Endoscopic Surgery of The Craniocervical Junction
Adam M. Zanation
INTRODUCTION
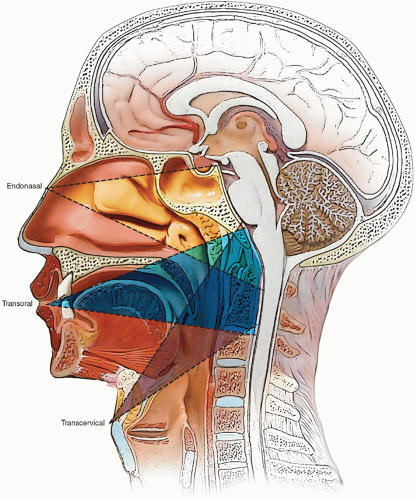
With the advent of the expanded endoscopic approach, otolaryngologists and neurosurgeons have been able to access a wide range of skull base pathology, from the crista galli down to the craniocervical junction. The transoral and transcervical approaches have been the gold standard method to access lesions located at the craniocervical junction. Since Alfieri et al. proved the feasibility of using an endoscopic endonasal approach in 2002, experienced surgeons have adopted these minimally invasive route. While all three approaches can give access to the C1/dens complex, each has its own advantages for more superior or inferior extension into the clivus or spine (Fig. 29.1).
The endonasal route has many advantages over the classic transoral route. Endonasal procedures obviate the need for splitting the hard and soft palate, a procedure which may be associated with velopharyngeal incompetence and dysphagia. Endonasal routes also avoid postoperative edema of the tongue with possible hypernasal speech and ischemic necrosis. There is also a lower probability of a need for tracheostomy and gastrostomy tube feeding. I have found that these patients can advance their diets more quickly and can be extubated earlier during their postoperative recovery.
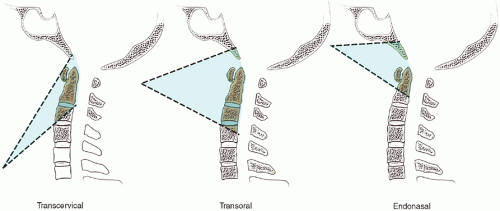
Theoretically, endonasal procedures should have a decreased rate of infectious complications (i.e., meningitis, pharyngeal cellulitis, cerebrospinal fluid [CSF] fistula) and wound dehiscence, as oral flora are not encountered. Anatomically, the endonasal approach should also provide an easier surgical corridor for those pathologic entities that are located superior to the body of C2 (Figs. 29.1 and 29.2). Patient body habitus is less of a factor with endonasal procedures, as those patients who require halo traction may wear the device during surgery.
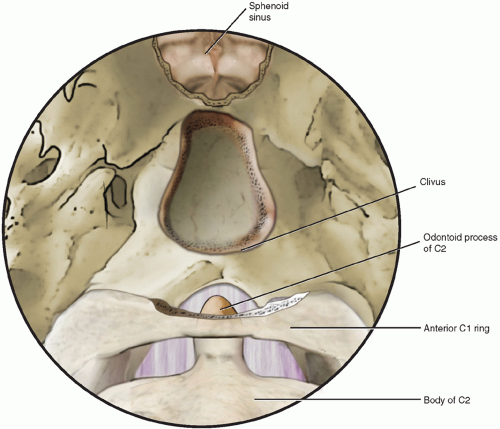
The disadvantages of the endonasal endoscopic approach include loss of the 3D open approach when using a 2D monitor and endoscope. Less exposure might be provided by the endonasal approach than the open transoral route, especially in the rostrocaudal and lateral directions. Theoretically violations of the dura may be difficult to manually repair endoscopically as compared to repairs done under an open operating microscope. The learning curve also is higher for otolaryngologists not facile with the endoscopic repair. Anatomically, the caudal limit of the endonasal approach does not permit surgery for pathology rostral to C2, whereas the transoral approach may be used down to C3 (Fig. 29.2). However, the endonasal approach has the benefit of easily accessing clival and superior direct extension (Fig. 29.3). Nasal anatomical defects might preclude endoscopic exploration, although middle turbinectomy may be employed to provide greater access. Specialized instrumentation is needed to access those lesions that are located further from the nasal aperture.
Recent studies have described combined transoral-endonasal approaches for surgery at the craniocervical junction. Because of the dearth of literature and experience with this approach, the focus of this chapter is on the endonasal approach. Regardless, there is no one approach that should be used for every patient, as every patient’s pathology and anatomy should be evaluated on a case-by-case basis. Table 29.1 highlights the benefits and limitations between the major surgical approaches to the craniocervical junction.
HISTORY
Patients with atlantoaxial instability and dysfunction may present with a wide variety of signs and symptoms. Those patients with recent trauma may present with associated head and neck lacerations and cervical whiplash. Patients with extensive cervicomedullary junction compression may present with pain or paresthesia of the neck, upper cervical spine, face, and occipital areas. General symptoms, such as fatigue, headache, and dizziness, may
be present, along with more specific symptoms of upper motor neuron injury, such as myoclonus, rigidity, hyper-reflexia, myelopathy, and dysphagia. Compression may be caused by primary or metastatic tumor, in which case symptoms may also be present at the primary site. Patients with congenital disorders may be asymptomatic until their third decades or have associated micrognathia, macroglossia, torticollis, or other pathognomonic features. Patients with rheumatologic disorders may present with systemic manifestations of the disease. Autoimmune disorders may only present with an antecedent infection. Metabolic causes may present with systemic signs, such as cardiac defects and short stature. A careful history of previous surgery must also be taken to rule out iatrogenic causes. A complete differential diagnosis for atlantoaxial instability and dysfunction is presented in Table 29.2.
be present, along with more specific symptoms of upper motor neuron injury, such as myoclonus, rigidity, hyper-reflexia, myelopathy, and dysphagia. Compression may be caused by primary or metastatic tumor, in which case symptoms may also be present at the primary site. Patients with congenital disorders may be asymptomatic until their third decades or have associated micrognathia, macroglossia, torticollis, or other pathognomonic features. Patients with rheumatologic disorders may present with systemic manifestations of the disease. Autoimmune disorders may only present with an antecedent infection. Metabolic causes may present with systemic signs, such as cardiac defects and short stature. A careful history of previous surgery must also be taken to rule out iatrogenic causes. A complete differential diagnosis for atlantoaxial instability and dysfunction is presented in Table 29.2.
TABLE 29.1 Comparison of Surgical Approaches to Craniocervical Junction Surgery | ||||||||
|---|---|---|---|---|---|---|---|---|
|