11 Dizziness, Imbalance, and Age-Related Vestibular Loss in the Geriatric Population
 Introduction
Introduction
Dizziness and imbalance are common conditions affecting the elderly population. They can be challenging to manage given that the symptoms can be nonspecific and may represent multiple underlying diagnoses. This chapter begins by defining dizziness and imbalance in the elderly and describing age-related vestibular loss (ARVL), which is of particular interest to the geriatric otolaryngologist. The chapter then reviews the epidemiology of dizziness, imbalance, and ARVL and discusses the physiological and pathological evidence for ARVL. Finally, the chapter reviews the evaluation and management of an older patient with dizziness and imbalance and closes with a discussion of falls risk assessment.
 Definitions of Dizziness and Imbalance in the Geriatric Population
Definitions of Dizziness and Imbalance in the Geriatric Population
Dizziness connotes a subjective perception of disorientation or involuntary motion, which can occur during movement or at rest.1 Dizziness can be subdivided further into the subtypes of vertigo and presyncopal lightheadedness. Vertigo is the false sensation that either the body or the environment is moving (usually spinning) and may be a symptom of vestibular, visual, or neurological impairment, psychological factors, or the use of multiple medications (polypharmacy). Vertigo that occurs in the elderly has been termed presbyvertigo. Presyncopal lightheadedness is the sensation of impending faint associated with transient diffuse cerebral hypoperfusion. Causal factors for lightheadedness include cardiovascular disease and orthostatic hypotension (e.g., resulting from excessive medication use or autonomic instability). Imbalance can be equated with disequilibrium, and it connotes a sense of postural instability generally associated with the trunk and legs without a sensation in the head.2 Imbalance is usually described either while standing or walking and typically does not occur at rest. Imbalance results from neuromuscular impairment related to muscle weakness, loss of peripheral sensation or proprioception, and/or arthritis. The imbalance or disequilibrium that occurs with aging has been termed presbystasis or presbyequilibrium.
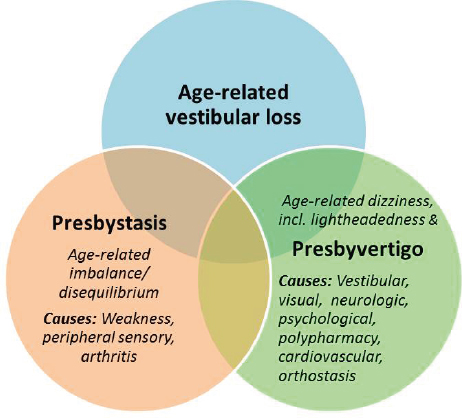
The typology of dizziness and imbalance is conceptualized in Fig. 11.1 as a set of overlapping conditions. Age-related vestibular loss (ARVL), which is in the realm of geriatric otolaryngology, is also depicted. The vestibular system plays an integral role in maintaining the vestibulo-ocular and vestibulo-spinal reflexes (VOR and VSR). The VOR is important for stabilization of gaze during head movement, and VOR impairment manifests as dizziness (i.e., abnormal sensation of motion). The VSR is important for trunk and limb stabilization during head movement. VSR dysfunction manifests as postural instability. The VOR and VSR are depicted in Fig. 11.1 as the overlap between ARVL and presbyvertigo and presbystasis, respectively. Interestingly, there is increasing recognition of the physiological importance of vestibuloautonomic projections. Vestibuloautonomic impairment has been associated with orthostatic hypotension.3 Thus ARVL may also be a causal factor for the symptom of presyncopal lightheadedness. Emerging evidence is suggesting that a certain amount of ARVL is present in older individuals but may not be manifesting symptomatically as dizziness or imbalance.4,5 This may be because the level of vestibular impairment has not crossed a critical threshold, or because an individual is able to compensate for the ARVL. ARVL is thus depicted in Fig. 11.1 as asymptomatic or “subclinical” and symptomatic or “clinical.”
As is evident in Fig. 11.1, multiple causative factors have been associated with dizziness and imbalance in the geriatric population. It is well known among researchers who study aging that geriatric conditions often result from numerous coexisting factors that may interact to have nonlinear, synergistic effects. Indeed, Tinetti and colleagues have described dizziness as a geriatric syndrome whereby symptoms result not from sole disease entities but from accumulated impairment in multiple systems.6 As a corollary, the authors suggest that the management of geriatric syndromes requires multifactorial interventions, or alternatively a focus on improving functional outcomes irrespective of the complex web of etiologic factors.
Fig. 11.1 Typology of age-related dizziness, imbalance, and vestibular loss. VOR, vestibulo-ocular reflex; VSR vestibulospinal reflex.
 Epidemiology of Dizziness, Imbalance, and Age-Related Vestibular Loss in the Geriatric Population
Epidemiology of Dizziness, Imbalance, and Age-Related Vestibular Loss in the Geriatric Population
Estimates of the prevalence of dizziness and imbalance in the geriatric population depend largely on the definitions of dizziness and imbalance used, and on the populations surveyed. Definitions vary as noted previously. The populations surveyed can vary with respect to their age ranges, whether they are population-based or clinic-based, and what types of clinics are being studied (e.g., primary vs. specialty care). Several large population-based studies have found a 20 to 30% prevalence of dizziness and imbalance in the elderly population (age ≥ 65 years).7–9 The prevalence of dizziness and imbalance rises steeply with age, with levels over 50% in the community-dwelling population over age 80.10 A study in institutionalized nursing home residents observed a prevalence of dizziness and vertigo of 68%.11 Among patients presenting to a primary care clinic, 24% reported dizziness and 17% identified dizziness as their major presenting complaint.12 Within the otolaryngology clinic, one study of 131,000 consecutive patients found that 6% of patients over age 65 presented with vertigo or a presumed vestibular diagnosis.13 Interestingly, this large-scale survey of otolaryngological practice found that visits from geriatric patients increased from 14.3% in 2004 to 17.9% in 2010. Moreover, this study noted that the five most common geriatric diagnoses were otologic (including hearing loss, external ear disorders, tinnitus, otitis media/eustachian tube disorders, and vertigo).
A landmark series of studies based in Germany estimated the population prevalence and incidence more specifically of vestibular vertigo (i.e., vertigo resulting from vestibular impairment). Community-dwelling participants in a national telephone survey were queried about symptoms of dizziness and vertigo. Those who reported moderate symptoms were administered a detailed neurotologic interview, from which vestibular vertigo was diagnosed based on symptoms of rotational vertigo, positional vertigo, or recurrent dizziness with nausea and oscillopsia or imbalance. Of note, the neurotologic interview was found to have good validity based on a gold standard of neurotology clinic–based diagnosis in establishing a vestibular diagnosis. The lifetime prevalence, 1-year prevalence, and incidence of vestibular vertigo were observed to be 7.8%, 4.9%, and 1.5%, respectively.14 The 1-year prevalence of vestibular vertigo increased with age to 7.2% in those aged 60 to 69 and 8.8% in individuals over age 80. This study was among the first to estimate the population prevalence of ARVL.
A more recent study estimated the prevalence of vestibular impairment in the U.S. population using an objective, rather than subjective (self-report based), test. Data were drawn from the 2001–2004 National Health and Nutrition Examination Survey (NHANES). Vestibular function was assessed in NHANES using the modified Romberg test, whereby vestibular impairment was inferred from an inability to stand on a foam pad with eyes closed. Thirty-five percent of U.S. adults age 40 years and older had evidence of balance dysfunction based on this postural metric.4 The odds of balance dysfunction increased significantly with age, such that 85% of individuals age 80 and above had evidence of balance dysfunction. These estimates are considerably higher than the prevalences of vestibular vertigo mentioned earlier from the German population. It is possible that the symptom of vestibular vertigo represents a component of clinical ARVL, whereas vestibular impairment based on the modified Romberg test represents subclinical ARVL.
Epidemiological analyses of dizziness, imbalance. and ARVL have also investigated risk factors for these conditions. Most studies have observed an increased prevalence of dizziness and imbalance in women.1 Vestibular vertigo was also more prevalent in women.15 However, the prevalence of vestibular impairment based on objective modified Romberg testing did not differ by gender.4 Findings from a review of the most frequently reported causes of dizziness in primary care practice are presented in Table 11.1.1 The review found that peripheral vestibular disease was the most common cause of dizziness, observed in 20 to 50% of cases. Peripheral vestibular diseases included benign paroxysmal positional vertigo (BPPV), labyrinthitis, and vestibular neuritis. Other common causes of dizziness were cardiovascular disease, systemic infection (leading to orthostatic hypotension), psychiatric disorders, metabolic disturbances, and use of multiple medications. A more recent epidemiological survey of the elderly population in England found that dizziness was associated with abnormal heart rhythm, hearing loss, vision loss, and low grip strength, whereas imbalance was associated with diabetes, arthritis, low grip strength, and vision loss.8 With respect to vestibular vertigo, independent risk factors were depression, tinnitus, and cardiovascular risk factors, including hypertension and dyslipidemia.14 Finally, independent risk factors for vestibular impairment as measured by the modified Romberg test included low socioeconomic status and diabetes mellitus.4,16
Epidemiological studies also have examined the impact of dizziness, imbalance, and ARVL on diverse outcomes, including falls, quality of life, health care utilization, and other economic outcomes. Dizziness has been associated with a two- to threefold increased risk of falling.4,10 Specifically with respect to ARVL, the study from NHANES found that individuals with objective vestibular impairment who were also clinically symptomatic (i.e., reported dizziness) had a 12-fold increase in the odds of falling. In a small pilot study, older fallers were found to have significantly higher rates of peripheral vestibular dysfunction than older nonfallers.17 A prospective study reported that elderly patients with vestibular asymmetry were significantly more likely to experience an incident fall.18 Moreover, several studies have observed an association between vestibular asymmetry and fall-related hip and wrist fracture risk.19–21
Table 11.1 Most common causes of dizziness in primary care practice
Category | Percent | Examples |
Peripheral vestibular disease | 20–50 | Benign paroxysmal positional vertigo (BPPV), labyrinthitis, vestibular neuritis |
Cardiovascular disease | 10–30 | Arrhythmia, congestive heart failure, vasovagal conditions (e.g., carotid sinus hypersensitivity) |
Systemic infection | 10–20 | Systemic viral and bacterial infection |
Psychiatric conditions | 5–15 | Depression, anxiety, hyperventilation |
Metabolic disturbances | 5–10 | Hypoglycemia, hyperglycemia, electrolyte disturbances, thyrotoxicosis, anemia |
Medications | 5–10 | Antihypertensives, psychotropic medications |
Data from Sloane PD, Coeytaux RR, Beck RS, Dallara J. Dizziness: state of the science. Ann Intern Med 2001;134(9 Pt 2):823–832. | ||
Quality of life measures assess general quality of life (e.g., the Short-Form Health Survey [SF-36]) as well as health-related quality of life (i.e., related to a specific health condition). Dizziness and vestibular vertigo have been associated with significantly poorer quality of life, in both the physical and the mental domains. One population-based study in Sweden found that dizziness was one of the most influential symptoms affecting general quality of life in older individuals.22 The most widely used measures of dizziness- and imbalance-related quality of life are the Dizziness Handicap Inventory (DHI),23 the Activities Balance Confidence (ABC) scale,24 and the Falls Efficacy scale (which measures fear of falling).25 Two studies that administered the DHI in patients presenting with dizziness to a primary care clinic and a specialized dizziness clinic found that over 60% of patients reported moderate to severe handicap associated with their dizziness in both clinical contexts.26,27 With respect to health care utilization and economic outcomes, the German population-based study found that vestibular vertigo was more likely than nonvestibular vertigo to be associated with a medical consultation, sick leave, interruption of daily activities, and avoidance of leaving the house.28 Similarly, a population-based study in the United States observed that 50% of older individuals with dizziness and balance problems saw at least one medical provider, and 35% saw three or more providers.29 A single provocative longitudinal study found that patients with disequilibrium at baseline were at significantly increased risk only for new-onset cognitive decline compared with controls.30
The epidemiological data reviewed thus far suggest that dizziness, imbalance, and ARVL are prevalent in the population and have significant clinical, functional, and economic implications. Several final points deserve mention at the conclusion of this section. First, as has been highlighted by numerous authors, the goal of research on dizziness and imbalance in the geriatric population should be the development of evidence-based clinical practice guidelines for the effective diagnosis and management of these conditions.1 To this end, the use of a common nomenclature is an important first step. Second, although dizziness and imbalance are prevalent in the geriatric population they are not universal. As one study specifically points out, not all individuals over age 90 had dizziness.10 As such, dizziness and imbalance in the geriatric population may be considered “age-concomitant” rather than “age-dependent” conditions.10 As a corollary, these conditions should be viewed as pathological, and efforts should be made to treat them. Finally, it follows that the potential scope of managing dizziness and imbalance in the geriatric population is enormous, likely far exceeding the capacity of geriatricians and otologists.11 Thus it might be necessary to train other types of health care professionals such as nurses and physical therapists to assist more in managing these conditions.
 Physiological and Pathological Evidence for Age-Related Vestibular Loss
Physiological and Pathological Evidence for Age-Related Vestibular Loss
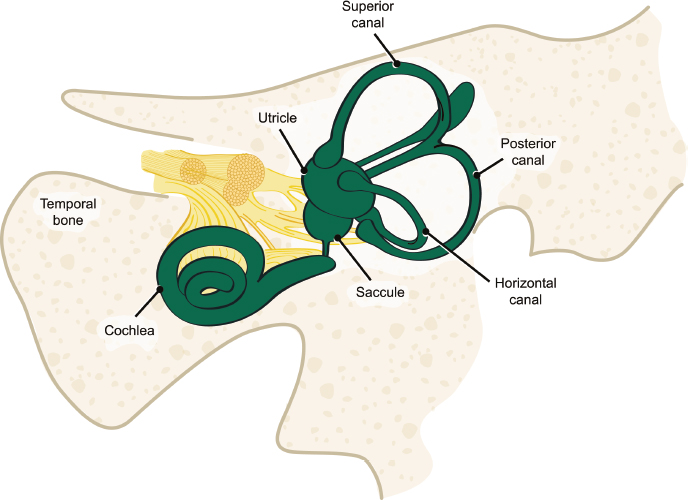
As already described, there is epidemiological evidence that ARVL is prevalent in the geriatric population. The vestibular system consists of five organs: three semicircular canals (anterior or superior, posterior and horizontal, or lateral), and two otolith organs—the saccule and the utricle (Fig. 11.2). The semicircular canals detect angular head rotations along the planes of the canals, whereas the otoliths detect linear translations of the head, as well as head orientation with respect to gravity. The saccular neuroepithelium is oriented in a vertical direction and preferentially detects vertical linear head movements, whereas the utricular neuroepithelium is horizontally oriented and preferentially detects horizontal head movements.
In recent years, numerous vestibular physiological tests have been developed that allow for localization of dysfunction within the five organs of the vestibular system. The most widely used vestibular tests are caloric and rotational chair testing, which evaluate the function of the horizontal semicircular canal.31 Recently, video-oculography techniques have made possible quantitative angular vestibulo-ocular reflex (AVOR) testing during head impulses to assess the function of each of the six semicircular canals.32,33 The vestibular-evoked myogenic potential (VEMP) tests are gaining increasing popularity as measures of otolith function. The sound-evoked cervical VEMP (cVEMP) is a product of the sacculocollic reflex and is thought to specifically reflect saccular function.34 The vibration-evoked ocular VEMP (oVEMP) has been suggested to selectively measure utricular function.35
Several classic studies have reported a decline in horizontal semicircular canal function with aging. Peterka and colleagues tested over 200 healthy subjects across a wide age range (7–81 years) and observed increased postural sway and decreased VOR gain to sinusoidal rotation with age.36 Caloric responses, however, were not observed to change with age. Paige similarly observed declining VOR responses with age to high-amplitude and highvelocity sinusoidal rotations in 81 patients age 18 to 89.37 The author concluded that “aging entails a progressive bilateral peripheral vestibular loss.” Baloh and colleagues completed one of the only longitudinal studies of vestibular function in 57 normal older individuals who were followed annually for 5 years.38 They observed a significant decrease over the 5 years in VOR gain to sinusoidal stimuli, again only at higher velocities.5 Interestingly, none of the older individuals reported symptoms of dizziness or imbalance. It is possible that a threshold of ARVL must be crossed for the disease to move from being subclinical to clinical.
In addition to age-related declines in semicircular canal function, studies also suggest that otolith function decreases with age. Welgampola and Colebatch performed cVEMP testing in 70 adults age 25 to 85.39 They observed decreasing click-evoked response amplitudes with age, notably a 25 to 30% decline in amplitude per decade from the sixth decade. Brantberg and colleagues measured tone-burst evoked cVEMPs in 1,000 consecutive patients seen in their clinic and observed a steady decline with age starting as early as age 40.40 A pilot study of 50 healthy older individuals age 70 and over evaluated the five vestibular end-organs simultaneously to assess which if any organ was disproportionately affected.41 The study observed that 80 to 90% of subjects had semicircular canal dysfunction, whereas only 50% of participants had abnormal saccular function and 20% had utricular impairment.
Histopathological analyses of human temporal bones also demonstrate the adverse effects of age, demonstrating declines in vestibular hair cell populations and progressive otoconial degeneration associated with aging.42–44 Interestingly, findings from temporal bone specimens corroborate the foregoing physiological data, demonstrating a greater loss of vestibular hair cells in the cristae ampullares of the semicircular canals relative to the otolithic maculae.45
 Evaluation and Management of an Older Patient with Dizziness and Imbalance
Evaluation and Management of an Older Patient with Dizziness and Imbalance
It is critical to take a systematic approach in the evaluation of an older patient with dizziness or imbalance. Some older individuals may report primarily vertigo, lightheadedness, or disequilibrium, which can suggest the predominance of certain underlying etiologies. However, it should be noted that older patients often have multiple concomitant impairments, such as low vision (e.g., from presbyopia or macular degeneration), cardiovascular disease (e.g., hypertension), muscle weakness, and arthritis, and the use of multiple medications. Although a particular impairment may predominate, it is possible that this impairment in combination with another deficit creates the clinical problem (i.e., the clinical problem is multifactorial). Accordingly, it is critical that the most common contributors to dizziness and imbalance in the elderly be addressed systematically every time in every patient.
The first step in the otolaryngologist’s evaluation of an elderly patient with dizziness and imbalance is to obtain a history. This includes asking when the symptoms started, whether the symptoms are progressive, how the patient would further characterize the symptoms (vertigo, lightheadedness, and/or imbalance), whether the symptoms are constant versus episodic (if episodic whether the duration is seconds, minutes, hours, or days), and whether the episodes occur at rest or only during head movement, standing, or walking. Of the major vestibular diagnoses, BPPV is particularly common in older adults and bears special mention. Increased BPPV in the elderly may reflect age-related degeneration of the otoconial membrane, leading to abnormal seeding of otoconia in the endolymph.46 A study of the German population observed a prevalence of 3.4% in individuals over age 60 and a cumulative lifetime incidence of almost 10% by age 80.47 BPPV accounted for 39% of cases of vertigo in older patients presenting to neurotology clinics.48 However, older patients do not always experience the classic presentation of BPPV—short episodes of rotatory vertigo associated with changes in head position. A study of 100 older patients presenting to general geriatric practices for chronic medical conditions found that 9% had unrecognized BPPV.49 Moreover, patients with BPPV had significantly increased fall risk. Another study found that older patients with BPPV were more likely to experience postural instability.50 Of note, this instability could be improved through canalith repositioning maneuvers.
The next step is to elicit a medical history to understand the multiple factors that might be contributing to the patient’s dizziness. Specifically, the following conditions should be noted: (1) eye disorders (e.g., cataracts, macular degeneration, or glaucoma), (2) cardiovascular disease (e.g., hypertension, arrhythmias, syncope), (3) musculoskeletal disorders (e.g., arthritis, weakness), (4) peripheral sensory loss (e.g., neuropathy), (5) psychiatric disease (e.g., depression, anxiety), (6) cognitive impairment, and (7) systemic conditions (e.g., diabetes). If any unrecognized nonvestibular impairment is identified, an appropriate referral should be made. The otolaryngologist should also ask about a history of hearing loss. Emerging evidence is suggesting a link between hearing loss, imbalance, and elevated fall risk.51
The otolaryngologist should then review the patient’s medications. Polypharmacy (i.e., the use of four or more medications) contributing to dizziness is a particular concern among older individuals. A study in the ambulatory adult population age 65 or older found that 44% of men and 57% of women take five or more medications.52 Moreover, older adults metabolize drugs differently than younger adults and may be exposed to higher drug levels at the usual doses. An increase in the number of medications used in the elderly has been associated with an increased risk of impaired balance.53 Certain classes of medications, including antihypertensive, psychotropic, and narcotic pain medications, have been associated with a particularly increased risk of dizziness and falls and have been termed fall risk–increasing drugs (FRIDs).54–56 Several clinical tools have been developed to evaluate potentially inappropriate medication use in older patients. The Beers criteria is the most commonly used tool.57 It contains of one list of medications that should be avoided independent of diagnosis, and a second list of medications that should be avoided considering the diagnosis. Further tools have been developed, including the Screening Tool of Older People’s potentially inappropriate Prescriptions) (STOPP) criteria, which enumerate medications to be avoided by organ system, and the Screening Tool to Alert doctors to Right Treatments (START) criteria, which list medications that should be recommended in older patients according to condition in the absence of any contraindications.57
With respect to the physical examination, we recommend screening for orthostatic hypotension (a systolic blood pressure decrease of at least 20 mm Hg or a diastolic blood pressure decrease of at least 10 mm Hg within 3 minutes of standing). Evidence of orthostasis could indicate excessive dose of antihypertensive medications (among other conditions) and should prompt referral to the primary care provider or cardiologist. Eye movements should be assessed, particularly the cardinal movements of smooth pursuit, saccade, and vergence. Deficits may indicate brainstem or cerebellar pathology and should prompt a referral to a neurologist. Cerebellar function should also be assessed with maneuvers such as the finger-nose-finger test, the rapid alternating hand movement test and heel-to-shin test. Deficits in any of these tests may indicate cerebellar dysfunction and should prompt referral to a neurologist.
Clinical vestibular testing should include assessment for spontaneous nystagmus (which would indicate vestibular asymmetry), postheadshaking nystagmus (which would indicate a latent vestibular asymmetry), and the horizontal head impulse test (HIT) (which evaluates horizontal semicircular canal function). One study showed that 50% of older adults age 70 and older had an abnormal HIT.58 Clinical testing should also include the Dix-Hallpike test to evaluate for BPPV, which, as mentioned previously, is very common in older individuals and is treatable. The Romberg test should be performed with eyes closed on foam to evaluate standing balance in the absence of vision and proprioceptive information (such that the patient is relying only on vestibular information). The patient’s gait should also be observed, to assess stability and the potential need for physical therapy and/or an assistive device. The timed up and go (TUG) test is an efficient and reproducible measure of fall risk. The patient is asked to stand from a seated position, walk 3 m, turn around, then return to sitting. Older adults who take longer than 14 seconds to complete the TUG are at significantly increased risk of falling.59
At present, the mainstays of management of the older patient with dizziness or imbalance seen in the otolaryngology clinic are management of polypharmacy, identification of nonvestibular contributors and appropriate referrals, management of hearing loss, home safety modification (including installing night lights and grab bars, removing throw rugs, and creating clear passageways within the home), use of assistive devices (cane and walker), and exercise programs (e.g., tai chi, or even light walking). For older patients with evidence of vestibular impairment, vestibular rehabilitation is the primary treatment. Vestibular rehabilitation is a program whereby patients learn to compensate for their vestibular loss by using visual or proprioceptive cues under the direction of a therapist.60,61 Studies have shown that vestibular rehabilitation is as effective in older patients as in younger patients.62 One randomized, controlled trial administered vestibular rehabilitation to a group of older patients with chronic dizziness seen in primary care clinics.63 The study found that vestibular rehabilitation significantly reduced dizziness symptoms and improved postural stability and dizziness-related quality of life. This trial is among the first to administer vestibular rehabilitation in primary care patients who did not have a specific vestibular diagnosis (except perhaps ARVL). Further research is needed to establish the appropriate timing for vestibular rehabilitation. Evidence that vestibular function starts to decline in middle age suggests the potential benefit of vestibular exercises prior to the onset of significant vestibular loss.11 This phenomenon has been termed prerehabilitation, or “prehab.”2 More recent studies have investigated the benefit of biofeedback prostheses in the treatment of vestibular impairment. The prostheses consist of body-worn devices that deliver sensory feedback (e.g., vibrotactile, auditory) to patients to orient the trunk during movement.64–68 Early reports are promising that the prostheses effectively improve dizziness and imbalance. Additionally, the multichannel implantable vestibular prosthesis represents a potential new technology for the treatment of ARVL that is awaiting human trials.69
Finally, pharmacological therapies for dizziness should be used judiciously and sparingly in older individuals. The most commonly-used medications to treat dizziness are vestibular suppressants, which include antihistamines (e.g., meclizine), anticholinergics (e.g., scopolamine), and benzodiazepines (e.g., lorazepam).70 Vestibular suppressants can be effective in reducing symptoms of vertigo and motion sickness. However, they have been shown to blunt the error signal that drives vestibular compensation.71 As such, vestibular suppressants are not indicated in the setting of chronic, progressive vestibular impairment (e.g., ARVL) where compensation is critical. Moreover, vestibular suppressants have sedating effects and are metabolized and cleared more slowly in older individuals.72 Thus they are not recommended in the elderly; indeed, antihistamines, anticholinergics, and benzodiazepines are listed in the Beers criteria. Interventions that challenge the vestibular system and foster compensation—such as vestibular therapy—are preferable to treat dizziness and imbalance in the elderly.
 Falls Risk Assessment
Falls Risk Assessment
The American Geriatrics Society (AGS) recommends that all patients older than age 65 with a history of falls or a balance and gait disorder should undergo multifactorial falls risk evaluation.73 If the opportunity exists, otolaryngologists should consider joining or developing multidisciplinary teams that provide multifactorial falls risk evaluation to older patients. Such a multidisciplinary falls prevention clinic has been established at the first author’s (YA’s) institution. All patients seen in the clinic are given a standardized questionnaire (Appendix). The questionnaire was developed based on AGS guidelines and with input from a multidisciplinary group of providers at the institution, including geriatricians, neurologists, otolaryngologists, ophthalmologists, orthopedists, cardiologists, physiatrists, psychiatrists, and physical and occupational therapists. Notably, the questionnaire quantifies fall history with the use of a falls severity grading scale developed in the clinic.74 Additionally, standard batteries such as the Geriatric Depression Scale, the Activities Balance Confidence Scale, the Lawton Instrumental Activities of Daily Living Scale, and the Falls Efficacy Scale are administered to measure the impact of imbalance and falls risk on the patient’s functional status and quality of life.24,25,75,76
A standardized physical examination was also developed for patients seen in the falls prevention clinic (Table 11.2), using measures in wide clinical and research use such as the Balance Evaluations Systems Test (the Mini-BEST), the Scale for the Assessment and Rating of Ataxia (SARA), and the Montreal Cognitive Assessment (MOCA).77–79 Vestibular testing is performed in all patients, including assessment of spontaneous nystagmus, gaze-evoked nystagmus, postheadshake nystagmus, visual VOR suppression, Dix-Hallpike test, and HIT using video-oculography. We also evaluate the other key contributors to fall risk, including vision loss (specifically loss of contrast sensitivity),80–82 peripheral sensory loss (particularly loss of joint proprioception),83,84 muscle weakness (particularly of the lower limbs),85,86 and neurocognitive decline (including loss of cerebellar and cognitive function).87–89 All patients receive personalized counseling on home modification and the need for assistive devices and are prescribed a program of physical and/or occupational therapy as needed. The screening questionnaire is used to direct any specialty referrals (e.g., to neurology, otolaryngology, or ophthalmology).
Table 11.2 Standard physical examination administered in the Johns Hopkins Falls Prevention Clinic: physical therapy and occupational therapy components
Physical therapy component | Occupational therapy component |
– Orthostatic vital signs – Contrast sensitivity – Vestibular and oculomotor testing using video-Frenzel lenses – Upper and lower extremity strength testing – Mini-BEST (Balance Evaluations Systems Test) | – Distal sensory testing (pinprick, joint proprioception, vibration) – Reflex testing (brachioradialis, patella, Achilles, Babinski) – Montreal Cognitive Assessment – Scale for the Assessment and Rating of Ataxia – Home assessment |
 Conclusion
Conclusion
As the population ages, increasingly otolaryngologists will be called on to manage the common geriatric problem of dizziness. This chapter reviews a nomenclature for dizziness and imbalance conditions in the elderly and emphasizes the need for a systematic approach to this multifactorial problem. Otolaryngologists should recognize the high prevalence of dizziness in the elderly, its potentially profound impact on quality of life and even length of life (shortened by fall injuries), and the availability of treatment to improve symptoms. Most older patients with dizziness can be helped, but first we must recognize them and treat them with enthusiasm and knowledge.
 References
References
15. Neuhauser HK. Epidemiology of vertigo. Curr Opin Neurol 2007;20(1):40–46
18. Ekvall Hansson E, Magnusson M. Vestibular asymmetry predicts falls among elderly patients with multi- sensory dizziness. BMC Geriatr 2013;13(1):77
61. Krebs DE, Gill-Body KM, Riley PO, Parker SW. Double-blind, placebo-controlled trial of rehabilitation for bilateral vestibular hypofunction: preliminary report. Otolaryngol Head Neck Surg 1993;109(4):735–741
71. Zee DS. Perspectives on the pharmacotherapy of vertigo. Arch Otolaryngol 1985;111(9):609–612