4 Evaluation of the Outpatient Geriatric Patient
 Introduction
Introduction
Older adults differ from younger adults in many ways that can affect evaluation strategies and, ultimately, treatment decision making. This chapter reviews the most salient of these characteristics and offers guidance to otolaryngologists with geriatric patients.
Population demographics mean that ever-increasing numbers of older adults will seek otolaryngology care in the coming decades.1 The impact of these changes will be ubiquitous, affecting the entire discipline with the exception of pediatric specialties and practices. Otolaryngologists readily understand that outpatient evaluation of a child differs from that of an adult, but many physicians do not recognize that the evaluation of an elderly adult also requires modification. Some of the differences between older adults and younger or middle-aged adults may not be readily apparent. Moreover, older adults vary dramatically within specific age ranges, with far more heterogeneity than children or even young adults. It is not uncommon to encounter patients in their 90s who appear to have lower disease burden than many in their 50s and 60s. The potential reasons for these disparities are numerous and collectively drive the need to comprehensively evaluate older patients who present for otolaryngological care.
The unique characteristics of older adults that impact outpatient evaluation in the typical otolaryngology practice include, but are not limited to, the following:
• Reduced functional reserve (frailty)
• Multiple comorbidities
• Polypharmacy
• Multiple physicians
• Sensory impairment (vision, hearing loss, olfaction)
• Reduced mobility
• Impaired balance with increased risk of falls
• Dysphagia, eating disorders
• Cognitive decline
• Inadequate social support
• Goals and expectations differ from those of younger adults
 Comprehensive Geriatric Assessment (CGA)
Comprehensive Geriatric Assessment (CGA)
The standard benchmark for geriatric evaluation is the comprehensive geriatric assessment (CGA), which is a standard assessment performed by geriatricians.2 The CGA is intended to serve as a baseline for the geriatrician in directing a patient’s medical care. As its name implies, it is comprehensive, requires hours to complete, and is usually unnecessary for the purposes of decision making in an otolaryngological office. Performance of a CGA should therefore be delegated to geriatricians. However, there are multiple evaluation components that should be performed by otolaryngologists, particularly those regarding surgical candidacy for older adults. These are discussed in this chapter in roughly descending order of importance. A useful tool is the Vulnerable Elderly Survey 13 (VES-13), which assesses physical well-being and strength as well as the subject’s ability to perform common activities of daily living (ADLs) without assistance.3
 Reduced Functional Reserve
Reduced Functional Reserve
Increased risk of frailty is the most critical defining characteristic of the elderly of which otolaryngologists must be aware. Frailty, a measure of reduced functional reserve, places the older adult at risk for a plethora of adverse and unanticipated consequences from seemingly minor interventions, including increased likelihood of surgical complications as well as ultimate hospital discharge to a setting other than home.4,5 Younger adults have substantial functional reserves in all organ systems in that they routinely use only a percentage of the total capacity of the organ system. Older adults may appear to be just as resilient as younger adults at first glance, but when stressed they may quickly exhaust their resources and suffer multiple-system organ failure. Therefore, assessment of frailty must be considered a fundamental part of any evaluation of older adults when surgical intervention is a consideration. Like Justice Potter’s famous statement regarding pornography, most people would state they are unable to define frailty, although they “recognize it when (they) see it.” However, as practitioners of the science as well as the art of medicine physicians are obligated to be more rigorous in their assessments than merely relying on subjective impression. Evaluation of frailty falls into this paradigm because objective measures of frailty exist and are used by some practitioners. These measures have been validated by several longitudinal studies, including studies that demonstrate a strong correlation with surgical outcomes.4–6 Measures may be demonstrated either on examination or via biochemical assessment. Several biochemical measures, such as circulating levels of D dimer (D-dimer assay) and interleukin-6 (IL-6) have been reported to correlate with other measures of frailty.6 For the purposes of outpatient evaluation there are several easily performed tests that all otolaryngologists can incorporate into their clinical practice. The reader will note that these can be divided roughly into subjective (exhaustion; reduced anxiety level) and objective (unintentional weight loss > 10 lb; getup-and-go test; grip strength) criteria.4
The get-up-and-go test is performed by arising from a sitting position, walking 8 feet, and returning and sitting. Scoring is 1 through 3, with loss of a point for (1) using arms to get up, (2) uncertain gait, and (3) taking longer than 10 seconds.7 Another test often used is measurement of walking speed (15 feet in 6 seconds or less).8
Grip strength is measured with a dynamometer, a low-cost device in common use. Normal men should produce more than 29 kg (median 39 kg), women somewhat less.9 Both of these measures correlate with both short-term and long-term survival and are considered valid measures of frailty.
 Comorbidities and Polypharmacy
Comorbidities and Polypharmacy
As patients age, they commonly collect new diagnoses as well as accumulate an ever-increasing list of medications to manage these illnesses. This characteristic is not unique to older adults, and otolaryngologists frequently encounter younger patients with more extensive comorbidities and longer medication lists than some of their elderly patients. Nonetheless, evaluation of geriatric patients requires diligent review of comorbid conditions with particular attention to medication lists. “Medication reconciliation” is recognized as a key component of high-quality health care and is particularly critical—and challenging—in the elderly. As the number of medications increases, the opportunity for unanticipated or unrecognized adverse effects increases as well. Elderly patients are at much higher risk for several reasons, including alterations in drug metabolism as well as pharmacokinetics. Diseases and conditions managed by otolaryngologists, particularly balance and swallowing disorders, are frequently impacted by medications being administered for other disorders. Well-established guidelines such as the Beers criteria list of potentially inappropriate medications10 and the American Geriatrics Society clinical practice guideline on fall prevention11 emphasize the significance of prescribed medications in increasing morbidity. Often the otolaryngologist is the first provider to note a relationship between balance or swallowing complaints and the patient’s medication list. Common offenders are psychoactive medications, including selective serotonin reuptake inhibitors (SSRIs), and anticholinergics, although other medication classes are often implicated as well. As such, it is incumbent on the otolaryngologist to review medication lists carefully, verify them with the patient (or the patient’s caregiver), and review possible interactions and untoward effects. This task is daunting because even the newer electronic health records (EHRs) typically fail to capture all medications that the patient is taking. The author of this chapter has himself been “victimized” by failure of the EHR (in this case the Veterans Health Administration Computerized Patient Record System [VHA CPRS]) to capture accurately all the medications being taken by elderly or cognitively impaired patients. In the absence of a truly interoperable health information exchange system in the United States, it falls to the provider and office staff to seek and update carefully and compulsively lists of all medications being taken by patients in the practice.
 Cognitive Decline
Cognitive Decline
Older adults are often quite adept at compensating for cognitive changes until late in disease progression. As such, casual conversation may fail to identify those with short-term memory loss or other information-processing defects. Standardized tests are available, of which the Mini-mental State Examination (MMSE) is the best known. This examination is copyrighted by Folstein12 but has been excerpted by many groups and organizations.13 Carefully scripted questioning by the otolaryngologist may provide valuable clues that cognitive decline is becoming potentially significant and should be investigated further. Inquiries regarding recent activities, family issues, other medical problems, schedules, and so forth, may yield enlightening results, particularly if the answers are associated with obvious confusion or confabulation. The following MMSE sample questions are excerpted from http://www.health.gov.bc.ca/pharmacare/adti/clinician/pdf/ADTI%20SMMSE-GDS%20Reference%20Card.pdf:
• Questions: What day of the week is this? What is tomorrow’s date? What country are we in? What city are we in?
• Say: “I am going to name three objects. When I am done, I will want you to repeat them. Remember them because I am going to ask you to repeat them later.”
• Spell the word world. Now spell it backward.
• “Now, what were the three objects I asked you to remember?”
• Show pencil, wristwatch. “What is this called?”
Recent evidence linking cognitive decline to unaided hearing loss is of particular importance to the otolaryngologist14 and is discussed in greater depth elsewhere in this text. Failure of older adults to respond appropriately to amplification suggests defective executive function, and should be interpreted as requiring further testing. “Speech-in-noise” or other specialized audiometry testing should be employed in the evaluation of older patients with evidence of mild cognitive decline or evidence of poor auditory rehabilitation following aiding. Perhaps even more pertinent is newer evidence suggesting early amplification may retard cognitive decline—a topic beyond the scope of this chapter.
 Assessment of Social Support
Assessment of Social Support
Historically, in the United States and in many cultures today, elderly people benefited from the support of their children and extended family. However, dramatic changes in U.S. culture including smaller families, mobile society, and two-income families mean that many elderly have no nearby family members to care for them. When their children have left home older people often relocate to “adult communities” remote from family and friends. As they age and require increasing levels of support, they may—or may not—be able to access support from community infrastructure and friends. In many such communities, support for the elderly is by other elderly—an obviously time-limited arrangement. As a result, some assessment of support is necessary for all elderly patients. This should include documentation of family member availability, community resources, primary care and other physicians, and assessment of travel needs and modalities. It is not uncommon to encounter patients in their 90s still driving to their appointments despite high levels of frailty and mild cognitive decline. It is not the intent of this chapter to address otolaryngologist involvement in deciding the wisdom of such behaviors, but clearly there is an expectation that any concerns be communicated not only to the patient, but also to the family and primary care provider.
 Eliciting Patient Goals
Eliciting Patient Goals
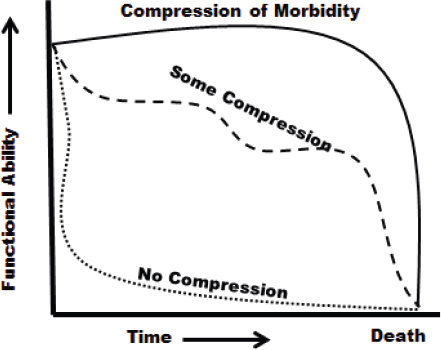
The goals and expectations of older adults usually differ from those of younger adults. These include independence, mobility, ability to communicate with family and friends, and avoidance of being alone, issues that younger people take for granted. One of the primary goals of most adults (old or young) is what geriatricians term compression of morbidity.15 Aging is accompanied by the recognition that life is time-limited, and that sooner or later all must die. However, gradual decline may not be inevitable because illness and functional ability may be modifiable such that disability is compressed into the shortest possible time prior to death (Fig. 4.1). Older patients are not so much afraid of dying as they are afraid of prolonged disability. Elicitation and identification of specific goals is a critical component of assessment of an older patient. Open discussion with the patient and caregiver (if available) should be undertaken at the first consultation, and the discussion should be reopened whenever difficult decisions arise. The goal of compression of morbidity may lead to decisions to avoid invasive procedures that have the potential to lead to long-term disability—or, conversely, may suggest early, aggressive intervention to extend useful, rewarding life even when the intervention may be accompanied by risk of earlier demise. This sort of decision making defies application of standard guidelines and mandates open, forthright discussion. Most older adults have no difficulty in making such decisions if the choices are clear and unambiguous. Unfortunately, predicting outcomes for a specific individual is a daunting task, regardless of age. Such discussions must include a frank disclosure of uncertainty when it exists, as well as clear openness on the part of the physician to accept and work with decisions made knowledgeably by each older patient.