashion, traveling through the SMAS, subcutaneous fat, and subsequently inserting into the skin (Fig. 1.5). This cutaneous insertion corresponds to the malar skin fold and nasojugal skin fold in the lower lid. The malar fold separates the thin lower eyelid skin from the thicker skin of the cheek and the more medial nasojugal fold, is a landmark for the angular vessels (Fig. 1.1).
Histologically, the orbitomalar ligament consists of collagen and elastic fibers. In 2002, Muzaffar et al.31 described a bilaminar septum-like structure attaching the orbicularis oculi muscle (at the junction of preseptal and orbital portion) to the inferior orbital rim and applied the term orbicularis retaining ligament to this structure. As a bilaminar membrane, the layer on the orbital side is thought to derive from a reflection of the orbital septum. Inferiorly, the membrane is derived from a continuation of the membrane covering the preperiosteal fat over the zygoma. This ligament is weakest centrally and tightest over the inferolateral orbital rim.
A recent study by Ghavami et al.32 in 2008 described the entire circumferential nature of the attachment of this ligament around the orbital rim. The ligament was shown to be continuous from the medial orbit to the lateral orbit in both the upper and lower eyelids. In the upper eyelid, it originates 2 to 3 mm above the insertion of the orbital septum along the superior orbital rim, and then merges with the septum onto the orbital rim at the arcus marginalis. Laterally, this ligament is longer and more lax than it is medially, which may partially explain the phenomenon of lateral hooding of the upper eyelid. The ligament serves as a fixation point for the orbicularis muscle of the upper and lower eyelid, and also has a protective capability in this anatomic location. For example, in the upper eyelid this ligament may help avoid upper eyelid ptosis when botulinum toxin is injected above the level of its origin at superior orbital rim. Normally, the orbitomalar ligament elongates with age as shown by Lucarelli. In the lower eyelid, this elongation and associated orbital septum attenuation allows orbital fat to move anteriorly and sometimes herniate below the inferior orbital rim.
Function
The complex structure and intricate neurologic control mechanisms of the eyelids enable the lids to perform various essential functions. In addition to protecting the eye and maintaining a healthy ocular surface, the eyelids also contribute significantly to facial features. They are important in the expression of emotion, as well as in facial recognition, and indicate states of attention.
Several distinct functions of the eyelid work together to provide a protective mechanism for the eye and to maintain a healthy ocular surface.53 The functions are
Voluntary eyelid opening
Tonic eyelid elevation for sustained opening of the eye
Involuntary lid–eye coordination to adjust eyelid position relative to vertical globe movement
Spontaneous and reflex blinking
Voluntary eyelid closure
Firm eyelid closure for eye protection or for expressive acts such as sneezing
The levator palpebrae superioris muscle is primarily responsible for the first three eyelid functions listed above. The remaining eyelid functions correlate to the action of the orbicularis oculi muscle and synchronously inhibited levator muscle function.
Accordingly, eyelid opening, eyelid position, and lid-eye coordination are unaffected by facial nerve dysfunction, whereas blinking and firm eye closure are affected.
Voluntary Opening
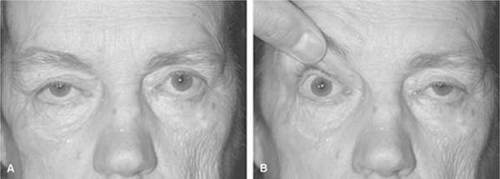
Eyelid opening is produced primarily by the levator palpebrae superioris muscle, which is innervated by the superior division of the oculomotor nerve and elevates the upper eyelid. Voluntary control of the levator muscle affects both eyelids synchronously because the levator muscles of both eyes share a common brainstem nucleus.53,54
The neural mechanism responsible for maintaining conjugate eyelid movements may be tightly linked to the mechanism that controls conjugate eye movement, known as Herring’s law of equal innervation for eye movement. This hypothesis is supported by several studies.54,55,56 Despite this, the eyelids can still elevate independently by imposing asymmetric frontalis activity.57 In patients with unilateral ptosis, the increase in levator stimuli in the ptotic eyelid causes retraction of the contralateral normal eyelid because of the principle of equal innervation. Covering or manually raising the ptotic eyelid eliminates the increased levator stimulation in the ptotic eye, which causes the contralateral normal eyelid to return to normal position, or causes contralateral ptosis in patients with bilateral asymmetric ptotis55 (Fig. 1.6). This concept is crucial in ptosis surgery, because the contralateral lid may demonstrate postoperative ptosis after correction of only the more severely ptotic eyelid in those patients with asymmetric bilateral ptosis who complain only of unilateral ptosis preoperatively.