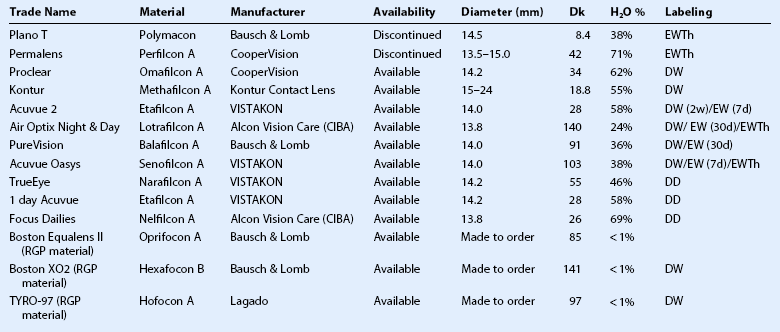
35 The first description of contact lenses in the medical literature was a report on contact lenses by Adolf Eugene Fick in 1888.1 Pearson,2 in his review of the history of contact lenses, reports Karl Otto Himmler as the first manufacturer of contact lenses. Pearson describes reports of contact lenses ranging in diameter from 15 to 22 mm in 1888, 1888, and 1889 by Fick, Kalt, and Muller, respectively, all made of glass. Examining these early glass and then polymethyl methacrylate (PMMA) large-diameter lens designs retrospectively exposes various reasons for failure, most prominently, hypoxia related to the impervious nature of glass or PMMA. This problem was circumvented in the middle of the last century through the use of small diameter PMMA corneal lenses that allowed the majority of the cornea access to atmospheric oxygen, with some transmission to the area under the mobile contact lens via the tear film. Overwear syndrome could arise, due to hypoxia under a tight or immobile lens. These lenses were used primarily for treatment of refractive error because there was invariably corneal touch and underlying hypoxia, both of which would be a challenge in the setting of ocular surface disease. Two innovations in material science allowed for contact lens to enter the therapeutic armamentarium: rigid gas-permeable polymers and soft hydrogels. The introduction of rigid gas-permeable polymers into contact lens manufacturing allowed for better physiological tolerance of corneal lenses and the reintroduction of large-diameter scleral lens designs in the early 1980s.3 Wide use of lenses made of these materials has been limited by challenges of corneal RGP lens fitting and the perception that a ‘hard’ lens cannot serve as a ‘bandage.’ Rigid gas-permeable scleral lenses that vault the cornea entirely can play a role in the treatment of ocular surface disease, as presented throughout the remainder of the chapter. The introduction of hydrophilic gels for biologic use, and in particular for contact lens, by Czech chemist Otto Wichterle in the 1960s led to the availability of ‘soft’ lenses within a decade. Soft lenses are easily fitted, with greater range of tolerance for a given lens profile. The potential for therapeutic use was recognized contemporaneously with the introduction of soft contact lenses. In the decades that followed, modifications to materials, including increased water content or silicone for the sake of increased oxygen permeability, or modifications to improve wetting, were introduced in the field of soft contact lenses. Oxygen transmission has been held as the paragon for therapeutic lens, but mechanical interaction with the surface is also key to tolerance and clinical effectiveness. A North American survey of ‘bandage’ soft lens use by optometrists and ophthalmologist in 2002 found that 72% of respondents had prescribed soft contact lenses for therapeutic purposes, most typically for corneal wound healing and management of postoperative complications.4 In the 2007 Report of the International Dry Eye Workshop,5 contact lens wear is among the treatment recommendations by severity level among level 3 interventions along with autologous serum tears and permanent punctal occlusion, with systemic treatment and surgery listed as level 4 interventions. Some are skeptical that a contact lens for ocular surface disease is therapeutic. One might ask how an object ‘hard’ or ‘soft’ can help an eye that is dry (and inflamed). Clinical observations are that an appropriately chosen, well-fitted therapeutic contact lens can: Consideration of mechanisms underlying these observations, some of which remain part hypothetical, is beyond the scope of this chapter. The prototype therapeutic contact lens was the Bausch & Lomb Plano T, a hydrophilic hydrogel introduced in the 1970s specifically as a therapeutic lens. It had low water content (38%), low oxygen permeability (Dk 8.4), and was thick. Clinically, it reduced pain, promoted epithelialization, sealed leaks, and induced corneal edema (which was good for leaks but bad for other indications). The Permalens (CooperVision Inc, Fairport, NY) represented a significant advance with higher Dk value of 42. It was developed as an extended-wear lens for aphakia to be changed monthly, but its properties in low powers were advantageous over a Plano T lens for therapeutic indications. When programmed replacement and disposable lenses for correction of refractive error entered the marketplace, clinicians chose these for OSD because of immediate availability among trial inventories and relative low cost,6,7 even though they were not labeled for therapeutic use. The Silsoft (Bausch & Lomb Inc, Rochester, NY) is the most gas-permeable soft lens (Dk 340); it is specifically approved for extended wear for the therapeutic indication of correction of pediatric aphakia. These lenses typically have required high lens plus power and larger diameter to support that power, all reducing availability of atmospheric oxygen to the cornea.8 In the last decade, very high Dk silicone hydrogel (SiHy) material and lenses have been developed and labeled specifically for therapeutic use in addition to cosmetic use. There have been reports of the utility of SiHy lenses as a therapeutic option across the spectrum of ocular surface disease.9,10 Epidemiologic studies have not found a lower rate of infection with these newer materials,11,12 but there should be advantages conferred in OSD simply because of their higher oxygen transmission. The authors recommend that clinicians choose a high Dk lens labeled for extended wear and/or therapeutic use as a first choice for therapeutic use in OSD (Fig. 35.1). Potential complications, including lens loss, lens deposits, discomfort, infectious keratitis and ulceration, and tight lens syndrome7 should be reviewed. The risks and benefits of overnight wear should be reviewed with the patient and weighed against the alternatives for the treatment of their particular disease process. It is probably not advisable to use a daily disposable lens on an extended wear or therapeutic basis as they were not developed or manufactured for those uses. Table 35.1 presents some lenses of historical and current interest, with their Dk, percentage water content, and labeling. Some soft lenses are labeled for therapeutic use on an extended wear basis. Others are labeled for extended wear, but not specifically for therapeutic use. Lenses labeled for daily wear could be used ‘off- label’ on an extended wear basis. Lenses labeled for extended wear on a cosmetic basis could be used ‘off-label’ on a therapeutic basis. There are very-large-diameter hydrogel lenses (16–24 mm diameter) that have special utility in instances of OSD in which there is history or likelihood of poor soft lens retention. Profound aqueous deficiency, incomplete blink, lid abnormalities, eye rubbing, and exposure can all be contributory to poor retention (Fig. 35.2). Large-diameter soft lenses sold in range of base curves for a given diameter and the lenses with larger diameters will have central and peripheral zones of different diameters. Ideally, an assortment of diameters and curvatures are kept on hand, and best fit, tolerance, and retention are assessed with empiric trials. Large-diameter soft lenses in SiHy materials have recently become available on a custom-order basis. In 1983, Ezekiel3 reported the use of gas-permeable material in a scleral or ‘haptic’ lens solving the problem of hypoxia in a large-diameter contact lens. This innovation was applied successfully in that decade in innovative large-diameter RGP lens designs at centers of excellence around the world.13–15 The Dk of RGP materials has exceeded that of soft lens materials until the advent of SiHy materials for soft lenses in the past decade. Once hypoxia was conquered by these high-Dk RGP materials, lens suction was the next challenge. Suction was circumvented, literally, by fenestration, which allows for air ventilation, or by haptic design with channels or contours that allow for fluid ventilation with no intrusion of air bubbles. Air ventilation is often satisfactory for eyes with optical indications, such as keratoconus or post-keratoplasty astigmatism, but air bubble(s) are typically not well tolerated in ocular surface disease. Reports of utility of RGP scleral lenses for OSD in general have emerged over the past two decades.13,14,16–19
Contact Lenses for Ocular Surface Disease
History of Contact Lenses and Innovations Allowing for Therapeutic Use
Characteristics of Soft Lenses Used for Treatment of Ocular Surface Disease
Very Large Diameter Soft Lenses
Characteristics of Scleral Lenses Used for Treatment of Ocular Surface Disease
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ento Key
Fastest Otolaryngology & Ophthalmology Insight Engine