Cornea
4.1 Superficial Punctate Keratopathy
Symptoms
Pain, photophobia, red eye, foreign body sensation, mildly decreased vision.
Signs
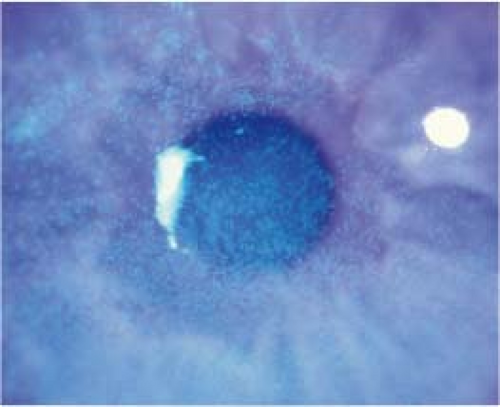
(See Figure 4.1.1.)
Critical. Pinpoint corneal epithelial defects that stain with fluorescein. May be confluent if severe. Staining pattern may allude to etiology. Pain is relieved by the instillation of anesthetic drops.
Other. Conjunctival injection, watery discharge.
Etiology
Superficial punctate keratopathy (SPK) is nonspecific but is most commonly seen in the following disorders, which may be associated with a specific staining pattern:
Superior staining
Contact lens-related disorder (e.g., chemical toxicity, tight lens syndrome, contact lens overwear syndrome, giant papillary conjunctivitis). SEE 4.20, CONTACT LENS-RELATED PROBLEMS.
Foreign body under the upper eyelid: Typically linear SPK, fine epithelial defects arranged vertically.
Floppy eyelid syndrome: Extremely loose upper eyelids that evert easily. SEE 6.6, FLOPPY EYELID SYNDROME.
Superior limbic keratoconjunctivitis (SLK): Superior bulbar conjunctival inflammation. SEE 5.4, SUPERIOR LIMBIC KERATOCONJUNCTIVITIS.
Vernal conjunctivitis: Atopy, large conjunctival papillae under the upper eyelid and/or limbus. SEE 5.1, ACUTE CONJUNCTIVITIS.
Interpalpebral staining
Dry eye syndrome: Poor tear lake, decreased tear break-up time, decreased Schirmer test. SEE 4.3, DRY EYE SYNDROME.
Neurotrophic keratopathy: Decreased corneal sensation. May progress to corneal ulceration. SEE 4.6, NEUROTROPHIC KERATOPATHY.
Ultraviolet burn/photokeratopathy: Often in welders or from sunlamps. SEE 4.7, ULTRAVIOLET KERATOPATHY.
Inferior staining
Blepharitis: Erythema, telangiectasias, or crusting of the eyelid margins, meibomian gland dysfunction. SEE 5.8, BLEPHARITIS/MEIBOMITIS.
Exposure keratopathy: Poor eyelid closure with failure of eyelids to cover the entire globe. SEE 4.5, EXPOSURE KERATOPATHY.
Topical drug toxicity (e.g., neomycin, gentamicin, trifluridine, atropine, as well as any drop with preservatives, including artificial tears, or any frequently used drop).
Conjunctivitis: Discharge, conjunctival injection, eyelids stuck together on awakening. SEE 5.1, ACUTE CONJUNCTIVITIS AND 5.2, CHRONIC CONJUNCTIVITIS.
Trichiasis/distichiasis: One or more eyelashes rubbing against the cornea (superior SPK if misdirected lashes from upper eyelid). SEE 6.5, TRICHIASIS.
Other
Trauma: SPK can occur from relatively mild trauma, such as chronic eye rubbing.
Mild chemical injury: SEE 3.1, CHEMICAL BURN.
Thygeson keratitis: Bilateral, recurrent epithelial keratitis (raised epithelial staining lesions, not SPK) without conjunctival injection. SEE 4.8, THYGESON SUPERFICIAL PUNCTATE KERATITIS.
Work-Up
History: Trauma? Contact lens wear? Eye drops? Discharge or eyelid matting? Chemical or ultraviolet light exposure? Snoring or sleep apnea? Time of day when worse?
Evaluate the cornea, eyelid margin, and tear film with fluorescein. Evert the upper and lower eyelids. Check eyelid closure, position, and laxity. Look for inward-growing or misdirected lashes.
Inspect contact lenses for fit (if still in the eye) and for the presence of deposits, sharp edges, and cracks.
Treatment
See the appropriate section to treat the underlying disorder. SPK is often treated nonspecifically as follows:
Noncontact lens wearer with a small amount of SPK
Artificial tears q.i.d., preferably preservative-free.
Can add a lubricating ointment q.h.s.
Noncontact lens wearer with a large amount of SPK
Preservative-free artificial tears q2h.
Ophthalmic antibiotic ointment (e.g., bacitracin/polymyxin B or erythromycin q.i.d. for 3 to 5 days).
Consider a cycloplegic drop (e.g., cyclopentolate 1% to 2% t.i.d.) for relief of pain and photophobia.
Contact lens wearer with a small amount of SPK
Discontinue contact lens wear.
Artificial tears four to six times per day, preferably preservative-free.
Can add a lubricating ointment q.h.s.
Contact lens wearer with a large amount of SPK
Discontinue contact lens wear.
Antibiotic: Fluoroquinolone (e.g., gatifloxacin, moxifloxacin, or besifloxacin) or aminoglycoside (e.g., tobramycin) drops four to six times per day as well as ophthalmic ointment q.h.s. (e.g., ciprofloxacin or bacitracin/polymyxin B). If confluent SPK, consider ophthalmic antibiotic ointment four to six times per day.
Consider a cycloplegic drop (e.g., cyclopentolate 1% to 2% t.i.d.) for relief of pain and photophobia.
Follow-Up
Noncontact lens wearers with SPK are not seen again solely for the SPK unless the patient is a child or is unreliable. Reliable patients are told to return if their symptoms worsen or do not improve within 2 to 3 days. When underlying ocular disease is responsible for the SPK, follow-up is in accordance with the guidelines for the underlying problem.
Contact lens wearers with a large amount of SPK are seen every day or two until significant
improvement is demonstrated. Contact lenses are not to be worn until the condition clears. Antibiotics may be discontinued when the SPK resolves. The patient’s contact lens regimen (e.g., wearing time, cleaning routine) must be corrected or the contact lenses changed if either is thought to be responsible (SEE 4.20, CONTACT LENS-RELATED PROBLEMS). Contact lens wearers with a small amount of SPK are rechecked in several days to 1 week, depending on symptoms and degree of SPK.
4.2 Recurrent Corneal Erosion
Symptoms
Recurrent attacks of acute ocular pain, photophobia, foreign body sensation, and tearing. The pain may awaken patients from sleep or occur immediately upon eye opening. There is often a history of prior corneal abrasion in the involved eye.
Signs
Critical. Localized irregularity and mobility of the corneal epithelium (fluorescein dye may outline the area with negative or positive staining) or a corneal abrasion. Epithelial changes may resolve within hours of the onset of symptoms so abnormalities may be subtle or absent when the patient is examined.
Other. Corneal epithelial dots or small cysts (microcysts), a fingerprint pattern, or map-like lines may be seen in both eyes if epithelial basement membrane (map–dot–fingerprint) dystrophy is present. These findings may also be seen unilaterally and focally in any eye that has recurrent erosions.
Etiology
Damage to the corneal epithelium or epithelial basement membrane from one of the following:
Anterior corneal dystrophy: Epithelial basement membrane (most common), Reis–Bücklers, Thiel–Behnke, and Meesmann dystrophies.
Previous traumatic corneal abrasion: Injury may have been years before the current presentation.
Stromal corneal dystrophy: Lattice, granular, and macular dystrophies.
Corneal degeneration: Band keratopathy, Salzmann nodular degeneration.
Keratorefractive, corneal transplant, cataract surgery, or any surgery in which the corneal epithelium is removed (either therapeutically or for visualization).
Work-Up
History: History of a corneal abrasion? Ocular surgery? Family history (corneal dystrophy)?
Slit lamp examination with fluorescein staining of both eyes (visualization of abnormal basement membrane lines may be enhanced by instilling fluorescein and looking for areas of rapid tear break-up, referred to as “negative staining”).
Treatment
Acute episode: Cycloplegic drop (e.g., cyclopentolate 1%) three times daily and ophthalmic antibiotic ointment (e.g., erythromycin, bacitracin) four to six times daily. Can use 5% sodium chloride ointment q.i.d. in addition to antibiotic ointment. If the epithelial defect is large, a pressure patch or bandage contact lens and topical antibiotic drops q.i.d. may be placed (NEVER patch contact lens wearers). Oral analgesics as needed.
Never prescribe topical anesthetic drops.
After epithelial healing is complete, artificial tears four to eight times per day and artificial tear ointment q.h.s. for at least 3 to 6 months, or 5% sodium chloride drops four times per day and 5% sodium chloride ointment q.h.s. for at least 3 to 6 months.
If the corneal epithelium is loose or heaped and is not healing, consider epithelial debridement. Apply a topical anesthetic (e.g., proparacaine) and use a sterile cotton-tipped applicator or cellulose sponge (e.g., Weck-Cel surgical spear) to gently remove all the loose epithelium.
For erosions not responsive to the preceding treatment, consider the following:
Prophylactic medical treatment with 5% sodium chloride ointment q.h.s.
Oral doxycycline (matrix metalloproteinase inhibitor) 50 mg b.i.d. with or without a short course of topical corticosteroid drops (e.g., fluorometholone 0.1% b.i.d. to q.i.d. for 2 to 4 weeks).
Extended-wear bandage soft contact lens for several months with a topical antibiotic and routine changing of the lens.
Anterior stromal puncture can be applied to localized erosions, such as in traumatic cases, outside the visual axis in cooperative patients. It can be performed with or without an intact epithelium. Stromal puncture may be applied manually at the slit lamp or with Nd:YAG laser. This treatment may cause small permanent corneal scars that are usually of no visual significance if outside the visual axis.
Epithelial debridement with diamond burr polishing of Bowman membrane or phototherapeutic keratectomy (PTK). Both are highly effective (up to 90%) for large areas of epithelial irregularity and lesions in the visual axis. Excimer laser ablation of the superficial stroma can be particularly helpful if repeated erosions have created anterior stromal haze or scarring.
Follow-Up
Every 1 to 2 days until the epithelium has healed, and then every 1 to 3 months, depending on the severity and frequency of the episodes. It is important to educate patients that persistent use of lubricating ointment (5% sodium chloride or tear ointment) for 3 to 6 months following the initial healing process reduces the chance of recurrence.
4.3 Dry Eye Syndrome
Symptoms
Burning, dryness, foreign body sensation, mildly to moderately decreased vision, excess tearing. Often exacerbated by smoke, wind, heat, low humidity, or prolonged use of the eye (e.g., when working on a computer that results in decreased blink rate). Usually bilateral and chronic (although patients sometimes are seen with recent onset in one eye). Discomfort often out of proportion to clinical signs.
Signs
Critical
Scanty or irregular tear meniscus seen at the inferior eyelid margin: The normal meniscus should be at least 0.5 mm in height and have a convex shape.
Decreased tear break-up time (measured from a blink to the appearance of a tear film defect, by using fluorescein stain): Less than 10 seconds indicates tear film instability.
Other. Punctate corneal or conjunctival fluorescein, rose bengal, or lissamine green staining; usually inferiorly or in the interpalpebral area. Excess mucus or debris in the tear film and filaments on the cornea may be found in severe cases.
Etiology
Idiopathic: Commonly found in menopausal and postmenopausal women.
Evaporative: Lipid layer tear deficiency; often associated with blepharitis or meibomian gland dysfunction. Symptoms may be worse in the morning with complaints of visual blurring upon waking.
Aqueous deficient: Aqueous layer tear deficiency; aqueous production decreases with age. Symptoms frequently worse later in the day or after extensive use of the eyes.
Combination: Evaporative and aqueous deficiency often occurs together. May also include a mucin layer tear deficiency.
Lifestyle related: Arid climate, allergen exposure, smoking, extended periods of reading/computer work/television viewing.
Connective tissue diseases (e.g., Sjögren syndrome, rheumatoid arthritis, granulomatosis with polyangiitis [Wegener granulomatosis], systemic lupus erythematosus).
Conjunctival scarring (e.g., ocular cicatricial pemphigoid, Stevens–Johnson syndrome, trachoma, chemical burn).
Drugs (e.g., oral contraceptives, anticholinergics, antihistamines, antiarrhythmics, antipsychotics, antispasmodics, tricyclic antidepressants, beta blockers, diuretics, retinoids, selective serotonin reuptake inhibitors, chemotherapy).
Infiltration of the lacrimal glands (e.g., sarcoidosis, tumor).
Postradiation fibrosis of the lacrimal glands.
Vitamin A deficiency: Usually from malnutrition, intestinal malabsorption, or bariatric surgery. SEE 13.7, VITAMIN A DEFICIENCY.
After corneal refractive surgery such as photorefractive keratectomy (PRK) and laser in situ keratomileusis (LASIK): Likely secondary to disruption of corneal nerves and interference with normal reflex tearing.
Work-Up
History and external examination to detect underlying etiology.
Slit lamp examination with fluorescein stain to examine the ocular surface and tear break-up time. May also use rose bengal or lissamine green stain to examine the cornea and conjunctiva. Tear meniscus is best examined prior to the instillation of eye drops.
Schirmer test. Technique: After drying the eye of excess tears, Schirmer filter paper is placed at the junction of the middle and lateral one-third of the lower eyelid in each eye for 5 minutes. Eyes are to remain open with normal blinking.
Unanesthetized: Measures basal and reflex tearing. Normal is wetting of at least 15 mm in 5 minutes.
Anesthetized: Topical anesthetic (e.g., proparacaine) is applied before drying the eye and placing the filter paper. Measures basal tearing only. Abnormal is wetting of 5 mm or less in 5 minutes. Less than 10 mm may be considered borderline. We prefer the less irritating anesthetized method.
Other potentially helpful in-office tests include measurement of tear osmolarity and level of matrix metalloproteinase-9 (MMP-9); elevation of these factors suggests dryness and inadequate tear film. Tear lactoferrin can also be measured; low levels suggest aqueous deficient dry eye disease.
Consider screening for Sjögren syndrome.
Treatment
Mild Dry Eye
Artificial tears q.i.d.
Moderate Dry Eye
Increase the frequency of artificial tear application up to q1–2h; use unit dose preservative-free artificial tears.
Add a lubricating ointment or gel q.h.s.
Lifestyle modification (e.g., humidifiers and smoking cessation).
Cyclosporine 0.05% b.i.d. is effective for patients with chronic dry eye and decreased tears secondary to ocular inflammation. Cyclosporine often burns with application for the first several weeks and takes 1 to 3 months for significant clinical improvement. To hasten improvement and lessen side effects, consider treating patients concomitantly with a mild topical corticosteroid drop (e.g., loteprednol 0.5%) b.i.d. to q.i.d. for 1 month while beginning cyclosporine therapy.
If these measures are inadequate or impractical, consider punctal occlusion. Use collagen inserts (temporary) or silicone or acrylic plugs (reversible). Be sure any inflammatory component including blepharitis is treated prior to punctal occlusion.
Severe Dry Eye
Cyclosporine 0.05%, as described earlier.
Punctal occlusion, as described earlier (both lower and upper puncta if necessary), and preservative-free artificial tears up to q1–2h. Consider permanent occlusion by thermal cautery if plugs fall out.
Add lubricating ointment or gel b.i.d. to q.i.d. p.r.n.
Moisture chamber (plastic film sealed at orbital rim) or goggles with lubrication at night.
If mucus strands or filaments are present, remove with forceps and consider 10% acetylcysteine q.i.d.
Other therapies may include oral flaxseed oil, oral omega-3 fatty acids, autologous serum tears, topical vitamin A, bandage contact lens, or a scleral lens.
Consider a permanent lateral tarsorrhaphy if all of the previous measures fail. A temporary adhesive tape tarsorrhaphy (to tape the lateral one-third of the eyelid closed) can also be used, pending a surgical tarsorrhaphy.
In addition to treating the dry eye, treatment for contributing disorders (e.g., blepharitis, exposure keratopathy) should be instituted if these conditions are present.
Always use preservative-free artificial tears if dosing is more frequent than q.i.d. to prevent preservative toxicity.
If the history suggests the presence of a connective tissue disease (e.g., history of arthritic pain, dry mouth), consider blood testing for these conditions and/or referral to an internist or rheumatologist for further evaluation.
Follow-Up
In days to months, depending on the severity of symptoms and degree of dryness. Anyone with severe dry eyes caused by an underlying chronic systemic disease (e.g., rheumatoid arthritis, Sjögren syndrome, sarcoidosis, ocular pemphigoid) may need to be monitored more closely.
Patients with Sjögren syndrome have an increased incidence of lymphoma and mucous membrane problems and may require internal medicine, rheumatologic, dental, and gynecologic follow-up.
4.4 Filamentary Keratopathy
Symptoms
Moderate-to-severe pain, red eye, foreign body sensation, tearing, photophobia.
Signs
Critical. Short fluorescein-staining strands of degenerated epithelial cells surrounding a mucus core adherent to anterior surface of cornea.
Other. Conjunctival injection, poor tear film, punctate epithelial defects.
Etiology
Severe ocular dryness: Most common cause. SEE 4.3, DRY EYE SYNDROME.
SLK: Filaments are located in the superior cornea, in association with superior conjunctival injection, superior punctate fluorescein staining, and superior corneal pannus. SEE 5.4, SUPERIOR LIMBIC KERATOCONJUNCTIVITIS.
Recurrent corneal erosions: Recurrent spontaneous corneal abrasions often occurring upon waking. SEE 4.2, RECURRENT CORNEAL EROSION.
Adjacent to irregular corneal surface (e.g., postoperative, near a surgical wound).
Patching (e.g., postoperative, after corneal abrasions) or ptosis.
Neurotrophic keratopathy: SEE 4.6, NEUROTROPHIC KERATOPATHY.
Work-Up
History, especially for the previously mentioned conditions.
Slit lamp examination with fluorescein staining.
Treatment
Treat the underlying condition.
Consider debridement of the filaments. After applying topical anesthetic (e.g., proparacaine), gently remove filaments at their base with fine forceps or a cotton-tipped applicator. This gives temporary relief, but the filaments will recur if the underlying etiology is not treated.
Lubrication with one of the following regimens:
Preservative-free artificial tears six to eight times per day and lubricating ointment q.h.s.
Punctal occlusion.
Acetylcysteine 10% q.i.d.
 NOTE: Acetylcysteine is not commercially available as a drop but can be made by a compounding pharmacy.
NOTE: Acetylcysteine is not commercially available as a drop but can be made by a compounding pharmacy.
If the symptoms are severe or treatment fails, then consider a bandage soft contact lens (unless the patient has severe dry eyes as underlying etiology). Extended-wear bandage soft contact lenses may need to be worn for weeks to months. Concomitant prophylactic or therapeutic topical antibiotics such as a fluoroquinolone drops are typically given, especially if associated with a corneal abrasion/epithelial defect.
Follow-Up
In 1 to 4 weeks. If the condition is not improved, consider repeating the filament removal or applying a bandage soft contact lens. Long-term lubrication must be maintained if the underlying condition cannot be eliminated.
4.5 Exposure Keratopathy
Symptoms
Ocular irritation, burning, foreign body sensation, tearing, and redness of one or both eyes. Usually worse in the morning.
Signs
Critical. Inadequate blinking or closure of the eyelids, leading to corneal drying. Punctate epithelial defects are found in the lower one-third of the cornea or as a horizontal band in the region of the palpebral fissure (see Figure 4.5.1).
Other. Conjunctival injection and chemosis, corneal erosion, infiltrate or ulcer, eyelid deformity, or abnormal eyelid closure.
Etiology
Seventh nerve palsy: Orbicularis oculi weakness (e.g., Bell palsy). SEE 10.9, ISOLATED SEVENTH NERVE PALSY.
Sedation or altered mental status.
Eyelid deformity (e.g., ectropion or eyelid scarring from trauma, eyelid surgery such as excisional procedure, chemical burn, or herpes zoster ophthalmicus).
Nocturnal lagophthalmos: Failure to close the eyes during sleep.
Proptosis (e.g., due to an orbital process such as thyroid eye disease). SEE 7.1, ORBITAL DISEASE.
After ptosis repair or blepharoplasty procedures.
Floppy eyelid syndrome: SEE 6.6, FLOPPY EYELID SYNDROME.
Poor blink (e.g., Parkinson disease, neurotrophic cornea).
Work-Up
History: Previous Bell palsy or eyelid surgery? Thyroid disease?
Evaluate eyelid closure and corneal exposure. Ask the patient to close his or her eyes gently (as if sleeping). Assess Bell phenomenon (the patient is asked to close the eyelids forcefully against resistance; abnormal when the eyes do not rotate upward). Check for eyelid laxity.
Check corneal sensation before instillation of anesthetic drops. If sensation is decreased, there is greater risk for corneal complications.
Slit lamp examination: Evaluate the tear film and corneal integrity with fluorescein dye. Look for signs of secondary infection (e.g., corneal infiltrate, anterior chamber reaction, severe conjunctival injection).
Investigate any underlying disorder (e.g., etiology of seventh nerve palsy).
Treatment
Prevention is critical. All patients who are sedated or obtunded are at risk for exposure keratopathy and should receive lubrication according to the following recommendations.
In the presence of secondary corneal infection, SEE 4.11, BACTERIAL KERATITIS.
Correct any underlying disorder.
Preservative-free artificial tears q2–6h. Punctal occlusion with plugs may also be considered.
Lubricating ointment q.h.s. to q.i.d.
Consider eyelid taping or patching q.h.s. to maintain the eyelids in the closed position. If severe, consider taping the lateral one-third of the eyelids closed (leaving the visual axis open) during the day. Taping is rarely definitive but may be tried when the underlying disorder is thought to be temporary.
A potential in-office procedure includes placement of a sutureless amniotic membrane tissue (e.g., sterilized, dehydrated amniotic membrane covered by a bandage soft contact lens or frozen, specialized plastic ring-mounted amniotic membrane such as Prokera).
When maximal medical therapy fails to prevent progressive corneal deterioration, one of the following surgical procedures may be beneficial:
Partial tarsorrhaphy (eyelids sewn together).
Eyelid reconstruction (e.g., for ectropion).
Eyelid gold or platinum weight implant (e.g., for seventh nerve palsy).
Orbital decompression (e.g., for proptosis).
Conjunctival flap or sutured/glued amniotic membrane graft (for severe corneal decompensation if the preceding fail).
Follow-Up
Reevaluate every 1 to 2 days in the presence of corneal ulceration. Less frequent examinations (e.g., in weeks to months) are required for less severe corneal disease.
4.6 Neurotrophic Keratopathy
Symptoms
Foggy or blurry vision, red eye, foreign body sensation, swollen eyelid.
Signs
Critical. Loss of corneal sensation, intrapalpebral epithelial defects with fluorescein staining.
Other
Early: Perilimbal injection and intrapalpebral corneal punctate epithelial defects or a frank nonhealing epithelial defect with rolled edges, stromal edema, and Descemet folds. Typically located inferior to the visual axis.
Late: Corneal ulcer usually without infectious infiltrate, although concomitant infectious keratitis may occur. The ulcer often has a gray, heaped-up epithelial border, tends to be in the lower one-half of the cornea, and is horizontally oval. Progressive thinning may occur rapidly and lead to a descemetocele (corneal stromal loss down to Descemet membrane) or perforation.
Etiology
Occurs in eyes with diminished or absent corneal sensation. Denervation causes the corneal epithelium and tear film to become abnormal and unstable. May occur with any of the following conditions:
Postinfection with varicella zoster virus (VZV) or herpes simplex virus (HSV).
Following ocular surgery, particularly after corneal incisional or laser surgery (e.g., keratoplasty, LASIK, PRK).
Tumor (especially an acoustic neuroma, where both the fifth and seventh cranial nerves may
be affected) or any neurologic insult/disease of the fifth cranial nerve (e.g., brainstem stroke, trauma, multiple sclerosis, Riley–Day syndrome).
Chronic contact lens wear.
Diabetic neuropathy.
Extensive panretinal photocoagulation: May damage the long ciliary nerves (these patients often have concurrent diabetic neuropathy).
Complication of trigeminal nerve or dental surgery.
Complication of radiation therapy to the eye or an adnexal structure.
Chronic topical medications (e.g., timolol, topical NSAIDs).
Topical anesthetic abuse.
Crack keratopathy: Often bilateral. Take careful history for crack cocaine smoking or potential exposure. Often helpful to admit patient and remove them from their environment.
Chemical injury or exposure to hydrogen sulfide or carbon disulfide (used in manufacturing).
Work-Up
History: Previous episodes of a red and painful eye? Prior herpes infection, cold sores, or shingles rash around the eye and/or forehead? Diabetes? History of irradiation, stroke, or hearing problem? Previous refractive procedure or other eye surgery? Chemical exposure? Smoking history? Topical medications?
Prior to anesthetic instillation, test corneal sensation bilaterally with a sterile cotton wisp.
Slit lamp examination with fluorescein staining of cornea and conjunctiva.
Check the skin for herpetic lesions or scars from a previous herpes zoster infection.
Look for signs of a corneal exposure problem (e.g., inability to close an eyelid, seventh nerve palsy, absent Bell phenomenon).
If suspicious of a central nervous system lesion, obtain a computed tomography (CT) or magnetic resonance imaging (MRI) of the brain.
Treatment
Eyes with neurotrophic keratopathy have impaired healing. If not treated in a timely manner, an epithelial defect in an eye with this condition may progress to stromal lysis and possibly perforation.
Mild-to-moderate punctate epithelial staining: Preservative-free artificial tears q2–4h and artificial tear ointment q.h.s. Consider punctal plugs and q.h.s. patching.
Small corneal epithelial defect: Antibiotic ointment (e.g., erythromycin or bacitracin q.i.d. to q1–2h) for 3 to 5 days or until resolved. Usually requires prolonged artificial tear treatment, as described above. Consider placement of a bandage soft contact lens with prophylactic antibiotic drops (e.g., ofloxacin or moxifloxacin t.i.d. to q.i.d.) along with frequent preservative-free artificial tears (q1–2h) as an alternative to antibiotic ointment.
Corneal ulcer: SEE 4.11, BACTERIAL KERATITIS, for the work-up and treatment of a secondarily infected ulceration. Treatment options for a neurotrophic ulceration include antibiotic ointment q2h, tarsorrhaphy (eyelids sewn together), sutureless amniotic membrane tissue, sutured/glued amniotic membrane graft, or conjunctival flap (SEE TREATMENT IN 4.5, EXPOSURE KERATOPATHY). Oral doxycycline (100 mg b.i.d.), a collagenase inhibitor, may slow stromal lysis. Systemic ascorbic acid (e.g., vitamin C 1 to 2 g daily) may promote collagen synthesis and reduce the level of ulceration. Autologous serum, albumin, or umbilical cord serum eye drops may also be beneficial.
Follow-Up
Mild-to-moderate epithelial staining: In 3 to 14 days.
Corneal epithelial defect: Every 1 to 3 days until improvement demonstrated, and then every 5 to 7 days until resolved.
Corneal ulcer: Daily until significant improvement is demonstrated. Hospitalization may be required for severe ulcers (SEE 4.11, BACTERIAL KERATITIS).
4.7 Ultraviolet Keratopathy
Symptoms
Moderate-to-severe ocular pain, foreign body sensation, red eye, tearing, photophobia, blurred vision; often a history of welding or using a sunlamp without adequate protective eyewear. Symptoms typically worsen 6 to 12 hours after the exposure. Usually bilateral.
Signs
Critical. Dense, confluent punctate epithelial defects in an interpalpebral distribution highlighted with fluorescein staining.
Other. Conjunctival injection, mild-to-moderate eyelid edema, mild-to-no corneal edema, relatively miotic pupils that react sluggishly, and mild anterior chamber reaction.
Differential Diagnosis
Toxic epithelial keratopathy from exposure to a chemical (e.g., solvents, alcohol) or drug (e.g., neomycin, gentamicin, antiviral agents).
Thermal burn/keratopathy: Often from contact with curling iron, boiling fluid, fire ember, or flame. Injury usually limited to corneal epithelium; may have marked superficial corneal opacification or eschar. Treat with possible debridement of involved area, and then as for corneal abrasion. SEE 3.2, CORNEAL ABRASION.
Exposure keratopathy: Poor eyelid closure. SEE 4.5, EXPOSURE KERATOPATHY.
Floppy eyelid syndrome: Loose upper eyelids that evert easily during sleep. SEE 6.6, FLOPPY EYELID SYNDROME.
Work-Up
History: Welding? Sunlamp use? Topical medications? Chemical exposure? Prior episodes? Use of protective eyewear?
Slit lamp examination: Use fluorescein stain. Evert the eyelids to search for a foreign body.
If chemical exposure suspected, check pH of tear lake in upper and lower conjunctival fornices. If not neutral (6.8 to 7.5), treat as chemical burn. SEE 3.1, CHEMICAL BURN.
Treatment
Cycloplegic drop (e.g., cyclopentolate 1%).
Antibiotic ointment (e.g., erythromycin or bacitracin) four to eight times per day.
Consider a pressure patch for the more affected eye for 24 hours in reliable patients.
Oral analgesics as needed.
Follow-Up
If a bandage soft contact lens was placed, the patient is seen in 1 to 2 days.
Reliable patients without a bandage contact lens are asked to assess their own symptoms after 24 hours (if a patch was placed, it is removed at this time).
If much improved, the patient continues with topical antibiotics (e.g., erythromycin or bacitracin ointment q.i.d.).
If still significantly symptomatic, reevaluate. If significant punctate staining is present, retreat with a cycloplegic, antibiotic, and possible pressure patch, as discussed previously.
Unreliable patients or those with an unclear etiology should not be patched and should not have a bandage contact lens placed. Such patients should be reexamined in 1 to 2 days.
4.8 Thygeson Superficial Punctate Keratitis
Symptoms
Mild-to-moderate foreign body sensation, photophobia, and tearing. No history of red eye. Usually bilateral with a chronic course of exacerbations and remissions.
Signs
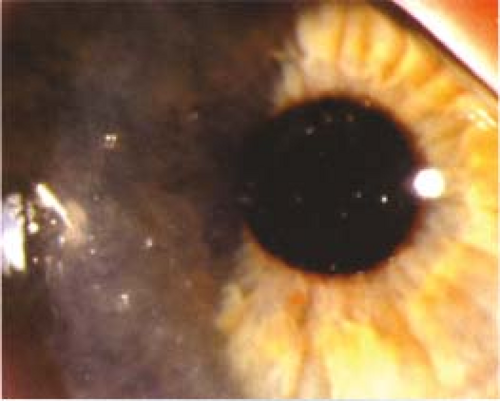
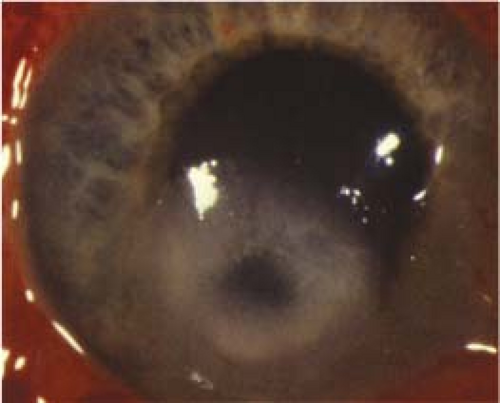
Critical. Coarse stellate gray-white corneal epithelial opacities that are often central, slightly elevated, and stain lightly with fluorescein. Underlying
subepithelial infiltrates may be present. (see Figure 4.8.1).
subepithelial infiltrates may be present. (see Figure 4.8.1).
Other. Minimal to no conjunctival injection, corneal edema, anterior chamber reaction, or eyelid abnormalities.
Treatment
Mild
Artificial tears four to eight times per day.
Artificial tear ointment q.h.s.
Moderate to Severe
Mild topical steroid (e.g., fluorometholone 0.1% or loteprednol 0.2% to 0.5% q.i.d.) for 1 to 4 weeks, followed by a very slow taper. May need prolonged low-dose topical steroid therapy.
If no improvement with topical steroids, a bandage soft contact lens can be tried.
Cyclosporine 0.05% drops daily to q.i.d. may be an alternative or adjunctive treatment, especially in patients with side effects from steroids.
Follow-Up
Weekly during an exacerbation, then every 3 to 6 months. Patients receiving topical steroids require intraocular pressure (IOP) checks every 4 to 12 weeks.
4.9 Pterygium/Pinguecula
Symptoms
Irritation, redness, decreased vision; may be asymptomatic.
Signs
Critical. One of the following, almost always centered at the 3- or 9-o’clock perilimbal position.
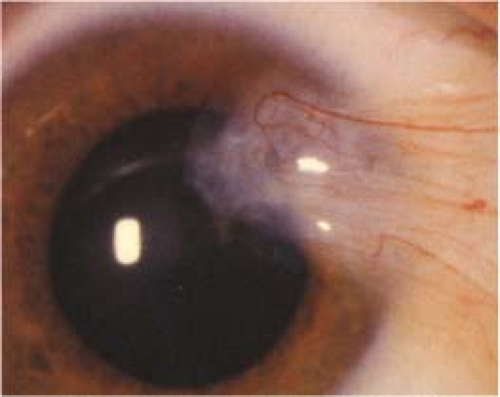
Pterygium: Wing-shaped fold of fibrovascular tissue arising from the interpalpebral conjunctiva and extending onto the cornea. There is no associated thinning of the cornea below these lesions. Usually nasal in location (see Figure 4.9.1).
Pinguecula: Yellow-white, flat or slightly raised conjunctival lesion, usually in the interpalpebral fissure adjacent to the limbus, but not involving the cornea.
Other. Either lesion may be highly vascularized and injected or may be associated with SPK or delle (thinning of the adjacent cornea secondary to drying). An iron line (Stocker line) may be seen in the cornea just beyond the leading edge of a pterygium.
Differential Diagnosis
Conjunctival intraepithelial neoplasia (CIN): Unilateral papillomatous jelly-like, velvety, or leukoplakic (white) mass, often elevated and vascularized. May not be in a wing-shaped configuration and not necessarily in the typical 3- or 9-o’clock location of a pterygium or pinguecula. SEE 5.12, CONJUNCTIVAL TUMORS.
 NOTE: Atypical pterygia require biopsy to rule out CIN or melanoma.
NOTE: Atypical pterygia require biopsy to rule out CIN or melanoma.
Limbal dermoid: Congenital rounded white lesion, usually at the inferotemporal limbus. SEE 5.12, CONJUNCTIVAL TUMORS.
Other conjunctival tumors (e.g., papilloma, nevus, melanoma). SEE 5.12, CONJUNCTIVAL TUMORS.
Pseudopterygium: Conjunctival tissue adherent to the peripheral cornea. May appear in location of previous trauma, corneal ulceration, or cicatrizing conjunctivitis. There is often associated underlying corneal thinning.
Pannus: Blood vessels growing into the cornea, often secondary to chronic contact lens wear, blepharitis, ocular rosacea, herpes keratitis, phlyctenular keratitis, atopic disease, trachoma, trauma, and others. Usually at the level of Bowman membrane with minimal to no elevation.
Sclerokeratitis: SEE 5.7, SCLERITIS.
Etiology
Elastotic degeneration of deep conjunctival layers resulting in fibrovascular tissue proliferation. Related to sunlight exposure and chronic irritation. More common in individuals from equatorial regions.
Work-Up
Slit lamp examination to identify the lesion and evaluate the adjacent corneal integrity and thickness. Check for corneal astigmatism in the axis of the pterygium.
Treatment
Protect eyes from sun, dust, and wind (e.g., ultraviolet-blocking sunglasses or goggles if appropriate).
Lubrication with artificial tears four to eight times per day to reduce ocular irritation.
For an inflamed pterygium or pinguecula:
Mild: Artificial tears q.i.d.
Moderate to severe: A mild topical steroid (e.g., fluorometholone 0.1% q.i.d., or loteprednol 0.2% to 0.5% q.i.d.), a nonsteroidal anti-inflammatory drop (e.g., ketorolac 0.4% to 0.5%), or a topical antihistamine ± mast cell stabilizer (e.g., bepotastine, ketotifen, olopatadine) may be used to decrease symptoms.
If a delle is present, then apply artificial tear ointment q2h. SEE 4.23, DELLE.
Surgical removal is indicated when:
The pterygium threatens the visual axis or induces significant astigmatism.
The patient is experiencing excessive irritation not relieved by the aforementioned treatment.
The lesion is interfering with contact lens wear.
Consider removal prior to cataract or refractive surgery.
Follow-Up
Asymptomatic patients may be checked every 1 to 2 years.
Pterygia should be measured periodically (every 3 to 12 months, initially) to determine the rate at which they are growing toward the visual axis.
If treating with a topical steroid, check after a few weeks to monitor inflammation and IOP. Taper and discontinue the steroid drop over several weeks once the inflammation has abated. A nonsteroidal drop may be used periodically for a limited duration if recurrent inflammation occurs. A topical antihistamine ± mast cell stabilizer can be used as needed (e.g., bepotastine, ketotifen, olopatadine).
4.10 Band Keratopathy
Symptoms
Decreased vision, foreign body sensation, corneal whitening; may be asymptomatic.
Signs
Critical. Anterior corneal plaque of calcium at the level of Bowman membrane, typically within the interpalpebral fissure, and separated from the limbus by clear cornea. Lucid spaces are often present in the plaque, giving it a Swiss cheese appearance. The plaque usually begins at the 3- and 9-o’clock positions, adjacent to the limbus. (See Figure 4.10.1.).
Other. May have other signs of chronic eye disease.
Etiology
More Common. Chronic uveitis (e.g., JIA), interstitial keratitis (IK), corneal edema, trauma, phthisis bulbi, long-standing glaucoma, dry eye, ocular surgery (especially retinal detachment repair with silicone oil), idiopathic.
Less Common. Hypercalcemia (may result from hyperparathyroidism, renal failure, sarcoidosis, multiple myeloma, Paget disease of bone, vitamin D excess, etc.), hyperphosphatemia, gout, corneal dystrophy, myotonic dystrophy, long-term exposure to irritants (e.g., mercury fumes), and other causes.
Work-Up
History: Chronic eye disease? Previous ocular surgery? Chronic exposure to environmental irritants or ocular medications? Systemic disease?
Slit lamp examination.
If no signs of chronic anterior segment disease or long-standing glaucoma are present, and the band keratopathy cannot be accounted for, then consider the following work-up:
Serum calcium, albumin, magnesium, and phosphate levels. Blood urea nitrogen and creatinine. Uric acid level if gout is suspected.
Treatment
Mild (e.g., Foreign Body Sensation)
Artificial tears four to six times per day and artificial tear ointment q.h.s. to q.i.d. as needed. Consider a bandage contact lens for comfort.
Severe (e.g., Obstruction of Vision, Irritation not Relieved by Lubricants, Cosmetic Problem)
Removal of the calcium may be performed at the slit lamp or under the operating microscope by chelation using disodium ethylenediamine tetraacetic acid (EDTA):
Disodium EDTA 3% to 4% is obtained from a compounding pharmacy.
Anesthetize the eye with a topical anesthetic (e.g., proparacaine) and place an eyelid speculum.
Debride the corneal epithelium overlying the calcium with a sterile scalpel or a sterile cotton-tipped applicator.
Wipe a cellulose sponge or cotton swab saturated with the EDTA solution over the band keratopathy until the calcium clears (which may take 10 to 60 minutes).
Irrigate with normal saline, place an antibiotic ointment (e.g., erythromycin), a cycloplegic drop (e.g., cyclopentolate 1% to 2%), and a pressure patch on the eye for 24 hours. Alternatively, a bandage soft contact lens or an amniotic membrane may be used to cover the epithelial defect with a topical antibiotic (e.g. moxifloxacin, gatifloxacin q.i.d.).
Consider giving the patient a systemic analgesic (e.g., acetaminophen with codeine).
Follow-Up
If surgical removal has been performed, the patient should be examined every few days until the epithelial defect has healed.
Residual anterior stromal scarring may be amenable to excimer laser PTK to improve vision. PTK may also be used to try to improve the ocular surface and prevent recurrent erosions.
The patient should be checked every 3 to 12 months, depending on the severity of symptoms. EDTA chelation can be repeated if the band keratopathy recurs.
Symptoms
Red eye, moderate-to-severe ocular pain, photophobia, decreased vision, discharge, acute contact lens intolerance.
Signs
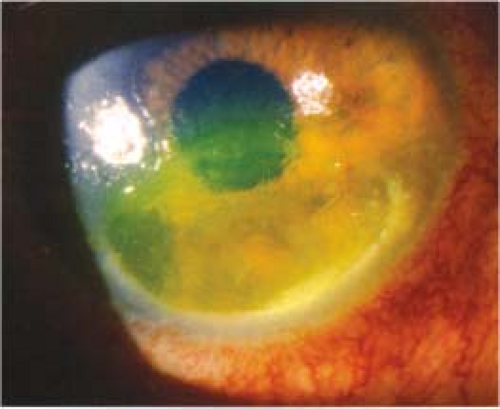
(See Figure 4.11.1.)
Critical. Focal white opacity (infiltrate) in the corneal stroma associated with an epithelial defect and underlying stromal thinning/tissue loss.
Other. Epithelial defect, mucopurulent discharge, stromal edema, folds in Descemet membrane, anterior chamber reaction, endothelial fibrin/cell deposition with or without hypopyon formation (which, in the absence of globe perforation, usually represents sterile inflammation), conjunctival injection, upper eyelid edema. Posterior synechiae, hyphema, and increased IOP may occur in severe cases.
Differential Diagnosis
Fungal: Must be considered after any traumatic corneal injury, particularly from vegetable matter (e.g., a tree branch), which may lead to filamentous fungal keratitis. Contact lens wear is another risk factor. Infiltrates commonly have feathery borders and may be surrounded by satellite lesions. Candida infections generally occur in eyes with pre-existing ocular surface disease and may mimic the clinical picture of bacterial ulcers. SEE 4.12, FUNGAL KERATITIS.
Acanthamoeba: This protozoan classically causes an extremely painful keratitis and/or stromal infiltrate; is associated with perineural invasion. It usually occurs in daily-wear soft contact lens wearers who may or may not practice poor lens hygiene. History of trauma or history of swimming and/or hot tubbing while wearing contact lenses may be elicited. In the early stages, the epithelial abnormality may look more like HSV keratitis than a bacterial ulcer. In the late stages (3 to 8 weeks), the infiltrate often becomes ring shaped. SEE 4.13, ACANTHAMOEBA KERATITIS.
HSV: May have eyelid vesicles or corneal epithelial dendrites. A history of recurrent unilateral eye disease or known ocular herpes is common. If a staining infiltrate develops in a patient with stromal herpetic keratitis, one needs to rule out bacterial superinfection. SEE 4.15, HERPES SIMPLEX VIRUS.
Atypical mycobacteria: Usually follows ocular injuries with vegetable matter or ocular surgery, such as cataract extraction, corneal grafts, and refractive surgery (especially LASIK). It has a more indolent course. Culture plates (on Lowenstein–Jensen media) must be kept for 8 weeks. An acid-fast bacillus smear is very helpful.
Sterile corneal thinning and ulcers: Minimal or no discharge, mild iritis, peripheral stromal infiltration with overlying staining and adjacent vascularization, and negative cultures. Corneal melting may be associated with various systemic diseases. SEE 4.22, PERIPHERAL CORNEAL THINNING/ULCERATION.
Staphylococcal hypersensitivity: Peripheral corneal infiltrates, sometimes with an overlying epithelial defect; usually multiple, often bilateral, with a clear space between the infiltrate and the limbus. Conjunctival injection is localized rather than diffuse, and there is less pain. There is minimal-to-no anterior chamber reaction. Often with coexisting blepharitis/meibomitis. SEE 4.18, STAPHYLOCOCCAL HYPERSENSITIVITY.
Sterile corneal infiltrates: Typically from an immune reaction to contact lens solutions or hypoxia related to contact lens wear. Usually multiple small, often peripheral, subepithelial infiltrates with little overlying staining and minimal anterior chamber reaction. Usually a diagnosis of exclusion after ruling out an infectious process. Similar lesions can occur after adenoviral conjunctivitis, but these tend to be more central and less dense with a preceding history of conjunctivitis. SEE 5.1, ACUTE CONJUNCTIVITIS.
Residual corneal foreign body or rust ring: History of foreign body injury. May be accompanied by corneal stromal inflammation, edema, and sometimes, a sterile infiltrate. There may be a mild anterior chamber reaction. The infiltrate and inflammation usually clear after the foreign body and rust ring are removed, but a superinfection may occur.
Topical anesthetic abuse: A type of neurotrophic ulcer that should be suspected when there is poor response to appropriate therapy. In the late stages of anesthetic abuse, the corneal appearance may mimic an infectious process such as Acanthamoeba or herpes simplex stromal keratitis. A large ring opacity, edema, and anterior chamber reaction are characteristic. Crack cocaine keratopathy has a similar appearance. Healing, with or without scarring, typically occurs after the exposure to anesthetic is stopped.
Etiology
Bacterial organisms are the most common cause of infectious keratitis. In general, corneal infections are assumed to be bacterial until proven otherwise by laboratory studies or until a therapeutic trial of topical antibiotics is unsuccessful. At Wills Eye, the most common causes of bacterial keratitis are Staphylococcus, Pseudomonas, Streptococcus, Moraxella, and Serratia species. Clinical findings vary widely depending on the severity of disease and on the organism involved. The following clinical characteristics may be helpful in predicting the organism involved. However, clinical impression should never take the place of broad-spectrum initial treatment and appropriate laboratory evaluation. SEE APPENDIX 8, CORNEAL CULTURE PROCEDURE.
Staphylococcal ulcers typically have a well-defined, gray-white stromal infiltrate that may enlarge to form a dense stromal abscess.
Streptococcal infiltrates may be either very purulent or crystalline (SEE 4.14, CRYSTALLINE KERATOPATHY). Acute fulminant onset with severe anterior chamber reaction and hypopyon formation are common in the former, while the latter tends to have a more indolent course and occurs in patients often on chronic topical steroids (e.g., corneal transplant patients).
Pseudomonas typically presents as a rapidly progressive, suppurative, necrotic infiltrate associated with a hypopyon and mucopurulent discharge in the setting of soft contact lens wear (see Figure 4.11.2).
Moraxella may cause infectious keratitis in patients with pre-existing ocular surface disease and in patients who are immunocompromised. Infiltrates are typically indolent, located in the inferior portion of the cornea, have a tendency to be full-thickness, and may rarely perforate.
Work-Up
History: Contact lens wear and care regimen should always be discussed. Sleeping in contact lenses? Daily or extended-wear lenses? Conventional, frequent replacement, or single use? Disinfecting solutions used? Recent changes in routine? Water exposure (swimming or hot tub use) with lenses? Trauma or corneal foreign body? Corneal surgery? History of refractive surgery? Eye care before visit (e.g., antibiotics or topical steroids)? Previous corneal disease? Systemic illness?
Slit lamp examination: Stain with fluorescein to determine if there is epithelial loss overlying the infiltrate; document the size, depth, and location of the corneal infiltrate and epithelial defect. Assess the anterior chamber reaction and look for a hypopyon. Measure the IOP, preferably with a Tono-Pen.
Corneal scrapings for smears and cultures if appropriate and if culture media are available. We routinely culture infiltrates if they are larger than 1 to 2 mm, in the visual axis, unresponsive to initial treatment, or if there is suspicion for an unusual organism based on history or examination. SEE APPENDIX 8, CORNEAL CULTURE PROCEDURE.
In contact lens wearers suspected of having an infectious ulcer, the contact lenses and case are cultured, if available. Explain to the patient that the cultured contact lenses will be discarded. A positive culture from a contact lens or contact lens case should be interpreted with clinical judgment. While a contaminant can be misleading, a result that supports the examination findings can be helpful.
Treatment
Ulcers and infiltrates are initially treated as bacterial unless there is a high index of suspicion of another form of infection. Initial therapy should be broad spectrum. Remember that bacterial coinfection may occasionally complicate fungal and Acanthamoeba keratitis. Mixed bacterial infections can also occur.
Cycloplegic drops for comfort and to prevent synechiae formation (e.g., cyclopentolate 1% t.i.d.; atropine 1% b.i.d. to t.i.d. recommended if a hypopyon in present). The specific medication depends on severity of anterior chamber inflammation.
Topical antibiotics according to the following algorithm:
Low Risk of Visual Loss
Small, nonstaining peripheral infiltrate with at most minimal anterior chamber reaction and no discharge:
Noncontact lens wearer: Broad-spectrum topical antibiotics (e.g., fluoroquinolone [moxifloxacin, gatifloxacin, besifloxacin, levofloxacin] or polymyxin B/trimethoprim drops q1–2h while awake).
Contact lens wearer: Fluoroquinolone (e.g., moxifloxacin, gatifloxacin, ciprofloxacin, besifloxacin, levofloxacin) ± polymyxin B/trimethoprim drops q1–2h while awake; can add tobramycin or ciprofloxacin ointment one to four times a day.
Borderline Risk of Visual Loss
Medium size (1 to 1.5 mm diameter) peripheral infiltrate, or any smaller infiltrate with an associated epithelial defect, mild anterior chamber reaction, or moderate discharge:
Fluoroquinolone (e.g., moxifloxacin, gatifloxacin, ciprofloxacin, besifloxacin, levofloxacin) ± polymyxin B/trimethoprim q1h around the clock. Consider starting with a loading dose of q5min for five doses and then q30min until midnight then q1h.
Vision Threatening
Our current practice at Wills Eye is to start fortified antibiotics for most ulcers larger than 1.5 to 2 mm, in the visual axis, or unresponsive to initial treatment. SEE APPENDIX 9, FORTIFIED TOPICAL ANTIBIOTICS/ANTIFUNGALS, for directions on making fortified antibiotics. If fortified antibiotics are not immediately available, start with a fluoroquinolone and polymyxin B/trimethoprim until fortified antibiotics can be obtained from a formulating pharmacy.
Fortified tobramycin or gentamicin (15 mg/mL) q1h, alternating with fortified cefazolin (50 mg/mL) or vancomycin (25 mg/mL) q1h. This means that the patient will be placing a
drop in the eye every one-half hour around the clock. Vancomycin drops should be reserved for resistant organisms, patients at risk for resistant organisms (e.g., due to hospital or antibiotic exposure, unresponsive to initial treatment), and for patients who are allergic to penicillin or cephalosporins. An increasing number of methicillin-resistant Staphylococcus aureus (MRSA) infections are now community acquired. If the ulcer is severe and Pseudomonas is suspected, consider starting fortified tobramycin every 30 minutes and fortified cefazolin q1h; in addition, consider fortified ceftazidime q1h.
In some cases, topical corticosteroids are added after the bacterial organism and sensitivities are known, the infection is under control, and severe inflammation persists. Infectious keratitis may worsen significantly with topical corticosteroids, especially when caused by fungus, atypical mycobacteria, or Pseudomonas.
Eyes with corneal thinning should be protected by a shield without a pressure patch (a patch is never placed over an eye thought to have an infection). The use of a matrix metalloproteinase inhibitor (e.g., doxycycline 100 mg p.o. b.i.d.) and a collagen synthesis promoter such as systemic ascorbic acid (e.g., vitamin C 1 to 2 g daily) may help to suppress connective tissue breakdown and prevent the perforation of the cornea.
No contact lens wear.
Oral pain medication as needed.
Oral fluoroquinolones (e.g., ciprofloxacin 500 mg p.o. b.i.d.; moxifloxacin 400 mg p.o. daily) penetrate the eye well. These may have added benefit for patients with scleral extension or for those with frank or impending perforation. Ciprofloxacin is preferred for Pseudomonas and Serratia.
Systemic antibiotics are also necessary for Neisseria infections (e.g., ceftriaxone 1 g intravenously [i.v.] q12–24h if corneal involvement, or a single 1 g intramuscular [i.m.] dose if there is only conjunctival involvement) and for Haemophilus infections (e.g., oral amoxicillin/clavulanate [20 to 40 mg/kg/day in three divided doses]) because of occasional extraocular involvement such as otitis media, pneumonia, and meningitis.
 NOTE: Systemic fluoroquinolones were historically used for Neisseria gonorrhoeae, but are no longer recommended to treat gonococcal infections (especially in men who have sex with men, in areas of high endemic resistance, and in patients with a recent foreign travel history) due to increased resistance. Additionally, they are contraindicated in pregnant women and children.
NOTE: Systemic fluoroquinolones were historically used for Neisseria gonorrhoeae, but are no longer recommended to treat gonococcal infections (especially in men who have sex with men, in areas of high endemic resistance, and in patients with a recent foreign travel history) due to increased resistance. Additionally, they are contraindicated in pregnant women and children.
Admission to the hospital may be necessary if:
Infection is sight threatening and/or impending perforation.
Patient has difficulty administering the antibiotics at the prescribed frequency.
High likelihood of noncompliance with drops or daily follow-up.
Suspected topical anesthetic abuse.
Intravenous antibiotics are needed (e.g., gonococcal conjunctivitis with corneal involvement). Often employed in the presence of corneal perforation and/or scleral extension of infection.
For atypical mycobacteria, consider prolonged treatment (q1h for 1 week, then gradually tapering) with one of the following topical agents: fluoroquinolone (e.g., moxifloxacin or gatifloxacin), amikacin (15 mg/mL), clarithromycin (1% to 4%), or tobramycin (15 mg/mL). Consider oral treatment with clarithromycin 500 mg b.i.d. Previous LASIK has been implicated as a risk factor for atypical mycobacteria infections.
Follow-Up
Daily evaluation at first, including repeat measurements of the size of the infiltrate and epithelial defect. The most important criteria in evaluating treatment response are the amount of pain, the epithelial defect size (which may initially increase because of scraping for cultures and smears), the size and depth of the infiltrate, and the anterior chamber reaction. The IOP must be checked and treated if elevated (SEE 9.7, INFLAMMATORY OPEN ANGLE GLAUCOMA). Reduced pain is often the first sign of a positive response to treatment.
If improving, the antibiotic regimen is gradually tapered but is never tapered past the minimum dose to inhibit the emergence of resistance (usually t.i.d. to q.i.d. depending on the agent). Otherwise, the antibiotic regimen is adjusted according to the culture and sensitivity results.
Consider new or repeat cultures and stains (without stopping treatment) in the setting of non-responsive or worsening infiltrate/ulcer. Treat with fortified antibiotics and modify based on culture results and the clinical course. Hospitalization may be recommended. SEE APPENDIX 8, CORNEAL CULTURE PROCEDURE.
A corneal biopsy may be required if the condition is worsening and infection is still suspected despite negative cultures.
For an impending or a complete corneal perforation, a corneal transplant or patch graft is considered. Cyanoacrylate tissue glue may also work in a treated corneal ulcer that has perforated despite infection control. Due to concern about drug penetration, antibiotics are often given for 1 to 2 days prior to glue application over an active area of infection.
4.12 Fungal Keratitis
Symptoms
Pain, photophobia, redness, tearing, discharge, foreign body sensation. Often history of minor trauma particularly with vegetable matter (e.g., a tree branch), contact lens wear, chronic eye disease, and/or a history of poor response to conventional antibacterial therapy. Usually more indolent than bacterial keratitis.
Signs
Critical
Filamentous fungi: Corneal stromal gray-white opacity (infiltrate) with a feathery border. The epithelium over the infiltrate may be elevated above the remainder of the corneal surface, or there may be an epithelial defect with stromal thinning (ulcer).
Nonfilamentous fungi: A gray-white stromal infiltrate similar to a bacterial ulcer.
Other. Satellite lesions surrounding the primary infiltrate, conjunctival injection, mucopurulent discharge, anterior chamber reaction, hypopyon. The infiltrate is more likely to extend beyond the epithelial defect than in bacterial ulcers.
Etiology
Filamentous fungi (e.g., Fusarium or Aspergillus species most commonly): Usually from trauma with vegetable matter in previously healthy eyes or associated with contact lens wear.
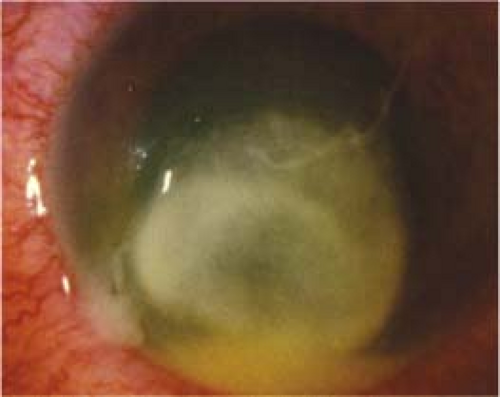
Nonfilamentous fungi (e.g., Candida species): Usually in previously diseased eyes (e.g., dry eyes, herpes simplex or zoster keratitis, exposure keratopathy, and chronic use of corticosteroid drops), see Figure 4.12.1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree