The term “
early laryngeal cancer” refers to a mucosally derived neoplastic lesion that may invade deeply into soft tissue, but not into the underlying cartilage. The majority of literature reports include carcinoma
in situ (CIS), T1 and T2 lesions in the spectrum of early laryngeal cancer. At the glottic level, early cancer implies a local lesion limited to single or multiple sites in the glottis or adjacent laryngeal subsites that might impair the cord mobility but does not cause cord fixation. Overall, these lesions display pathologic invasiveness and a potential to metastasize, which exceeds that of CIS but is less than deeply infiltrating carcinoma (
1). By contrast, early supraglottic cancer may not be confined to the primary site because of its regional metastatic behavior. Pathologic invasion of the epiglottic cartilaginous foramina, short of entering the preepiglottic space (PES), is included.
EPIDEMIOLOGY
Laryngeal cancer is the second most common type of head and neck cancer worldwide, with an estimated incidence of 151,000 cases resulting in about 82,000 deaths annually (
2). With a male-to-female ratio of 6:1, laryngeal cancer is also the 13th most common cancer in men worldwide (
2). Geographic variations in the incidence and mortality of laryngeal cancer suggest that a larger proportion of the cases occur in South-Central Asia, Eastern Asia, Central Europe, and Eastern Europe (2): incidence in the United States has declined, associated with reduced smoking (
3).
In the United States, laryngeal cancer accounts for about one-fourth of the annual cases of head and neck cancer with an estimated incidence of 12,720 cases (
4). Overall, about 60% of laryngeal cancer cases are diagnosed as
“early laryngeal cancer” and encompass the Tis, T1N0M0, or T2N0M0 categories (
5). These commonly arise from the glottis and are mostly squamous cell carcinoma (
6). Variation in site predominance, however, has been reported across ethnic groups; for example, glottic cancers appear to be the most common in Caucasians, while in African Americans, the incidence of glottic and supraglottic cancers appear to be equal (
7).
RISK FACTORS
Smoking and alcohol consumption are well-established etiologic factors for laryngeal cancers. Their combined use has been associated with a multiplicative effect for the risk of developing laryngeal cancer (
8,
9). A recent study by Hashibe et al. (
10) showed that the incidence of cancers attributable to tobacco and alcohol exposure was the highest in larynx of all head and neck cancer sites at 89%. About 5% of laryngeal cancers occur in nonsmokers and nondrinkers, suggesting that other factors such as diet, gastroesophageal reflux, previous radiation, and viral infection may also contribute (
11). Human papillomavirus types 16 and 18 have been detected in frequencies ranging from 5% to 32% of analyzed samples in laryngeal cancer (
11). Occupational exposures to wood dust, polycyclic hydrocarbons, and asbestos have also been associated with increased risk for developing laryngeal cancer (
12).
ANATOMY OF THE LARYNX
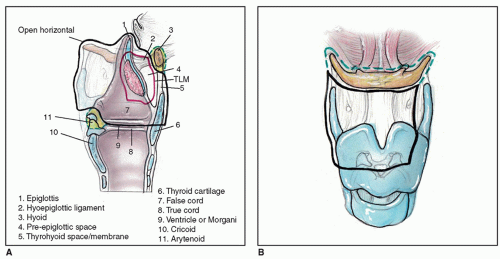
The laryngeal skeleton is composed of cartilages—thyroid, cricoid, arytenoids, epiglottis, cuneiform, and corniculate— interconnected with ligaments and membranes and moved by groups of intrinsic and extrinsic laryngeal muscles (see
Fig. 124.2).
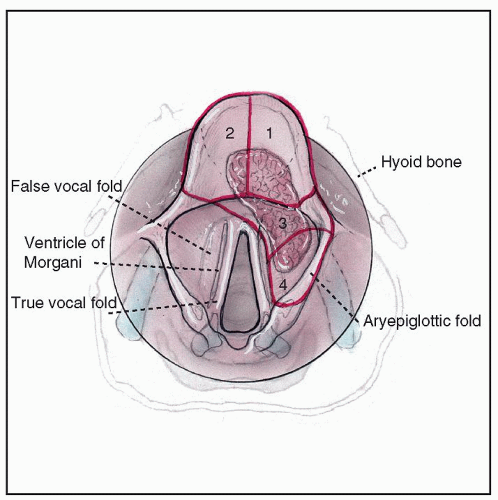
Anatomical subsites: The larynx is divided into three regions: supraglottis, glottis, and subglottis. The supraglottis extends from the epiglottis to the ventricular apices, encompassing the false cords, aryepiglottic folds, the arytenoids, and the laryngeal surface of the epiglottis. The glottis contains the true vocal cords, the anterior commissure, the interarytenoid region, and the floor of the ventricles. It extends inferiorly to 1 cm below the plane of the apex of the ventricles. The true vocal cords thicken at the anterior commissure and form the macula flava, anterior to which the ligaments merge into the Broyle tendon. The Broyle tendon, also known as anterior commissure tendon, gets inserted into the thyroid cartilage. The subglottis extends from 1 cm below the apex of ventricles to the lower border of the cricoid cartilage.
Laryngeal membranes: The conus elasticus or the cricovocal membrane arises from the inner surface of the cricoid arch and extends superiorly to attach anteriorly to the inner surface of the thyroid cartilage and posteriorly to the tip of the vocal process of arytenoids. Its free upper border thickens to form the vocal ligament. The quadrangular membrane extends between the arytenoids and epiglottis. Its upper border forms the aryepiglottic fold, while the free lower border constitutes the false cord. The thyrohyoid membrane is another fibroelastic membrane that attaches inferiorly to the upper border of the thyroid cartilage and superiorly to the posterior surface of hyoid bone.
Laryngeal spaces: Knowledge of laryngeal spaces is important to the understanding of the spread of laryngeal cancer and, therefore, planning of conservation surgical procedures. The preepiglottic space or the space of Boyer lies anterior to the infrahyoid epiglottis. It is bounded superiorly by the hyoepiglottic ligament, inferiorly by the attachment of epiglottis to the thyroid and anteriorly by the thyrohyoid membrane and upper part of the thyroid cartilage. It contains fibrofatty tissue and numerous lymphatic channels. Laterally, it merges with the paraglottic space. The paraglottic space surrounds the laryngeal ventricle and is bounded anterolaterally by the thyroid cartilage, posterolaterally by pyriform sinus mucosa, superomedially by quadrangular membrane, and inferomedially by conus elasticus. The paraglottic space provides an important route to extralaryngeal spread of cancer.
Lymphatic pathways: The supraglottis has a rich lymphatic network. The lymphatics drain primarily to the upper jugular (level II) chain of lymph nodes. It can extend to the middle (level III) and lower jugular groups (level IV), and depending on the site of tumor, cross-drainage may occur to the contralateral nodes. Lymphatic drainage from the glottis is essentially nonexistent although the cords themselves have a network of superficial mucosal lymphatics. The paratracheal (level VI) group of lymph nodes is the primary echelon of lymphatic drainage from the subglottis that may further spread to the delphian node and upper mediastinal (level VII) or the level IV nodes.
Blood supply: The arterial blood supply to the supraglottic larynx is derived from the superior laryngeal artery, a branch of the superior thyroid artery; the lower half of the larynx is supplied by the inferior laryngeal branch of the inferior thyroid artery.
Nerve supply: Sensation above the vocal fold is supplied by the internal branch of the superior laryngeal nerve, whereas the external branch provides motor supply to the cricothyroid muscles. Both sensory and motor innervations below the vocal fold are provided by the recurrent laryngeal nerve.
EARLY SUPRAGLOTTIC CANCER
Supraglottic squamous cell cancers comprise 30% to 40% of laryngeal cancers in the United States (
5,
19). The lesions are often silent in their early stages and may present with non-site-specific symptoms such as a sore throat or referred otalgia. Persistent dysphagia or aspiration does not usually manifest until the primary tumor attains significant bulk. Due to abundant lymphatic outflow, an enlarged metastatic neck node is another mode of presentation for early supraglottic tumors. The incidence of cervical metastasis at presentation, however, depends upon the T stage, location, and differentiation of the primary tumor and is reported to vary from zero to approximately 33% in T1-T2 tumors (
20).
Surgical Pathology
Whole-organ laryngeal section studies (
21,
22) and numerous clinical observations (
23,
24,
25) have postulated the supraglottic larynx as a distinct anatomic laryngeal subunit, above the true vocal cords. This compartmentalization is partly attributed to separate embryologic derivations, with the supraglottic structures emanating from branchial arches III and IV (buccopharyngeal anlage) and the glottic-subglottic structures from branchial arch VI (tracheopulmonary anlage). However, no specific anatomical structure has been identified that might act as a barrier between the supraglottic and glottic regions (
23).
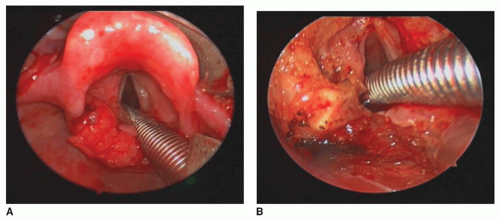
Early tumors spread within the confines of the supraglottic unit. This concept combined with an understanding of the key avenues of extension, makes supraglottic laryngectomy (SGL), endoscopic or open, a highly effective option for treatment of early-stage cancers. Infrequently, invasion of the glottis can occur when the tumor of the epiglottic petiole extends inferiorly or when extension from the undersurface of the false cord reaches the ventricle.
A certain subset of tumors arises in the (infrahyoid) angle between the epiglottis and the anterior false cord. Dubbed “engelkarzinom” by our German colleagues, this presentation may have considerable deep extension toward or into the PES.
The epiglottic perichondrium and the thyroepiglottic ligament limit anterior extension, but the tumor spreads into the fatty areolar tissue of the PES via infiltration through the epiglottic cartilage fenestrations. Involvement of PES implies a T3 stage, but insidious extension in this direction can occur in early supraglottic lesions, particularly if the tumor originates in the infrahyoid epiglottis. In the PES, there is a transition of the tumor edge from “infiltrating” to broad, “pushing” type with a pseudocapsule, probably arising from the expanded epiglottic perichondrium (
21). A tumor-free space usually exists between the hyoid bone and the advancing front of the tumor, a feature that makes preservation of the hyoid in SGL oncologically safe and functionally superior. In late tumors, extralaryngeal spread occurs when extension is observed anteriorly from the PES, breaching the thyrohyoid membrane, sometimes reaching the strap muscles. Another late route of extralaryngeal spread is through the hyoepiglottic ligament to the vallecula and tongue base superiorly. Deep lateral extension of the supraglottic tumor to the thyroid cartilage is rare; ossified cartilage has higher susceptibility to invasion. Lesions of the aryepiglottic fold may spread laterally to involve the medial wall of pyriform sinus.
Staging and Treatment Planning
A complete workup to assess the patient, the subsite and stage of primary tumor, and the presence of cervical lymphadenopathy is indicated (
Table 123.1). This includes a thorough history and physical examination, including neck palpation and fiberoptic laryngoscopy. This affords direct visualization of the tumor extent, arytenoid involvement, and cord mobility. Cord hypomobility implies paraglottic space invasion, and cord fixation upstages the primary tumor to T3.
Assessment of comorbidity, particularly, pulmonary diseases, is a crucial component of preoperative planning for conservation surgery. Patients with poor pulmonary reserve, as determined by forced expiratory volume in one second (FEV1) of greater than 75% or FEV1/FVC (functional vital capacity) ratio of less than 65%, are at greater risk of troublesome aspiration.
For T2 lesions, radiologic evaluation with computed tomography (CT) or magnetic resonance imaging (MRI) is performed to determine the extent of the primary and to rule out involvement of the PES, the paraglottic space, or the inner thyroid cortex, factors that escalate the T stage. CT, MRI, and especially gray-scale ultrasonography can reliably assess cervical lymphadenopathy, supplemented by ultrasound-guided fine-needle aspiration (FNA), if indicated. The latter is particularly useful in decision making for or against treating the contralateral neck (see “Management of the Neck”). Chest radiography, CT, or positron emission tomography (PET) is used to evaluate distant metastasis or second primary tumors in smokers.
Operative direct laryngoscopy should be performed along with photodocumentation to accurately assess the primary tumor and obtain biopsies for diagnosis and/or mapping in postradiation, recurrent cases. It also provides the opportunity to determine the suitability for a conservation procedure and decide the ideal approach—transoral or open. Occasionally, exophytic bulk conceals the accurate determination of the inferior tumor extent, whereupon rigid telescopes may be helpful. To detect synchronous primaries, a complete examination of the upper aerodigestive tract (UADT) mucosa is performed.