Infections of the upper airways are a frequent cause of morbidity in children. Viral laryngotracheobronchitis (croup) is the most common cause of stridor in children and usually has a self-limited course with occasional relapses in early childhood. Epiglottitis has become rare in developed countries with the advent of universal vaccinations against Haemophilus influenzae . It can be rapidly fatal, however, if not promptly recognized and appropriately managed. This article reviews the pathogenesis, epidemiology, clinical presentation, diagnosis, and management of these pediatric upper airway infections.
Croup
Laryngotracheobronchitis (croup) is a viral-mediated inflammatory condition of the subglottic airway that typically affects children between age 6 months and 3 years. Before the modern era of pediatric airway management, croup was considered a major cause of morbidity and mortality in children. Reports dating back to the 1800s describe as much as a 100% mortality rate from diphtheric croup, for which the only management was tracheotomy to bypass the obstructed airway. Although not the first to attempt intubation for croup, Joseph O’Dwyer, an obstetrician from New York, is credited with developing the first set of instruments designed for endotracheal intubation of children who had croup in the 1880s. In his first series of 50 cases of children who had croup, the mortality rate was 76% after intubation, which was an improvement over the almost certain death from the disease alone during this era. By 1887, O’Dwyer’s mortality rate was as low as 50% .
With the advent of modern techniques to support and secure the airway, mortality from croup has become a rarity in developed countries. Most children can be managed in the primary care setting, with even the most recalcitrant cases manageable without the need for a surgical airway intervention.
Pathogenesis
The subglottis is the region of the airway between the true vocal folds and the trachea. It is the narrowest point of the pediatric airway and the most common site of inflammatory conditions causing clinically significant airway obstruction in children. There are a number of reasons why even a small amount of inflammation in the subglottis can result in airway compromise:
The subglottis is the only region of the airway bounded by a complete cartilaginous ring that prevents the airway’s outward expansion in the face of edema.
The pseudostratified, ciliated, columnar respiratory epithelium lining the subglottis is loosely adherent to the underlying perichondrium.
Numerous mucus-secreting glands lie within the subgottis mucosa.
Even 1 mm of edema in the normal pediatric subglottis reduces its area by more than 50%.
Croup is typically caused by respiratory viruses, with parainfluenza I, II, and III accounting for up to 80% of cases. Parainfluenza I is the etiologic agent in 50% to 70% of patients who are hospitalized for croup . Other pathogens implicated in the pathogenesis of croup include adenovirus, respiratory syncytial virus, varicella, herpes simplex virus measles, enteroviruses, Mycoplasma pneumoniae , and influenza viruses A and B . Influenza-mediated croup is associated with a more severe disease course compared with parainfluenza . The virus is transmitted through inhalation and infects the epithelial cells of the laryngeal and tracheal mucosa, causing edema and glandular hypersecretion. Bacteria are an infrequent cause of croup, although bacterial tracheitis, which can result in significant airway obstruction and even death from the accumulation of pseudomembranes and fibrinous exudate within the airway, is most often caused by Staphylococcus aureus and Streptococcus pyogenes . Fungi and mycobacteria are extremely rare infectious causes of laryngotracheobronchitis and, when noted, should raise suspicion of an underlying immunodeficiency.
Noninfectious narrowing of the subglottis caused by congenital stenosis, internal or external laryngeal trauma, thermal injury, mass lesions such as hemangioma, and aspirated foreign bodies may present with clinical and radiographic findings similar to acute infectious laryngotracheobronchitis. Intubation may result in a series of changes within the subglottis (beginning with inflammatory edema and perichondritis) that occasionally progresses to mature subglottic stenosis. During the evolution of subglottic stenosis, the patient may present with symptoms that are not differentiable from viral croup. The role of supraesophageal reflux in the pathogenesis of croup remains unclear. A study by Contencin and Narcy demonstrated that 100% of eight patients who had recurrent croup had pH probe studies consistent with reflux.
Epidemiology
Croup is the most common cause of stridor in children and accounts for up to 15% of emergency department and primary care visits for respiratory infections in the United States . It most commonly affects children, with its peak incidence at age 2 years; however, there are isolated reports of cases in adults . The annual incidence ranges from 1.5% to 6% in children younger than 6 years . There is a slight male preponderance (male-to-female ratio, 3:2) . The incidence of croup is highest in the fall and early winter months.
Most cases of croup are managed in the primary care or emergency room setting, with 1.5% to 31% of patients requiring admission and less than 5% requiring endotracheal intubation . The mortality from croup has greatly decreased over the past 50 years secondary to advances in pediatric intensive care and airway management. Nevertheless, there are still isolated reports of mortality from croup, emphasizing the need for vigilant observation and early airway intervention in severe cases .
Clinical presentation
The patient who has croup typically presents with a hoarse voice, a “barking” cough, a low-grade fever, and variable degrees of stridor and respiratory distress. In contrast to epiglottitis, children who have croup typically present with a viral prodrome that may include rhinorrhea, cough, and sore throat for 1 to 2 days before the onset of the classic croup symptoms. A risk factor evaluation should always be sought, with careful attention paid to the patient’s neonatal and intubation history.
Examination findings may be similar to those of a viral upper respiratory tract infection, but children who have croup typically do not present with the toxic appearance characteristic of epiglottitis. A low-grade fever is often noted on examination, as is the finding of a hoarse voice, the characteristic high-pitched barking cough, and stridor. An evaluation for signs of respiratory distress including tachypnea, retractions, nasal flaring, agitation, lethargy, oxygen desaturation, and cyanosis should be performed. The Westley score is a tool used in various institutions to characterize the severity of respiratory distress in children who have croup ( Table 1 ) . The clinical efficacy of this and other scoring systems has not been extensively evaluated, and their utility remains controversial. The complete examination of the patient who has croup should include an evaluation for the presence of cutaneous hemangiomas, which may raise the possibility of a subglottic hemangioma, especially if present in a patient younger than 6 months who has croup.
| Indicator of disease severity | Score |
|---|---|
| Stridor | |
| None | 0 |
| Only with agitation/excitement | 1 |
| At rest with stethoscope | 2 |
| At rest without stethoscope | 3 |
| Retraction | |
| None | 0 |
| Mild | 1 |
| Moderate | 2 |
| Severe | 3 |
| Air entry | |
| Normal | 0 |
| Decreased | 1 |
| Severely decreased | 2 |
| Cyanosis | |
| None | 0 |
| With agitation | 4 |
| At rest | 5 |
| Level of consciousness | |
| Normal | 0 |
| Altered mental status | 5 |
Croup usually presents in children between age 6 months and 3 years, with a discrete episode of symptoms lasting between 3 and 7 days. Up to 5% of children may have more than one episode . Patients who are younger than 6 months when they first present with croup, those who have an unusually long duration of symptoms (>1 week), those who have unusually severe symptoms, and those who have recurrent croup should be evaluated for congenital or acquired airway narrowing.
Spasmodic croup is a nebulous condition that presents with a history and physical examination similar to viral croup without the associated infectious clinical findings. The patient is usually acutely symptomatic at night, with rapid resolution of the condition occurring over a period of 24 to 48 hours . The etiology of spasmodic croup is unknown but may be allergic. The differential diagnosis of croup is listed in Box 1 .
Congenital
Laryngomalacia
Vocal cord paralysis
Laryngeal web
Subglottic stenosis
Subglottic hemangioma
Tracheomalacia
Infectious/inflammatory
Respiratory papillomatosis
Epiglottitis
Peritonsillar abscess
Deep neck space infection
Diphtheria
Bacterial tracheitis
Mycobacteria
Laryngeal candidiasis
Angioedema
Wegener’s granulomatosis
Extraesophageal reflux
Traumatic/toxic
Acquired subglottic stenosis
Inhalational injury
Foreign body
Vascular
Innominate artery compression
Double aortic arch
Aberrant subclavian artery
Pulmonary artery sling
Neoplastic
Diagnosis and initial management
The diagnosis of croup should be made clinically. The characteristic barking cough, hoarse voice, stridor, and low-grade fever in the absence of the previously mentioned risk factors may obviate the need for additional diagnostic tests, which are nonspecific. If the patient presents with significant respiratory distress, expeditious coordinated care should be arranged between the otolaryngologist, anesthesiologist, and critical care intensivist. Measures to secure the airway are of utmost priority. Supplemental humidified oxygen and racemic epinephrine may be administered until definitive intervention to secure the airway can be undertaken. Care must be taken during this period to avoid excessive stimulation of the child because this may exacerbate the airway compromise.
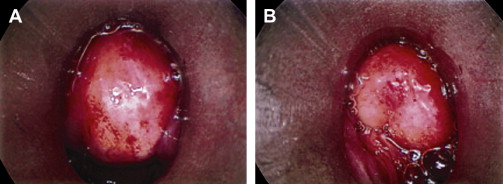
If the patient is stable and the diagnosis is in question, high-kilovoltage plain films of the airway and a chest radiograph may be obtained to rule out findings suggestive of another etiology. Anteroposterior films may demonstrate symmetric subglottic narrowing (“steeple sign”), although this may be absent in up to 50% of cases and may be present in the absence of croup ( Fig. 1 ) . Flexible fiberoptic laryngoscopy has a limited ability to evaluate the subglottis but may be sought to rule out pathology of the supraglottis and vocal cords when the diagnosis is unclear. Direct microlaryngoscopy and bronchoscopy (MLB) is the gold standard for the diagnosis of airway lesions and should be employed (1) when the diagnosis of croup is in question after noninvasive testing, (2) in the evaluation of a patient who has atypical croup, (3) when bacterial tracheitis is suspected, and (4) in patients who have risk factors suggestive of underlying airway pathologies. If possible, the patient should be at his or her baseline before performing MLB to most accurately assess the airway in the absence of acute edema. Moreover, MLB of the acutely infected airway may result in exacerbation of the edema secondary to manipulation, which may worsen the patient’s airway obstruction.
Definitive management
When the airway is deemed stable and the diagnosis of croup is established, supportive and medical measures should be employed in the primary care or emergency room setting. Sixty percent of children present with mild croup symptoms and are often discharged from the emergency department without any treatment . Supportive measures may include placing the patient in a cool-mist “croup” tent; medical options include possible administration of oxygen, racemic epinephrine, and systemic steroids. The value of cool mist, which was the mainstay of therapy for croup for over a century, is controversial. Cool mist is thought to improve airflow through the edematous subglottis by decreasing the viscosity of secretions. A recent meta-analysis and randomized controlled trial failed to demonstrate the benefit of cool mist in the outcome of moderate and severe croup .
Due to their significant anti-inflammatory effects, systemic steroids are the mainstay of therapy for patients with croup and can be administered by way of nebulization and oral or intravenous routes. The liberal administration of steroids for mild to severe croup significantly reduces the severity and duration of croup episodes and is thought to be responsible for the dramatic decrease in the need for hospital or intensive care admissions and endotracheal intubation . In a double-blinded controlled trial, Bjornson and colleagues reported a statistically significant reduction in symptoms, parental stress, and the need for subsequent care after administration of a single dose of oral dexamethasone (0.6 mg/kg) to patients who had mild croup. Two recent randomized trials demonstrated similar efficacy of low-dose (0.15 mg/kg) and high-dose (0.6 mg/kg) dexamethasone in reducing croup symptoms . Amir and colleagues recently demonstrated no difference in the outcome of mild to moderate croup after administration of oral or intramuscular steroids. Donaldson and colleagues noted similar findings in their study assessing intramuscular versus oral steroids in patients who had moderate to severe croup. Both of these studies highlight the utility of oral steroid therapy due to ease of administration in the ambulatory setting. The role of continued steroid therapy after the initial dose is unclear, but it may be considered for patients who require hospital admission for treatment.
Adrenergic agents are highly effective at reducing airway edema by rapidly constricting mucosal blood vessels and reducing vascular permeability . Due to the potential for side effects including agitation, tachycardia, and hypertension, the use of nebulized (racemic or levo-) epinephrine is commonly reserved for patients who have moderate to severe respiratory distress. The rapid onset of action of epinephrine (10–30 minutes) makes its use beneficial in these severe cases because the anti-inflammatory effects of steroids may not be appreciated for several hours after administration. A recent randomized controlled trial assessing the efficacy of levo-epinephrine in combination with systemic or inhaled steroids demonstrated significant improvement in the outcome of patients who had moderate and severe croup when treated with combination therapy . Patients treated with epinephrine need to be observed for at least 3 to 4 hours after administration due to the possibility of symptom regression after the initial beneficial effects subside.
Heliox is a low-density alternative to oxygen that is thought to improve gas flow through the compromised airway. The value of heliox in the treatment of croup has recently been assessed. In a randomized controlled trial of 29 patients, Weber and colleagues reported similar benefits from the use of heliox and racemic epinephrine.
Admission to the medical ward or ICU should be considered (1) if the patient has evidence of continued respiratory distress after initial therapy, (2) if the patient presents with severe croup, or (3) if the social situation does not permit easy access to medical care in case of worsening symptomatology. Hospital care is largely supportive, although further medical management and rarely intubation are occasionally necessary. Otolaryngology consultation should be sought when
Significant airway compromise is present
Diagnosis of croup is in question
Patient has recurrent or prolonged croup
Suspicion of bacterial tracheitis is present
Congenital or acquired airway pathology is diagnosed
Intubation should be reserved for cases of severe croup refractory to medical measures. Care must be taken to use the smallest possible endotracheal tube to avoid traumatizing the inflamed mucosa. The patient may be extubated after detection of an air leak.
Surgical management for croup is limited to MLB, as previously indicated. Tracheotomy is rarely required to secure the airway. A discussion of the surgical management of predisposing airway pathologies is beyond the scope of this article.
Summary
Over the past century, advances in the management of croup have transformed this condition from an almost certain death sentence to a relatively benign self-limited condition. A careful history and physical examination are critical to the diagnosis of croup and essential to ruling out less common conditions that mimic or presdispose to acute viral laryngotracheobronchitis. As with any airway condition, the first consideration in a patient who has croup should be rapid airway assessment and stabilization. When this step is complete, croup is almost always manageable with supportive and medical measures in the primary care or emergency room setting, with surgery reserved for diagnosis and management of complications.
Epiglottitis
Epiglottitis is an acute inflammation of the epiglottis or supraglottis that may lead to the rapid onset of life-threatening airway obstruction and is considered an otolaryngologic emergency. Since the widespread implementation of a conjugate vaccine for Haemophilus influenzae type b (Hib) nearly 2 decades ago, the incidence of epiglottitis has significantly declined in children. Securing the airway should be accomplished immediately in a controlled setting. Coordinated communication between the otolaryngologist, anesthesiologist, and intensivist is vital to the care provided to these critically ill patients.
Historical accounts of George Washington’s death suggest that he succumbed to acute epiglottitis. One early December morning in 1799, George Washington awoke with a severe sore throat. Throughout the day, his condition rapidly deteriorated as he developed difficulty in swallowing, an unintelligibly muffled voice, and persistent restlessness. Although a tracheotomy was suggested by one physician in attendance at his bedside, the procedure was not well-practiced at that time, and a series of bloodlettings were performed instead. He expired less than 24 hours from the onset of his symptoms .
Pathogenesis
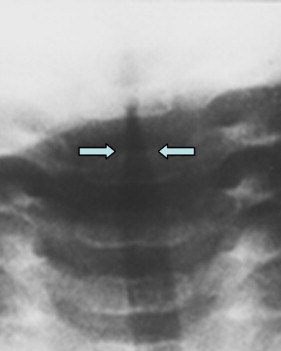
The epiglottis comprises a leaf-shaped elastic cartilage with overlying loose connective tissue and a thin epithelial layer. It arises from the posterior tongue base and covers the laryngeal inlet during swallowing. Any inflammation of the epiglottis can easily spread to the attached aryepiglottic folds and the arytenoid soft tissues, causing a more generalized supraglottitis. Bacterial invasion of the mucosa leads to fulminant infection, with rapid evolution of edema causing severe, life-threatening obstruction of the upper airway ( Fig. 2 ).