11 Cushing’s Disease
Cushing’s disease (CD) is generally recognized as being best treated with surgery. Careful preoperative assessment and good surgical technique are the most reliable methods of achieving the optimal outcome: elimination of hypercortisolism, permanent eradication of the tumor, and preservation of pituitary function while avoiding complications. Depending on the surgeon’s experience and the specific characteristics of the lesion, one can often feel confident in offering the patient a likely cure while preserving normal pituitary function. If surgery alone is unsuccessful, in almost all patients hypercortisolism can be eliminated with irradiation therapy or bilateral adrenalectomy. To better convey our surgical strategy for the treatment of patients with CD, we first discuss the preoperative evaluation of patients with Cushing’s syndrome, as well as the histopathologic findings that form the basis of our surgical technique.
 Pathology
Pathology
Cushing’s disease is caused by an adrenocorticotropic hormone (ACTH)-secreting adenoma. As such, the adenomas stain for ACTH using immunohistochemistry and, as with other types of pituitary tumors, they are monoclonal in origin.1 They disrupt the normal acinar pattern of the gland when stained for reticulin. When no definite tumor is identified at surgery and partial or total hypophysectomy is performed, the tissue specimen is examined using closely spaced sequential slices because tumors as small as 1 mm in diameter or less can be the source of CD. In the event that no tumor is found, the diagnosis of corticotroph hyperplasia is entertained if there is histologic evidence of hyperplasia, and a peripheral venous level of corticotropin-releasing hormone (CRH) is obtained to assess this possibility further. In the experience of the senior author, corticotroph hyperplasia is exceedingly rare (only two suspected, but unproven, cases from over 900 operations for CD). In the presence of sustained hypercortisolism a unique cytoplasmic staining pattern, known as Crooke’s hyaline change, occurs in the normal corticotrophs of the pituitary from which ACTH production has been shut down. The “hyaline” is composed of intracytoplasmic microfilaments that do not stain for ACTH. Crooke’s changes may also be found in the ACTH-staining cells of the adenoma itself.
It is important to note that pituitary adenomas compress the immediately adjacent normal anterior lobe, producing a histologic pseudocapsule, which has surgical implications. Although the presence of a histologic pseudocapsule around pituitary tumors was noted in the early 1900s, until recently the sequence of the stages of its development was unexplored. In 2006 a study reported the examination of pseudocapsule development by histologic analysis of portions of pituitary glands removed during operations for CD in patients in whom no adenoma could be identified during surgery.2 The distribution of tumor size and its relation to the presence of a histologic pseudocapsule were examined. A multilayered reticulin capsule occurred in tumors that exceeded 2 to 3 mm in maximum diameter. For tumors 1 mm or smaller, there was no reticulin capsule. The absence of this reticulin capsule in cases of very small tumors contributes to difficulty with their identification during surgical exploration of the pituitary gland in patients with CD and negative magnetic resonance imaging (MRI). On the other hand, for lesions larger than 2 mm the presence of the pseudocapsule enveloping the adenoma contributes to the identification of microadenomas buried in the pituitary gland during surgery, even in patients with negative MRI, and allows consistency of complete tumor excision.2–4
 Diagnosis
Diagnosis
It is imperative to have complete and accurate diagnostic testing before surgery is considered. The most commonly used tests to detect hypercortisolism, and establish the presence of Cushing’s syndrome, are serial 24-hour urine free cortisol (UFC) measurements to establish excess cortisol secretion, diurnal plasma cortisol levels, or evening salivary cortisol levels to detect loss of diurnal rhythm of cortisol secretion, and the overnight low-dose dexamethasone suppression test to detect a relative resistance to negative feed-back by glucocorticoids.
The UFC measurements are assayed using a variety of techniques. The normal upper levels vary with the technique used and with the laboratory performing the assay. Hypercortisolism is associated with the loss of normal diurnal variation in cortisol secretion, which is demonstrated by obtaining morning (8 to 9 a.m.) and evening (11 p.m. to 12 midnight) plasma cortisol levels. Salivary cortisol levels are also reliably used for this purpose and are well suited for outpatient screening of adult and pediatric patients for hypercortisolism.5 A study of more than 140 patients demonstrated a sensitivity of 93% and a specificity of 100% using this test to determine the presence of Cushing’s syndrome.6
The low-dose (1-mg) dexamethasone suppression test is commonly used to detect abnormal regulation of cortisol secretion. The overnight test, rather than the 2-day test, is the most commonly used test today. In persons with a normal hypothalamic-pituitary-adrenal axis, morning cortisol levels are suppressed by the overnight low-dose dexamethasone suppression test (1.0 mg given the night before a morning [7 to 8 a.m.] cortisol measurement). A morning plasma cortisol level greater than 1.8 μg/dL after the bedtime (11 p.m.) administration of 1 mg of dexamethasone detects most patients with Cushing’s syndrome and justifies further diagnostic evaluation.7
When hypercortisolism has been found, one must determine whether the process is ACTH-dependent or ACTH-independent. With Cushing’s disease or ectopic ACTH secretion, the ACTH levels will be normal or elevated. In contrast, in adrenal disease, because of the negative feedback of the high cortisol levels on hypothalamic CRH production and secretion and on pituitary ACTH production and secretion, plasma ACTH is undetectable or low (<5 pg/mL) relative to the degree of glucocorticoid secretion. For this reason, these two entities are categorized as ACTH-dependent, in contrast with adrenal tumors in ACTH-independent Cushing’s syndrome, as the adrenal cortical cortisol secretion is autonomous.
In patients with Cushing’s syndrome the differential diagnosis of Cushing’s disease from adrenal disease and ectopic ACTH secretion can be accomplished through the high-dose overnight dexamethasone suppression test. For this test, 8 mg of dexamethasone is administered orally at 11 p.m. and morning (7 to 8 a.m.) plasma cortisol measurements are obtained; suppression of morning serum cortisol of greater than 68% is required to assign a diagnosis of CD,8,9 although greater sensitivity is obtained if more than 90% suppression is used.
The CRH stimulation test is also used to differentiate between ectopic ACTH-secretion and an ACTH-secreting pituitary tumor.10–12 Because ACTH secreting adenomas are well-differentiated tumors derived from pituitary corticotrophs, most ACTH-secreting adenomas respond to CRH. Ectopic tumors, not being derived from pituitary tissue, do not express receptors for CRH and therefore do not respond to it. The sensitivity and specificity of the test are optimal using ≥35% for the maximum ACTH response from the 15- or 30-minute samples to indicate Cushing’s disease.13
The presence of ACTH-dependent hypercortisolism leads to an MRI focused on the sella. In many patients with CD a high-resolution pituitary MRI will demonstrate the presence and location of a pituitary tumor. However, a negative MRI does not rule out an adenoma. The false-negative rate using the standard T1-weighted spin echo after contrast enhancement in Cushing’s disease is as high as 40 to 50% at many centers (Fig. 11.1).14
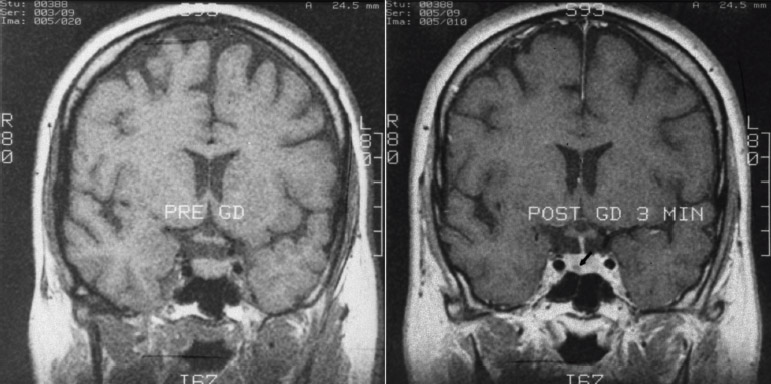
Fig. 11.1 Pre– and post—gadolinium-enhanced coronal spoiled gradient (SPGR) magnetic resonance imaging scan demonstrating an adenoma in the right anterior aspect of the pituitary gland. The SPGR technique with 1-mm cuts has improved sensitivity in finding small adenomas.
If the high-dose dexamethasone suppression test and the CRH stimulation test are consistent with CD and the pituitary MRI reveals an adenoma, no further diagnostic testing is necessary. However, if either of the provocative endocrine tests is inconsistent with CD, or the MRI does not reveal an adenoma, inferior petrosal sinus sampling (IPSS) is performed. IPSS has the greatest diagnostic accuracy of the available tests for the differential diagnosis of CD versus ectopic ACTH syndrome.15 By placing catheters into the inferior petrosal sinuses and a peripheral vein, one can obtain simultaneous samples for central and peripheral plasma ACTH concentrations at 2 and 0 minutes before and 3, 5, and 10 minutes after intravenous CRH administration (1 μg/kg body weight). IPSS is used only in patients with confirmed hypercortisolism, as the test cannot discriminate between normal subjects and patients with CD. Because this is an invasive procedure with rare but serious associated risks,16 it is reserved for patients in whom the results of provocative endocrine testing are conflicting or equivocal and in instances where there is no lesion found on MRI. A peak central ACTH concentration to peripheral ACTH concentration ratio of 2:1 during baseline (before CRH) or 3:1 before or after CRH is diagnostic of CD.15 Although reports of false-negative results exist,17 these are often due to improper placement of the catheter tips, and in our experience the diagnostic accuracy approaches 100% in patients who undergo successful sampling bilaterally. Because the accuracy of the test relies on successful placement of the catheter tips in the inferior petrosal sinuses bilaterally, venography is performed to confirm placement and evaluate the venous anatomy. It is important to note that IPSS does not reliably allow lateralization of MRI-negative adenomas, as the lateralization accuracy is only approximately 70% in patients with microadenomas identified at surgery, compromising its usefulness as a localizing measure during surgery.15
 Imaging
Imaging
Magnetic resonance imaging is the imaging modality of choice for detection of pituitary adenomas. Aside from detecting the presence of tumors and defining their anatomy, MRI provides anatomical information that is useful during the surgical approach. In particular, the anatomy of the sphenoid sinus and the parasellar anatomy, and the location of the carotid arteries can be assessed from an MRI scan. Recently the spoiled gradient recalled acquisition technique, used with 1-mm nonoverlapping slices, was shown to be more sensitive than the conventional spin echo approach (sensitivity 80% versus 49%) in detecting adenomas in patients with CD.18 Because the sensitivity of the conventional MRI techniques (spin echo) for CD (Fig. 11.1) is only 50 to 75%,19–22 many patients have a negative MRI. When interpreting the results of an MRI scan, one must keep in mind that pituitary adenomas are found incidentally in 10% of normal volunteers and in 5 to 20% of random autopsy specimens. Incidental adenomas may also be identified during surgery.23,24 It is therefore important to establish the diagnosis of CD through endocrine testing before performing surgery.
 Surgery
Surgery
As discussed previously in the pathology section, the pseudocapsule can be used as a surgical capsule in the surgical treatment of microadenomas. The discussion in this section reflects the surgical technique of the senior author, which has been developed over several years of experience.
Initially a wide, bloodless exposure of the sella is established. Using a drill with a 3- to 4-mm bur, the bone covering the anterior and inferior surfaces of the sella is thinned to less than 0.5-mm thickness, and then an initial opening of the anterior face of the sella turcica (Fig. 11.2) is performed. In patients with a positive MRI, the initial opening is made away from the tumor, over the normal anterior lobe. A 2-mm Kerrison rongeur with a thin distal lip (0.75 mm) is used to remove the remaining thin layer of bone of the anterior sella face in small increments. The bone is removed laterally until at least 2 mm of the most medial aspect of each cavernous sinus is visible. Superiorly bone removal extends to the tuberculum sellae. Inferiorly, a disk dissector is used to separate gently the dura from the bone of the sella floor after the anterior face of the sella has been removed. The sella floor is then removed with a small pituitary rongeur. Oozing bone margins are covered with a thin layer of bone wax. Because of the very low pressure in the cavernous sinus and the smaller dural veins draining into it, the same technique, or placement of small pieces of Gelfoam soaked in thrombin, can be used successfully for any site that slowly oozes blood from the layer between the dura and bone at the margins of the bone removal. At this stage the operative field should be bloodless and should expose the entire anterior sella dura and most of the inferior dura covering the pituitary. Inspection of the dura reveals any region of invasion of the anterior or inferior dura. In cases of small tumors that reach the anterior surface of the pituitary gland, careful examination of the dural surface may provide clues to the site of the tumor. Coagulation of the dura is avoided during the exposure because it tends to adhere the dura to the underlying pituitary capsule and because coagulation produces a region of white discoloration of the pituitary capsule and the contiguous region of gland immediately beneath it, a change in color that may be misleading in the search for small, gray-white adenomas of CD. The dura is opened using a no. 15 scalpel, with care taken to make the incision completely through the dura but not to enter the capsule of the pituitary gland.
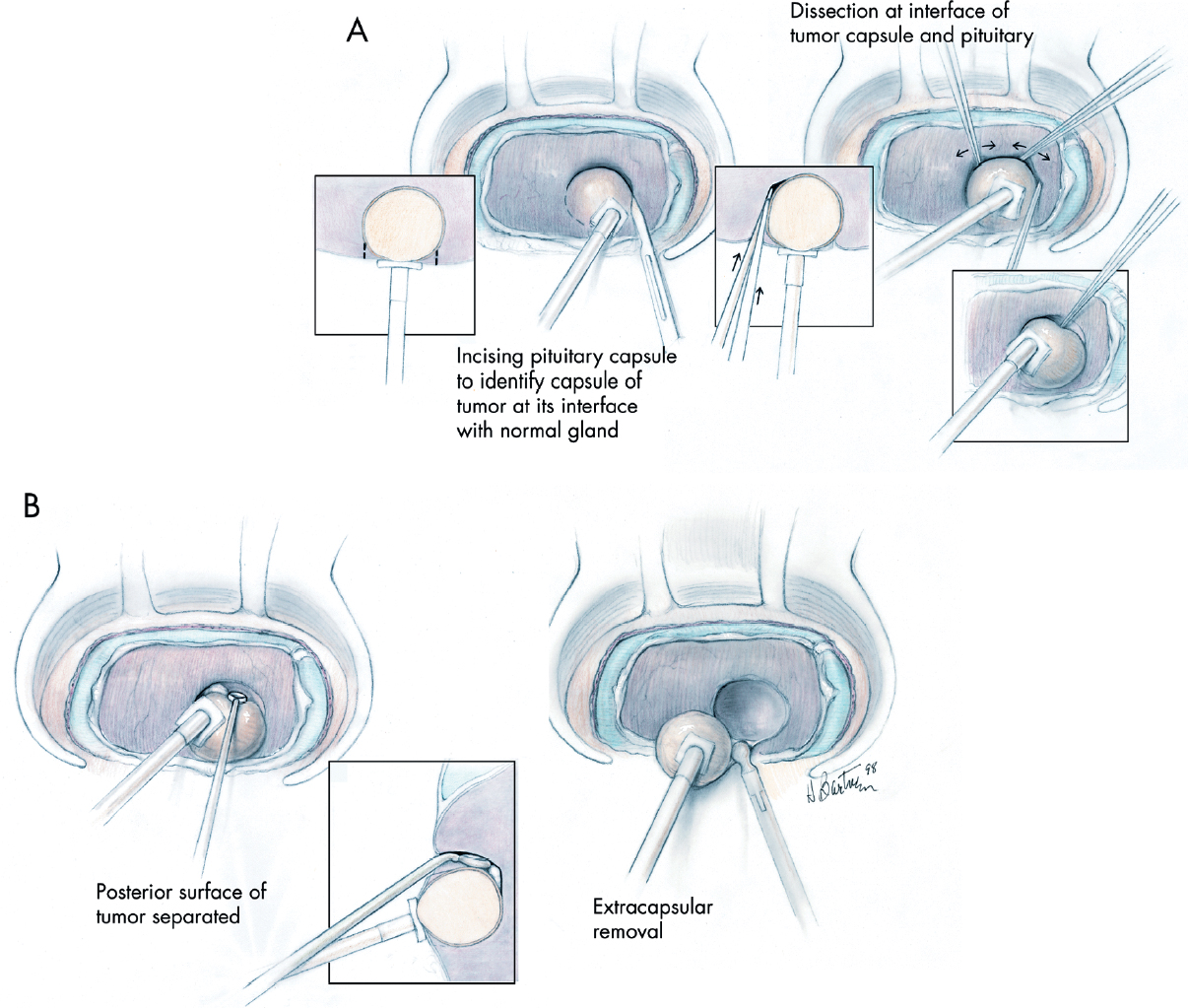
Fig. 11.2 Illustration of the surgical technique. A curvilinear incision is made through the pituitary capsule just beyond the point at which the most superficial dome of the tumor reaches the surface of the gland (A, left). This permits a thin layer of normal gland to be passed through before reaching the surgical capsule of the adenoma (left inset), allowing easy identification of the surgical capsule and the creation of a surgical plane of dissection at the margin of the tumor, at the interface of the normal gland and the surgical capsule of the adenoma. This interface is further defined using the tips of the bipolar forceps in a series of movements parallel to the surface of the adenoma and in the crevice between the gland and the adenoma (B, right and center). Gentle dissection of the interface between the adenoma and gland is continued following the curvilinear margin of the adenoma. After the most superficial portion of the tumor has been defined circumferentially, the deeper adenoma margins are defined and dissected in a similar fashion (B); the posterior margin of the adenoma often requires dissection using a disk dissector and a small or medium ring curette (B, center). After the margins of the tumor have been completely dissected, to prevent rupture of the tumor the last remaining connection between the pseudocapsule of the specimen and the pituitary capsule is grasped with a small cup forceps and the tumor is removed (B, right). In cases of tumors 8 to 10 mm or less in diameter, the entire tumor can usually be shelled out of its bed in the anterior lobe as an intact specimen. Successful and complete removal leaves a smoothly lined hemispherical tissue void in the anterior lobe. (From Oldfield EH, Vortmeyer AO. Development of a histological pseudocapsule and its use as a surgical capsule in the excision of pituitary tumors. J Neurosurg 2006;104:7–19. Reprinted with permission.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


