Purpose
To investigate the relationship between the integrity of the photoreceptor microstructures and retinal sensitivity after half-dose photodynamic therapy (PDT) in eyes with chronic central serous chorioretinopathy (CSC).
Design
Prospective, noncomparative, interventional case series.
Methods
Thirteen eyes of 13 patients with chronic CSC who had received half-dose verteporfin PDT were studied. The best-corrected visual acuity (BCVA), macular retinal sensitivity in the central 12 degrees, and optical coherence tomographic (OCT) findings were evaluated at baseline and at 1, 3, 6, and 12 months after the half-dose PDT. The integrities of the external limiting membrane (ELM), the inner segment/outer segment junction (IS/OS) line, and the cone outer segment tips (COST) line were determined. The retinal sensitivity was determined by MP-1 microperimetry.
Results
The serous retinal detachment (SRD) was completely resolved in 11 eyes at 1 month and in 1 eye at 3 months. The remaining eye had a persistent SRD throughout the follow-up period. The mean retinal sensitivity was significantly better at 1, 3, 6, and 12 months after the half-dose PDT than at baseline. Before the PDT, 12 eyes had a continuous ELM and 1 eye had a fragmented ELM. The number of eyes with an intact IS/OS line and COST line increased with increasing post-PDT time. At 12 months after PDT, the IS/OS line was detected in 11 eyes and the COST line in 6 eyes. At 6 and 12 months, the retinal sensitivity was significantly higher in eyes with an intact COST line and IS/OS lines than in eyes with an intact IS/OS line only. However, no difference was found in the visual acuity of these 2 groups. The 1 eye with a persistent SRD and another eye with fragmented ELM and absent IS/OS and COST lines through the follow-up periods were associated with poor retinal sensitivity of 8.5 dB and 10.9 dB respectively.
Conclusions
Our findings show that there is a significant improvement in the macular sensitivity after half-dose PDT in eyes with chronic CSC. The improvement was correlated with the recovery of the IS/OS and COST lines at 6 and 12 months.
Eyes with central serous chorioretinopathy (CSC) are characterized by serous retinal detachments (SRDs) in the macula. The SRDs are caused by a leakage of fluid from the choroid into the subretinal space through a breakdown of the barrier in the retinal pigment epithelium (RPE). CSC often resolves spontaneously in several months without treatment; however, some patients show a persistent SRD and functional disturbances. Chronic CSC may be associated with RPE atrophy and retinal degeneration, including cystoid macular degeneration, resulting in poor visual function.
Photodynamic therapy (PDT) with verteporfin has been used to treat persistent SRDs, and the results have been good. PDT appears to reduce choroidal exudation by temporary choriocapillaris occlusion, which then decreases the amount of fluid leaking into the subretinal space. Previous studies suggest that photodynamic therapy may increase the risk of secondary choroidal neovascularization and RPE atrophy.
Recently, several studies examined the effects of a modification of the standard PDT procedures (eg, half-dose verteporfin with PDT) to treat SRDs and demonstrated good results without complications.
A relative central scotoma is one of the chief complaints of CSC patients. Microperimetry is a valuable supplemental test that can enable objective assessment of the residual complaints in patients who have regained normal best-corrected visual acuity (BCVA). There have been 3 studies that reported an improvement in macular sensitivity after PDT in eyes with chronic CSC. In general, it was not uncommon to find low retinal sensitivity in spite of a complete resolution of the SRD.
Spectral-domain optical coherence tomography (SD-OCT) has enabled investigators to examine the morphology of the microstructures of the photoreceptors of the retina. A recent study using SD-OCT demonstrated its ability to resolve the cone outer segment tips (COST) line, which is formed by the microvilli of the retinal pigment epithelial cells. A significant association between the BCVA and the integrity of the photoreceptor inner and outer segment junction (IS/OS) line and the COST line has been reported for some retinal diseases. However, no information is available on the relationship between retinal sensitivity and OCT findings of the microstructures of the photoreceptors after PDT for CSC.
Thus, the purpose of this study was to determine whether the integrities of the IS/OS and COST lines were significantly correlated with the BCVA and retinal sensitivity 1 year after half-dose PDT in eyes with CSC.
Patients and Methods
Patients who were diagnosed as chronic CSC in Surugadai Nihon University Hospital between September 2008 and June 2009 were enrolled in the study. The inclusion criteria were: 1) presence of SRD involving the fovea detected by OCT; 2) visual symptoms for more than 6 months with diffuse pigment epithelial decompensation or focal leakage on fluorescein angiography (FA); and 3) hyperpermeability including the macular area during indocyanine green angiography (IA). The exclusion criteria were: evidence of choroidal neovascularization on either FA or IA; and other ocular and macular diseases, such as age-related macular degeneration, idiopathic polypoidal vasculopathy, pathologic myopia, inflammatory diseases, retinal vasculopathies, and hereditary dystrophies, that affect the visual acuity.
All patients had a comprehensive ophthalmic examination including refraction, visual acuity measurements, FA, IA, OCT, and microperimetry at baseline. The visual acuity measurements, OCT, and microperimetry were repeated at 1, 3, 6, and 12 months after the PDT.
Microperimetry was performed using the MP-1 (Nidek Technologies, Vigonza, Italy). The Goldmann III (Nidek Technologies) target and a 4-2 staircase strategy were used. Forty-five stimulus locations covering an area of 12 degrees in diameter were examined. The stimuli were projected on a white background with background illumination set to 1.27 cd/m 2 and a stimulus presentation time of 200 ms. The stimulus intensity varied from 0 dB to 20 dB in 1-dB steps. All patients had to demonstrate good collaboration in the microperimetry test, which means a correct understanding of the technique and a good concentration.
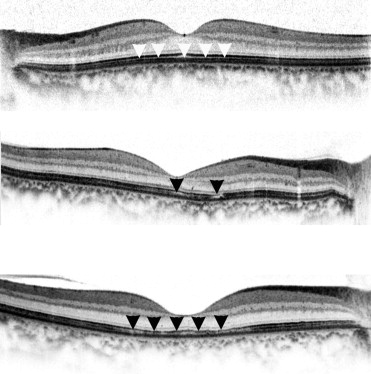
OCT images were obtained with the SD-OCT (Spectralis HRA+OCT, Heidelberg Engineering GmbH, Heidelberg, Germany). The area of the serous retinal detachment before PDT was examined in the horizontal B-scan cross-sectional images. The following morphologic changes of the macular photoreceptor microstructures were evaluated by 2 masked investigators (K.F. and Y.M.) independently: the presence or absence of SRD and the integrities of the external limiting membrane (ELM), the IS/OS line, and the COST line. The ELM, IS/OS line, and COST line were graded as continuous, fragmented, or absent ( Figure 1 ).
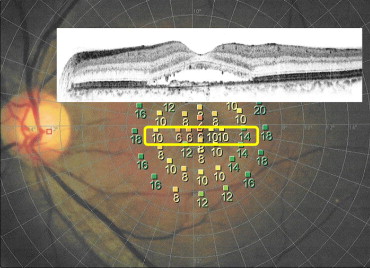
To determine the correlation between the retinal sensitivities and OCT findings, we selected the points of retinal sensitivities within the SRD determined by the OCT images of a horizontal scan ( Figure 2 ).
PDT was performed using half-dose verteporfin (Visudyne; Novartis AG, Bulach, Switzerland). Briefly, 3 mg/m 2 of verteporfin was infused over 10 minutes, and 15 minutes after beginning the infusion the laser treatment was begun. The total light energy delivered to the area of hyperpermeability detected on the IA images was 50 J/cm 2 . The spot size covered the area of dilated and congested choroidal vessels and the area with sub-RPE leakage shown in the IA images.
Paired t tests were used to determine the significance of improvements in function after the PDT. A P < .05 was considered statistically significant.
Results
Thirteen eyes of 13 patients (13 men) were studied. All 13 patients were diagnosed with chronic CSC and were treated with half-dose PDT. The clinical characteristics and changes of visual function before and after the half-dose PDT are shown in the Table . The mean age of the patients was 50.7 years, with a range of 40 to 64 years. None of the patients had a history of corticosteroid use before the PDT. The mean duration of the symptoms before the half-dose PDT was 45 months, with a range of 6 to 132 months. The initial BCVA ranged from 0.15 to 1.5 decimal units or 0.82 to −0.18 logarithm of the minimal angle of resolution (logMAR) units. The mean PDT spot size was 4469 μm, with a range of 2700 to 5900 μm. The PDT spot area included the fovea in all cases.
| Patient No. | Sex | Age (Y) | Duration of Symptom (M) | GLD | Recurrence | RD at 12M | BCVA (Decimal Units) | Retinal Sensitivity (dB) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | 1M | 3M | 6M | 12M | Baseline | 1M | 3M | 6M | 12M | |||||||
| 1 | Male | 45 | 12 | 3800 | (−) | (−) | 0.9 | 1.0 | 1.2 | 1.5 | 1.5 | 8.86 | 12.86 | 13.43 | 15.71 | 16.57 |
| 2 | Male | 64 | 120 | 5100 | (−) | (−) | 0.7 | 0.6 | 0.6 | 0.8 | 0.7 | 8 | 9.25 | 11 | 9.75 | 12.75 |
| 3 | Male | 40 | 48 | 2700 | (−) | (−) | 1.0 | 1.0 | 1.5 | 1.5 | 1.5 | 6.67 | 12.33 | 12.33 | 14.33 | 16.33 |
| 4 | Male | 54 | 132 | 5900 | (−) | (−) | 1.5 | 1.2 | 1.5 | 1.5 | 1.5 | 9.33 | 13.67 | 16.33 | 18.33 | 18.33 |
| 5 | Male | 62 | 13 | 5300 | (−) | (−) | 0.7 | 0.7 | 0.8 | 1.0 | 1.0 | 6.44 | 6 | 12.44 | 12.67 | 15.11 |
| 6 | Male | 57 | Unknown | 4500 | (+) | 0.15 | 0.1 | 0.15 | 0.2 | 0.2 | 3.14 | 6.29 | 8.57 | 6.57 | 8.57 | |
| 7 | Male | 55 | 12 | 4500 | (−) | (−) | 0.7 | 1.0 | 1.0 | 1.5 | 1.5 | 10 | 12 | 14.33 | 14.67 | 14.33 |
| 8 | Male | 45 | 72 | 4200 | (−) | (−) | 1.2 | 1.2 | 1.5 | 1.5 | 1.5 | 5 | 16.75 | 18.75 | 17.25 | 19.5 |
| 9 | Male | 41 | 6 | 4300 | (−) | (−) | 0.5 | 0.7 | 0.8 | 0.9 | 0.9 | 9.33 | 10.67 | 13.33 | 14.67 | 14.67 |
| 10 | Male | 44 | 36 | 3500 | (−) | (−) | 0.2 | 0.3 | 0.4 | 0.4 | 0.7 | 4.22 | 7.1 | 9.56 | 14.67 | 10.89 |
| 11 | Male | 50 | 6 | 4900 | (−) | (−) | 0.7 | 0.7 | 0.9 | 0.9 | 0.9 | 2.5 | 14 | 16.25 | 17.5 | 15.75 |
| 12 | Male | 46 | 33 | 4000 | (−) | (−) | 0.9 | 0.9 | 1.0 | 1.0 | 1.5 | 11.2 | 14.8 | 17.2 | 17.6 | 18.8 |
| 13 | Male | 56 | 60 | 5400 | (−) | (−) | 0.9 | 0.7 | 1.0 | 1.5 | 1.2 | 8.86 | 12 | 17.14 | 19.71 | 19.14 |
None of the 13 eyes had a decrease in the mean retinal sensitivity within the area of the serous retinal detachment. All eyes had improvements of retinal sensitivity of >2.5 dB at 12 months. The mean retinal sensitivity within the area of the SRD significantly improved from 7.2 dB at baseline to 11.4, 13.9, 14.9, and 15.4 dB at 1, 3, 6, and 12 months after half-dose PDT, respectively. The BCVA improved significantly only after 3 months ( P < .01, Figure 3 ).
The SRD resolved completely after 1 month in 11 eyes and after 3 months in 1 eye. The remaining eye (Case 6) had a persistent SRD throughout the follow-up period, even though SRD decreased gradually.
The appearance of the ELM, IS/OS, and COST lines in the horizontal OCT scans are shown in Figure 4 . Before the PDT, 12 eyes had a continuous ELM and 1 eye had a fragmented ELM. The IS/OS and COST lines were absent in all eyes. The number of eyes with fragmented and continuous IS/OS line and COST line gradually increased during the post-PDT period. At 12 months after half-dose PDT, a continuous or fragmented IS/OS line was detected in 11 of 13 eyes, and a continuous or fragmented COST line was detected in 6 eyes. At 12 months, 1 eye with a persistent SRD (Case 6) did not show an IS/OS line and COST line in the OCT images, and the retinal sensitivity was low at 8.5 dB. Another eye with a fragmented ELM and absent IS/OS and COST line (Case 10) also had poor retinal sensitivity at 10.9 dB.




