Conjunctiva
Inflammation of the conjunctiva (conjunctivitis) is the most common eye disease worldwide. It varies in severity from a mild hyperemia with tearing to a severe conjunctivitis with copious purulent discharge. The cause is usually exogenous, but rarely may be endogenous.
The types of conjunctivitis and their most common causes are summarized in Tables 5–1 and 5–2. Conjunctival inflammation that occurs in the setting of uveitis, or scleral or episcleral inflammation is discussed in Chapter 7.
| Bacterial |
| Hyperacute (purulent) |
| Neisseria gonorrhoeae |
| Neisseria meningitidis |
| Neisseria gonorrhoeae subspecies kochii |
| Acute (mucopurulent) |
| Pneumococcus (Streptococcus pneumoniae) (temperate climates) |
| Haemophilus aegyptius (Koch-Weeks bacillus) (tropical climates) |
| Subacute |
| Haemophilus influenzae (temperate climates) |
| Chronic, including blepharoconjunctivitis |
| Staphylococcus aureus |
| Moraxella lacunata (diplobacillus of Morax-Axenfeld) |
| Rare types (acute, subacute, chronic) |
| Streptococci |
| Moraxella catarrhalis |
| Coliforms |
| Proteus |
| Corynebacterium diphtheriae |
| Mycobacterium tuberculosis |
| Chlamydial |
| Trachoma (C trachomatis serovars A–C) |
| Inclusion conjunctivitis (C trachomatis serovars D–K) |
| Lymphogranuloma venereum (LGV) (C trachomatis serovars L1–3) |
| Viral |
| Acute viral follicular conjunctivitis |
| Pharyngoconjunctival fever due to adenoviruses types 3 and 7 and other serotypes |
| Epidemic keratoconjunctivitis due to adenovirus types 8 and 19 |
| Herpes simplex virus |
| Acute hemorrhagic conjunctivitis due to enterovirus type 70; rarely, coxsackievirus type A24 |
| Chronic viral follicular conjunctivitis |
| Molluscum contagiosum virus |
| Viral blepharoconjunctivitis |
| Varicella, herpes zoster due to varicella-zoster virus |
| Measles virus |
| Rickettsial (rare) |
| Nonpurulent conjunctivitis with hyperemia and minimal infiltration, often a feature of rickettsial diseases |
| Typhus |
| Murine typhus |
| Scrub typhus |
| Rocky Mountain spotted fever |
| Mediterranean fever |
| Q fever |
| Fungal (rare) |
| Ulcerative or granulomatous |
| Candida |
| Granulomatous |
| Rhinosporidium seeberi |
| Coccidioides immitis (San Joaquin Valley fever) |
| Sporothrix schenckii |
| Parasitic (rare but important) |
| Chronic conjunctivitis and blepharoconjunctivitis |
| Thelazia californiensis |
| Loa loa |
| Ascaris lumbricoides |
| Trichinella spiralis |
| Schistosoma haematobium (bladder fluke) |
| Taenia solium (cysticercus) |
| Pthirus pubis (Pediculus pubis, public louse) |
| Fly larvae (Oestrus ovis, etc) (ocular myiasis) |
| Immunologic (allergic) |
| Immediate (humoral) hypersensitivity reactions |
| Hay fever conjunctivitis (pollens, grasses, animal danders, etc) |
| Vernal keratoconjunctivitis |
| Atopic keratoconjunctivitis |
| Giant papillary conjunctivitis |
| Delayed (cellular) hypersensitivity reactions |
| Phylctenulosis |
| Mild conjunctivitis secondary to contact blepharitis |
| Autoimmune disease |
| Primary and secondary Sjögren’s syndrome |
| Mucous membrane pemphigoid |
| Chemical or irritative |
| Latrogenic |
| Idoxuridine, brimonidine, apraclonidine, dipivefrin, and other topically applied drugs |
| Preservatives in eye drops |
| Contact lens solutions, particularly their preservatives |
| Occupational |
| Acids |
| Alkalies |
| Smoke |
| Wind |
| Ultraviolet light |
| Caterpillar hair |
| Etiology unknown |
| Folliculosis |
| Chronic follicular conjunctivitis (Orphan’s conjunctivitis, Axenfeld’s conjunctivitis) |
| Ocular rosacea |
| Psoriasis |
| Stevens–Johnson syndrome, toxic epidermal necrolysis, and erythema multiforme |
| Dermatitis herpetiformis |
| Epidermolysis bullosa |
| Superior limbic keratoconjunctivitis |
| Ligneous conjunctivitis |
| Reiter’s syndrome |
| Mucocutaneous lymph node syndrome (Kawasaki disease) |
| Associated with systemic disease |
| Thyroid disease (exposure, congestive) |
| Gouty conjunctivitis |
| Carcinoid conjunctivitis |
| Sarcoidosis |
| Tuberculosis |
| Syphilis |
| Secondary to dacryocystitis or canaliculitis |
| Conjunctivitis secondary to dacryocystitis pneumococci or beta-hemolytic streptococci |
| Conjunctivitis secondary to canaliculitis Actinomyces israelii, Candida species Aspergillus species (rarely) |
| Clinical Findings and Cytology | Viral | Bacterial | Chlamydial | Allergic |
|---|---|---|---|---|
| Itching | Minimal | Minimal | Minimal | Severe |
| Hyperemia | Generalized | Generalized | Generalized | Generalized |
| Tearing | Profuse | Moderate | Moderate | Moderate |
| Exudation | Minimal | Profuse | Profuse | Minimal |
| Preauricular adenopathy | Common | Uncommon | Common only in inclusion conjunctivitis | None |
| In stained scrapings and exudates | Monocytes | Bacteria, PMNs1 | PMNs, plasma cells, inclusion bodies | Eosinophils |
| Associated sore throat and fever | Occasionally | Occasionally | Never | Never |
Because of its location, the conjunctiva is exposed to many microorganisms and other environmental factors. Several mechanisms protect the surface of the eye. In the tear film, the aqueous component dilutes infectious material, mucus traps debris, and a pumping action of the lids constantly flushes the tears to the tear duct. In addition, the tears contain antimicrobial substances, including lysozyme and antibodies (IgG and IgA).
Common pathogens that can cause conjunctivitis include Streptococcus pneumoniae, Haemophilus influenzae, Staphylococcus aureus, Neisseria meningitidis, most human adenovirus strains, herpes simplex virus type 1 and type 2, and two picornaviruses. Two sexually transmitted agents that cause conjunctivitis are Chlamydia trachomatis and Neisseria gonorrhoeae.
Damage to the conjunctival epithelium by a noxious agent may be followed by epithelial edema, cellular death and exfoliation, epithelial hypertrophy, or granuloma formation. There may also be edema of the conjunctival stroma (chemosis) and hypertrophy of the lymphoid layer of the stroma (follicle formation). Inflammatory cells, including neutrophils, eosinophils, basophils, lymphocytes, and plasma cells, may be seen and often indicate the nature of the damaging agent. These cells migrate from the conjunctival stroma through the epithelium to the surface. They then combine with fibrin and mucus from the goblet cells to form conjunctival exudate, which is responsible for the “mattering” on the lid margins (especially in the morning).
The inflammatory cells appear in the exudate or in scrapings taken with a sterile platinum spatula from the anesthetized conjunctival surface. The material is stained with Gram’s stain (to identify the bacterial organisms) and with Giemsa’s stain (to identify the cell types and morphology). A predominance of polymorphonuclear leukocytes is characteristic of bacterial conjunctivitis. Generally, a predominance of mononuclear cells—especially lymphocytes—is characteristic of viral conjunctivitis. If a pseudomembrane or true membrane is present (eg, epidemic keratoconjunctivitis or herpes simplex virus conjunctivitis), neutrophils usually predominate because of coexistent necrosis. In chlamydial conjunctivitis, neutrophils and lymphocytes are generally present in equal numbers.
In allergic conjunctivitis, eosinophils and basophils are frequently present in conjunctival biopsies, but they are less common on conjunctival smears; eosinophils or eosinophilic granules are commonly found in vernal keratoconjunctivitis. High levels of proteins secreted by eosinophils (eg, eosinophil cationic protein) can be found in the tears of patients with vernal, atopic, or allergic conjunctivitis. Eosinophils and basophils are found in allergic conjunctivitis, and scattered eosinophilic granules and eosinophils are found in vernal keratoconjunctivitis. In all types of conjunctivitis, there are plasma cells in the conjunctival stroma. Unlike other inflammatory cells, they do not migrate through the epithelium, and are therefore not present in smears of exudate or of scrapings from the conjunctival surface unless the epithelium has become necrotic (eg, trachoma). In trachoma, the rupturing of a follicle allows the plasma cells to reach the epithelial surface. As the mature follicles of trachoma rupture easily, the finding of large, pale-staining lymphoblastic (germinal-center) cells in scrapings strongly suggests trachoma.
The important symptoms of conjunctivitis include foreign body sensation, scratching or burning sensation, sensation of fullness around the eyes, itching, and photophobia.
Foreign body sensation and scratching or burning sensation are often associated with the swelling and papillary hypertrophy that normally accompany conjunctival hyperemia. Pain rather than discomfort commonly indicates corneal involvement.
The important signs of conjunctivitis include hyperemia, tearing, exudation, pseudoptosis, papillary hypertrophy, chemosis, follicles, pseudomembranes and membranes, granulomas, and preauricular adenopathy.
Hyperemia is the most conspicuous clinical sign of acute conjunctivitis. The redness is most marked in the fornix and diminishes toward the limbus by virtue of the dilation of the posterior conjunctival vessels. (A perilimbal dilation or ciliary flush suggests inflammation of the cornea or deeper structures.) A brilliant red suggests bacterial conjunctivitis, whereas a milky appearance suggests allergic conjunctivitis. Hyperemia without cellular infiltration suggests irritation from physical causes, such as wind, sun, smoke, etc, but it may occur occasionally with diseases associated with vascular instability (eg, acne rosacea).
Tearing (epiphora) is often prominent in conjunctivitis, the tears resulting from the foreign body sensation, the burning or scratching sensation, or the itching. Mild transudation also arises from the hyperemic vessels and adds to the tearing. An abnormally scant secretion of tears and an increase in mucous filaments suggest dry eye syndrome.
Exudation is a feature of all types of acute conjunctivitis. The exudate is flaky and amorphous in bacterial conjunctivitis and stringy in allergic conjunctivitis. “Mattering” of the eyelids occurs upon awakening in almost all types of conjunctivitis, and if the exudate is copious and the lids are firmly stuck together, the conjunctivitis is probably bacterial or chlamydial.
Pseudoptosis is a drooping of the upper lid secondary to infiltration and inflammation of Müller’s muscle. The condition is seen in several types of severe conjunctivitis, for example trachoma and epidemic keratoconjunctivitis.
Papillary hypertrophy is a nonspecific conjunctival reaction that occurs because the conjunctiva is bound down to the underlying tarsus or limbus by fine fibrils. When the tuft of vessels that forms the substance of the papilla (along with cellular elements and exudates) reaches the basement membrane of the epithelium, it branches over the papilla like the spokes in the frame of an umbrella. An inflammatory exudate accumulates between the fibrils, heaping the conjunctiva into mounds. In necrotizing disease (eg, trachoma), the exudate may be replaced by granulation tissue or connective tissue.
When the papillae are small, the conjunctiva usually has a smooth, velvety appearance. A red papillary conjunctiva suggests bacterial or chlamydial disease (eg, a velvety red palpebral conjunctiva is characteristic of acute trachoma). With marked infiltration of the conjunctiva, giant papillae form. Also called “cobblestone papillae” in vernal keratoconjunctivitis because of their crowded appearance, giant papillae are flat-topped, polygonal, and milky-red in color. On the upper tarsus, they suggest vernal keratoconjunctivitis and giant papillary conjunctivitis with contact lens sensitivities; on the lower tarsus, they suggest atopic keratoconjunctivitis. Giant papillae may also occur at the limbus, especially in the area that is normally exposed when the eyes are open (between 2 and 4 o’clock and between 8 and 10 o’clock). Here they appear as gelatinous mounds that may encroach on the cornea. Limbal papillae are characteristic of vernal keratoconjunctivitis but rarely occur in atopic keratoconjunctivitis.
Chemosis of the conjunctiva strongly suggests acute allergic conjunctivitis but may also occur in acute gonococcal or meningococcal conjunctivitis and especially in adenoviral conjunctivitis. Chemosis of the bulbar conjunctiva is seen in patients with trichinosis. Occasionally, chemosis may appear before there is any gross cellular infiltration or exudation.
Follicles are seen in most cases of viral conjunctivitis, in all cases of chlamydial conjunctivitis except neonatal inclusion conjunctivitis, in some cases of parasitic conjunctivitis, and in some cases of toxic conjunctivitis induced by topical medications such as idoxuridine, brimonidine, apraclonidine, and dipivefrin, or by preservatives in eye drops or contact lens solutions. Follicles in the inferior fornix and at the tarsal margins have limited diagnostic value, but when they are located on the tarsi (especially the upper tarsus), chlamydial, viral, or toxic conjunctivitis (following topical medication) should be suspected.
The follicle consists of a focal lymphoid hyperplasia within the lymphoid layer of the conjunctiva and usually contains a germinal center. Clinically, it can be recognized as a rounded, avascular white or gray structure. On slitlamp examination, small vessels can be seen arising at the border of the follicle and encircling it.
Pseudomembranes and membranes are the result of an exudative process and differ only in degree. A pseudomembrane is a coagulum on the surface of the epithelium, and when it is removed, the epithelium remains intact. In contrast, a true membrane is a coagulum involving the entire epithelium, and if it is removed, a raw, bleeding surface remains. Both pseudomembranes and membranes may accompany epidemic keratoconjunctivitis, primary herpes simplex virus conjunctivitis, streptococcal conjunctivitis, diphtheria, mucous membrane pemphigoid, Stevens–Johnson syndrome, toxic epidermal necrolysis, and erythema multiforme. They may also be an aftermath of chemical exposure, especially alkali burns.
Ligneous conjunctivitis is a peculiar form of recurring membranous conjunctivitis. It is bilateral, seen mainly in children, and predominantly in females. It may be associated with other systemic findings, including nasopharyngitis and vulvovaginitis.
Granulomas of the conjunctiva always affect the stroma and most commonly are chalazia. Other endogenous causes include sarcoidosis, syphilis, cat-scratch disease, and, rarely, coccidioidomycosis. Parinaud’s oculoglandular syndrome includes conjunctival granulomas and a prominent preauricular lymph node, and this group of diseases may require biopsy examination to establish the diagnosis.
Phlyctenules represent a delayed hypersensitivity reaction to microbial antigen, for example staphylococcal or mycobacterial antigens. Phlyctenules of the conjunctiva initially consist of a perivasculitis with lymphocytic cuffing of a vessel. When they progress to ulceration of the conjunctiva, the ulcer bed has many polymorphonuclear leukocytes.
Preauricular lymphadenopathy is an important sign of conjunctivitis. A grossly visible preauricular node is seen in Parinaud’s oculoglandular syndrome and, rarely, in epidemic keratoconjunctivitis. A large or small preauricular node, sometimes slightly tender, occurs in primary herpes simplex conjunctivitis, epidemic keratoconjunctivitis, inclusion conjunctivitis, and trachoma. Small but nontender preauricular lymph nodes tend to occur in pharyngoconjunctival fever and acute hemorrhagic conjunctivitis. Occasionally, preauricular lymphadenopathy may be observed in children with infections of the meibomian glands.
Two forms of bacterial conjunctivitis are recognized: acute (including hyperacute and subacute) and chronic. Acute bacterial conjunctivitis is usually benign and self-limited, lasting no more than 14 days. Treatment with one of the many available antibacterial agents usually cures the condition within a few days. In contrast, hyper-acute (purulent) conjunctivitis caused by N gonorrhoeae or N meningitidis may lead to serious ocular complications if not treated promptly. Chronic conjunctivitis is usually secondary to eyelid disease or nasolacrimal duct obstruction.
The organisms that account for most cases of bacterial conjunctivitis are listed in Table 5–1. Generally it manifests as bilateral irritation and injection, purulent exudate with sticky lids on waking, and occasionally lid edema. The infection usually starts in one eye and may be spread to the eye by direct contact from the hands. It may be spread from one person to another by fomites.
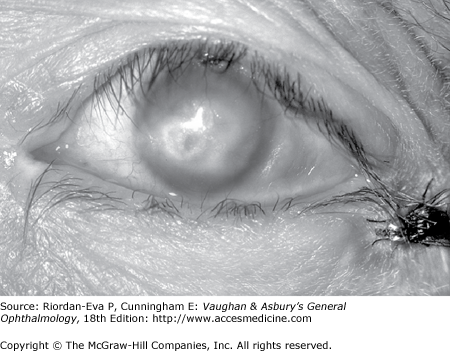
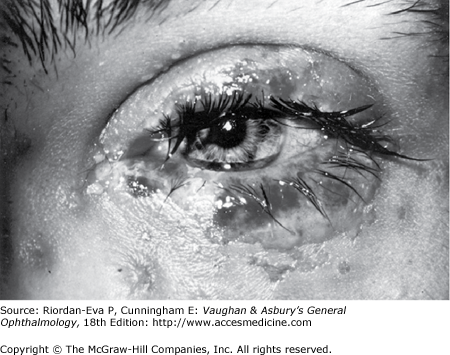
Hyperacute (purulent) bacterial conjunctivitis (caused by N gonorrhoeae, Neisseria kochii, and N meningitidis) is marked by a profuse purulent exudate (Figure 5–1). Meningococcal conjunctivitis may occasionally be seen in children. Any severe, profusely exudative conjunctivitis demands immediate laboratory investigation and immediate treatment. If there is any delay, there may be severe corneal damage or loss of the eye, or the conjunctiva could become the portal of entry for either N gonorrhoeae or N meningitidis, leading to septicemia or meningitis.
Acute mucopurulent (catarrhal) conjunctivitis often occurs in epidemic form and is called “pinkeye” by most laymen. It is characterized by an acute onset of conjunctival hyperemia and a moderate amount of mucopurulent discharge. The most common causes are S pneumoniae in temperate climates and Haemophilus aegyptius in warm climates. Less common causes are staphylococci and other streptococci. The conjunctivitis caused by S pneumoniae and H aegyptius may be accompanied by subconjunctival hemorrhages. H aegyptius conjunctivitis in Brazil has been followed by a fatal purpuric fever produced by a plasmid-associated toxin of the bacteria.
Subacute conjunctivitis is caused most often by H influenzae and occasionally by Escherichia coli and proteus species. H influenzae infection is characterized by a thin, watery, or flocculent exudate.
Chronic bacterial conjunctivitis occurs in patients with nasolacrimal duct obstruction and chronic dacryocystitis, which are usually unilateral. It may also be associated with chronic bacterial blepharitis or meibomian gland dysfunction. Patients with floppy lid syndrome or ectropion may develop secondary bacterial conjunctivitis.
Rarely, bacterial conjunctivitis may be caused by Corynebacterium diphtheriae and Streptococcus pyogenes. Pseudomembranes or membranes caused by these organisms may form on the palpebral conjunctiva. The rare cases of chronic conjunctivitis produced by Moraxella catarrhalis, the coliform bacilli, proteus, etc, are as a rule indistinguishable clinically.
In most cases of bacterial conjunctivitis, the organisms can be identified by the microscopic examination of conjunctival scrapings stained with Gram’s stain or Giemsa’s stain; this reveals numerous polymorphonuclear neutrophils. Conjunctival scrapings for microscopic examination and culture are recommended for all cases and are mandatory if the disease is purulent, membranous, or pseudomembranous. Antibiotic sensitivity studies are also desirable, but empirical antibiotic therapy should be started. When the results of antibiotic sensitivity tests become available, specific antibiotic therapy can then be instituted.
Chronic marginal blepharitis often accompanies staphylococcal conjunctivitis except in very young patients who are not subject to blepharitis. Conjunctival scarring may follow both pseudomembranous and membranous conjunctivitis, and in rare cases corneal ulceration and perforation supervene.
Marginal corneal ulceration may follow infection with N gonorrhoeae, N kochii, N meningitidis, H aegyptius, S aureus, and M catarrhalis; if the toxic products of N gonorrhoeae diffuse through the cornea into the anterior chamber, they may cause toxic iritis.
Specific therapy of bacterial conjunctivitis depends on identification of the microbiologic agent. While waiting for laboratory reports, the physician can start topical therapy with a broad-spectrum antibacterial agent (eg, polymyxin-trimethoprim). In any purulent conjunctivitis in which the Gram stain shows gram-negative diplococci suggestive of neisseria, both systemic and topical therapy should be started immediately. If there is no corneal involvement, a single intramuscular dose of ceftriaxone, 1 g, is usually adequate systemic therapy. If there is corneal involvement, a 5-day course of parenteral ceftriaxone, 1–2 g daily, is required.
In purulent and mucopurulent conjunctivitis, the conjunctival sac should be irrigated with saline solution as necessary to remove the conjunctival secretions. To prevent spread of the disease, the patient and family should be instructed to give special attention to personal hygiene.
Acute bacterial conjunctivitis is almost always self-limited. Untreated, it may last 10–14 days; if properly treated, 1–3 days. The exceptions are staphylococcal conjunctivitis (which may progress to blepharoconjunctivitis and enter a chronic phase) and gonococcal conjunctivitis (which, when untreated, can lead to corneal perforation and endophthalmitis). Since the conjunctiva may be the portal of entry for the meningococcus to the bloodstream and meninges, septicemia and meningitis may be the end results of meningococcal conjunctivitis.
Chronic bacterial conjunctivitis may not be self-limited and may become a troublesome therapeutic problem.
Although worldwide the number of individuals with profound vision loss from trachoma has dropped from 6 million to 1.3 million, trachoma remains one of the leading causes of preventable blindness. It was first recognized as a cause of trichiasis (misdirected lashes) as early as the 27th century BC. It is usually endemic in regions with poor hygiene, overcrowding, poverty, lack of clean water and poor sanitation. Blinding trachoma occurs in many parts of Africa, in some parts of Asia, among Australian aborigines, and in northern Brazil. Communities with milder nonblinding trachoma occur in the same regions and in some areas of Latin America and the Pacific Islands.
Trachoma usually presents bilaterally and often spreads by direct contact or fomites, most often from other family members, who should also be examined for the disease. Insect vectors, especially flies, may play a role in transmission. The acute forms of the disease are more infectious than the cicatricial forms, and the larger the inoculum, the more severe the disease. Spread is often associated with epidemics of bacterial conjunctivitis and with the dry seasons in tropical and semitropical countries.
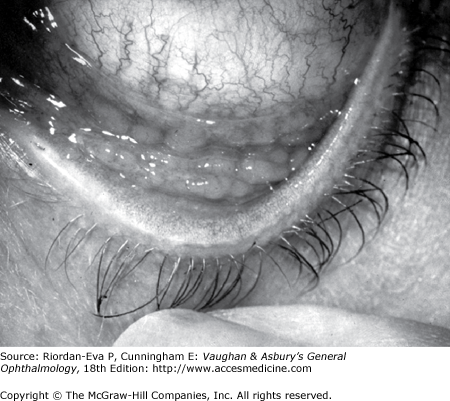
Trachoma begins as a chronic follicular conjunctivitis of childhood that progresses to conjunctival scarring (Figure 5–2). In severe cases, trichiasis occurs in early adult life as a result of severe conjunctival scarring. The constant abrasion of inturned lashes and a defective tear film lead to corneal scarring, usually after the age of 30 years (Figure 5–3).
The incubation period of trachoma averages 7 days but varies from 5–14 days. In an infant or child, the onset is usually insidious, and the disease may resolve with minimal or no complications. In adults, the onset is often subacute or acute, and complications may develop early. At onset, trachoma often resembles other bacterial conjunctivitis. The signs and symptoms usually consist of tearing, photophobia, pain, exudation, edema of the eyelids, chemosis of the bulbar conjunctiva, hyperemia, papillary hypertrophy, tarsal and limbal follicles, superior keratitis, pannus formation, and a small, tender preauricular node.
In established trachoma, there may also be superior epithelial keratitis, subepithelial keratitis, pannus, or superior limbal follicles, and ultimately the pathognomonic cicatricial remains of these follicles, known as Herbert’s pits—small depressions covered by epithelium at the limbocorneal junction. The associated pannus is a fibrovascular membrane arising from the limbus, with vascular loops extending onto the cornea. All of the signs of trachoma are more severe in the upper than in the lower conjunctiva and cornea.
To establish the presence of endemic trachoma in a family or community, a substantial number of children must have at least two of the following signs:
Five or more follicles on the flat palpebral conjunctiva lining the upper eye lid.
Typical conjunctival scarring of the upper palpebral conjunctiva.
Limbal follicles or their sequelae (Herbert’s pits).
An even extension of blood vessels on to the cornea, most marked at the upper limbus.
While occasional individuals will meet these criteria, it is the wide distribution of these signs in individual families and in a community that identify the presence of trachoma.
For control purposes, the World Health Organization has developed a simplified method to describe the disease (Table 5–3).
| TF: | Five or more follicles on the upper palpebral conjunctiva. |
| TI: | Diffuse infiltration and papillary hypertrophy of the upper palpebral conjunctiva obscuring at least 50% of the normal deep vessels. |
| TS: | Trachomatous conjunctival scarring. |
| TT: | Trichiasis or entropion (inturned eyelashes). |
| CO: | Corneal opacity. |
The presence of TF and TI indicates active infectious trachoma and a need for treatment. TS is evidence of damage from the disease. TT is potentially blinding and is an indication for corrective lid surgery. CO is the final blinding lesion of trachoma.
Chlamydial inclusion bodies may be found in Giemsa-stained conjunctival scrapings, but they are not always present. Inclusions appear in the Giemsa-stained preparations as particulate, dark purple, or blue cytoplasmic masses that cap the nucleus of the epithelial cell. Fluorescent antibody stains and enzyme immunoassay tests are available commercially and are widely used in clinical laboratories. These and other new tests, including polymerase chain reaction (PCR), have superseded Giemsa staining of conjunctival smears and isolation of chlamydial agent in cell culture.
The agent of trachoma resembles the agent of inclusion conjunctivitis morphologically, but the two can be differentiated serologically by microimmunofluorescence. Trachoma is usually caused by C trachomatis serovars A, B, Ba, or C.
Epidemiologic and clinical factors to be considered in differentiating trachoma from other forms of follicular conjunctivitis can be summarized as follows:
No history of exposure to endemic trachoma speaks against the diagnosis.
Viral follicular conjunctivitis (due to infection with adenovirus, herpes simplex virus, picornavirus, and coxsackievirus) usually has an acute onset and is clearly resolving by 2–3 weeks.
Infection with genitally transmitted chlamydial strains usually has an acute onset in sexually active individuals.
Chronic follicular conjunctivitis with exogenous substances (molluscum nodules of the lids, topical eye medications) resolve slowly when the nodules are removed or the drug is withdrawn.
Parinaud’s oculoglandular syndrome is manifested by massively enlarged preauricular or cervical lymph nodes, although the conjunctival lesion may be follicular.
Young children often have some follicles (like hypertrophied tonsils), a condition known as folliculosis.
The atopic conditions vernal conjunctivitis and atopic keratoconjunctivitis are associated with giant papillae that are elevated and often polygonal, with a milky-red appearance. Eosinophils are present in smears.
Look for a history of contact lens intolerance in patients with conjunctival scarring and pannus; giant papillae in some contact lens wearers can be confused with trachoma follicles.
Conjunctival scarring occur as a frequent complication of trachoma and can destroy the accessory lacrimal glands and obliterate the ductules of the lacrimal gland. These effects may drastically reduce the aqueous component of the precorneal tear film, and the film’s mucous components may be reduced by loss of goblet cells. The scars may also cause distortion of the upper lid with inward deviation of individual lashes (trichiasis) or of the whole lid margin (entropion), so that the lashes constantly abrade the cornea. This often leads to corneal ulceration, bacterial corneal infections, and corneal scarring.
Ptosis, nasolacrimal duct obstruction, and dacryocystitis are other common complications of trachoma.
Striking clinical improvement can usually be achieved with tetracycline, 1–1.5 g/d orally in four divided doses for 3–4 weeks; doxycycline, 100 mg orally twice daily for 3 weeks; or erythromycin, 1 g/d orally in four divided doses for 3–4 weeks. Several courses are sometimes necessary for actual cure. Systemic tetracyclines should not be given to a child under 7 years of age or to a pregnant woman. Tetracycline binds to calcium in the developing teeth and in growing bone and may lead to congenital yellowish discoloration of the permanent teeth and skeletal (eg, clavicular) abnormalities. Recent studies in developing countries have demonstrated that azithromycin is an effective treatment for trachoma given orally as a 1-g dose in children. Because of minimal side effects and ease of administration, this macrolide antibiotic has become the drug of choice for mass treatment campaigns.
Topical ointments or drops, including preparations of sulfonamides, tetracyclines, erythromycin, and rifampin, used four times daily for 6 weeks, are equally effective.
From the time therapy is begun, its maximum effect is usually not achieved for 10–12 weeks. The persistence of follicles on the upper tarsus for some weeks after a course of therapy should therefore not be construed as evidence of therapeutic failure.
Surgical correction of trichiasis is essential to prevent scarring from late trachoma in developing countries. Such surgery is increasingly done by nonspecialist physicians or specially trained auxiliary personnel.
Characteristically, trachoma is a chronic disease of long duration. Under good hygienic conditions (specifically, face-washing of young children), the disease resolves or becomes milder so that severe sequelae are avoided.
Inclusion conjunctivitis is often bilateral and usually occurs in sexually active young people. The chlamydial agent infects the urethra of the male and the cervix of the female. Transmission to the eyes of adults is usually by oral-genital sexual practices or hand to eye transmission. About 1 in 300 persons with genital chlamydial infection develops the eye disease. Indirect transmission has been reported to occur in inadequately chlorinated swimming pools. In newborns, the agent is transmitted during birth by direct contamination of the conjunctiva with cervical secretions. Credé prophylaxis (1% silver nitrate) gives only partial protection against inclusion conjunctivitis.
Inclusion conjunctivitis may have an acute or a subacute onset. The patient frequently complains of redness, pseudo-ptosis, and discharge, especially in the mornings. Newborns have papillary conjunctivitis and a moderate amount of exudate, and in hyper-acute cases, pseudomembranes occasionally form and can lead to scarring. Since the newborn has no adenoid tissue in the stroma of the conjunctiva, there is no follicle formation; but if the conjunctivitis persists for 2–3 months follicles appear, similar to the conjunctival picture in older children and adults. In the newborn, chlamydial infection may cause pharyngitis, otitis media, and interstitial pneumonitis.
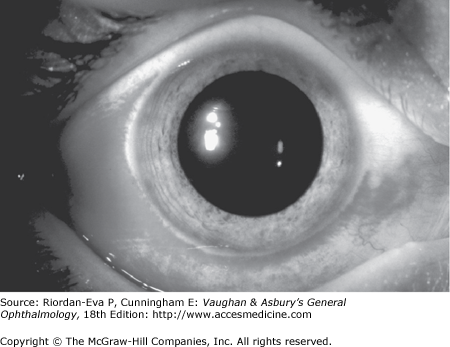
In adults, the conjunctiva of both tarsi—especially the lower tarsus—have papillae and follicles (Figure 5–4). Since pseudomembranes do not usually form in the adult, scarring does not usually occur. Superficial keratitis may be noted superiorly and, less often, a small superior micropannus (<1–2 mm). Subepithelial opacities, usually marginal, often develop. Otitis media may occur as a result of infection of the auditory tube.
Because of the sexually transmitted nature of adult inclusion conjunctivitis and the need for systemic treatment of the patient and the patient’s sexual partners, rapid diagnostic tests such as the direct fluorescent antibody test and enzyme-linked immunosorbent assay (ELISA) and PCR have replaced Giemsa staining in routine clinical practice. In the case of chlamydial ophthalmia neonatorum, rapid diagnosis is also imperative to prevent systemic complications such as chlamydial pneumonitis. Inclusion conjunctivitis is usually caused by C trachomatis serovars D–K with occasional isolations of serotype B. Serologic determinations are not useful in the diagnosis of ocular infections, but measurement of IgM antibody levels is extremely valuable in the diagnosis of chlamydial pneumonitis in infants.
Inclusion conjunctivitis can be clinically differentiated from trachoma on the following grounds:
Active, follicular trachoma occurs commonly in young children or others living in or exposed to a community with endemic trachoma; inclusion conjunctivitis occurs in sexually active adolescents or adults.
Conjunctival scarring is very rare in adult inclusion conjunctivitis.
Herbert’s pits serve as a hallmark of previous trachoma infection.
Oral erythromycin suspension, 50 mg/kg/d in four divided doses for at least 14 days may be used to treat infants. Systemic treatment is necessary because chlamydial infection also involves the respiratory and gastrointestinal tracts. Topical antibiotics (tetracyclines, erythromycin, sulfonamides) are not useful in newborns treated with oral erythromycin. Both parents also should be treated with oral tetracycline or erythromycin.
In adults, cure of chalmydial disease can be achieved with doxycycline, 100 mg orally twice daily for 7 days; erythromycin, 2 g/d for 7 days, or possibly azithromycin 1 g in a single dose. (Systemic tetracyclines should not be given to a pregnant woman or a child under 7 years of age, since they cause epiphysial problems in the fetus or staining of the young child’s teeth.) The patient’s sexual partners should be examined and treated.
When one of the standard therapeutic regimens is followed, recurrences are rare. If untreated, inclusion conjunctivitis runs a course of 3–9 months or longer with an average duration of 5 months.
Lymphogranuloma venereum conjunctivitis is a rare sexually transmitted disease, manifesting as dramatic granulomatous conjunctival reaction with greatly enlarged preauricular nodes (Parinaud’s syndrome). It is caused by C trachomatis serovars L1, L2, or L3.
Chlamydia psittaci only rarely causes conjunctivitis in humans. Strains from parrots (psittacosis) and cats (feline pneumonitis) have caused follicular conjunctivitis in humans. The prototype strains of C pneumoniae were isolated from the conjunctiva but have not been identified as a cause of ocular disease.
Viral conjunctivitis, a common affliction, can be caused by a wide variety of viruses. Severity ranges from severe, disabling disease to mild, rapidly self-limited infection.
Pharyngoconjunctival fever is characterized by fever of 38.3–40°C, sore throat, and a follicular conjunctivitis in one or both eyes. The follicles are often very prominent on both the conjunctiva (Figure 5–5) and the pharyngeal mucosa. The disease can be either bilateral or unilateral. Injection and tearing often occur, and there may be transient superficial epithelial keratitis and occasionally some subepithelial opacities. Preauricular lymphadenopathy (nontender) is characteristic. The syndrome may be incomplete, consisting of only one or two of the cardinal signs (fever, pharyngitis, and conjunctivitis).
Pharyngoconjunctival fever is most frequently caused by adenovirus type 3 and occasionally by types 4 and 7. The virus can be grown on HeLa cells and identified by neutralization tests. As the disease progresses, it can also be diagnosed serologically by a rising titer of neutralizing antibody to the virus. Clinical diagnosis is a simple matter, however, and clearly more practical.
Conjunctival scrapings contain predominantly mononuclear cells, and no bacteria grow in cultures. The condition is more common in children than in adults and can be transmitted in poorly chlorinated swimming pools. The conjunctivitis is self-limited, and as such, only supportive treatment is indicated, with the episode resolving in approximately 10 days.
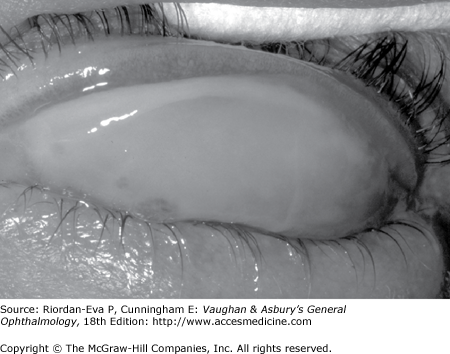
The onset of epidemic keratoconjunctivitis is often unilateral, with both eyes subsequently being affected but the first eye usually being more severely affected. Initial symptoms include conjunctival injection, moderate pain, and tearing. Usually by 5–14 days, photophobia, epithelial keratitis, and round subepithelial opacities have also developed (Figure 5–6). Corneal sensation is normal. A tender preauricular node is characteristic. Edema of the eyelids, chemosis, and conjunctival hyperemia mark the acute phase, with follicles and subconjunctival hemorrhages often appearing within 48 hours. Pseudomembranes (Figure 5–7) (and occasionally true membranes) may occur and may be followed by flat scars or symblepharon formation.
The conjunctivitis usually resolves by 3–4 weeks at most. The subepithelial opacities are concentrated in the central cornea, usually sparing the periphery, and may persist for months but generally heal without scars.
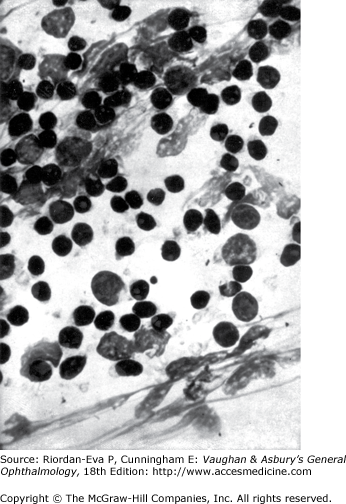
Epidemic keratoconjunctivitis is caused by adenovirus types 8, 19, 29, and 37 (subgroup D of the human adenoviruses). They can be isolated in cell culture and identified by neutralization tests. Scrapings from the conjunctiva show a primarily mononuclear inflammatory reaction (Figure 5–8); when pseudomembranes occur, neutrophils may also be prominent.
Epidemic keratoconjunctivitis in adults is confined to the external eye, but in children there may be systemic symptoms of viral infection as fever, sore throat, otitis media, and diarrhea. Nosocomial transmission during eye examinations takes place all too often by way of the physician’s examination, use of improperly sterilized ophthalmic instruments, or use of contaminated solutions. Eye solutions, particularly topical anesthetics, can be contaminated when a dropper tip aspirates infected material from the conjunctiva or cilia. The virus can persist in the solution, which becomes a source of spread.
The danger of contaminated solution bottles can be avoided by the use of individual sterile droppers or unit-dose packages of eye drops. Regular hand washing between examinations and careful cleaning and sterilization of instruments that touch the eyes—especially tonometers—are also mandatory. Applanation tonometers should be cleaned by wiping with alcohol or hypochlorite, then rinsing with sterile water and carefully drying.
There is no specific therapy at present, but cold compresses and artificial tears will relieve some symptoms. Corticosteroids utilized during acute conjunctivitis may prolong late corneal involvement and should be avoided whenever possible. Antibacterial agents should be administered if bacterial superinfection occurs.
Herpes simplex virus (HSV) conjunctivitis, usually a disease of young children, is an uncommon entity characterized by unilateral injection, irritation, mucoid discharge, pain, and mild photophobia. It occurs during primary infection with HSV or during recurrent episodes of ocular herpes (Figure 5–9). It is often associated with herpes simplex keratitis, in which the cornea shows discrete epithelial lesions that usually coalesce to form single or multiple branching epithelial (dendritic) ulcers (Figure 5–10). The conjunctivitis is follicular or, less often, pseudomembranous. (Patients receiving topical antivirals may develop follicular conjunctivitis that can be differentiated because the herpetic follicular conjunctivitis has an acute onset.) Herpetic vesicles may sometimes appear on the eyelids and lid margins, associated with severe edema of the eyelids. Typically, there is a small tender preauricular node.
No bacteria are found in scrapings or recovered in cultures. If the conjunctivitis is follicular, the predominant inflammatory reaction is mononuclear, but if it is pseudomembranous, the predominant reaction is polymorphonuclear, owing to the chemotaxis of necrosis. Intranuclear inclusions (because of the margination of the chromatin) can be seen in conjunctival and corneal cells if Bouin fixation and the Papanicolaou stain are used but not in Giemsa-stained smears. The finding of multinucleated giant epithelial cells has diagnostic value.
The virus can be readily isolated by gently rubbing a dry Dacron or calcium alginate swab over the conjunctiva and transferring the infected cells to a susceptible tissue culture.
HSV conjunctivitis may persist for 2–3 weeks, and if it is pseudomembranous, it may leave fine linear or flat scars. Complications consist of corneal involvement (including dendrites) and vesicles on the skin. Although type 1 herpesvirus causes the overwhelming majority of ocular cases, type 2 is the usual cause of herpetic conjunctivitis in newborns and a rare cause in adults. In the newborn, there may be generalized disease with encephalitis, chorioretinitis, hepatitis, etc. Any HSV infection in the newborn must be treated with systemic antiviral therapy (acyclovir) and monitored in a hospital setting.
If the conjunctivitis occurs in a child over 1 year of age or in an adult, it is usually self-limited and may not require therapy. Topical or systemic antivirals should be given, however, to prevent corneal involvement. For corneal ulcers, corneal debridement may be performed by gently wiping the ulcer with a dry cotton swab, applying antiviral drops, and patching the eye for 24 hours. Topical antivirals alone should be applied for 7–10 days (eg, trifluridine every 2 hours while awake). Herpetic keratitis may also be treated with 3% acyclovir ointment (not available in the United States) five times daily for 10 days, or with oral acyclovir, 400 mg five times daily for 7 days. Corticosteroid use is contraindicated since it may aggravate herpetic infections causing a prolonged and usually more severe course.
Newcastle disease conjunctivitis is a rare disorder characterized by burning, itching, pain, redness, tearing, and (rarely) blurring of vision. It often occurs in small epidemics among poultry workers handling infected birds or among veterinarians or laboratory helpers working with live vaccines or virus.
The conjunctivitis resembles that caused by other viral agents, with chemosis, a small preauricular node, and follicles on the upper and lower tarsus. No treatment is available or necessary for this self-limited disease.
All of the continents and most of the islands of the world have had major epidemics of acute hemorrhagic conjunctivitis. It was first recognized in Ghana in 1969. It is caused by enterovirus type 70 and occasionally by coxsackievirus A24.
Characteristically, the disease has a short incubation period (8–48 hours) and course (5–7 days). The usual signs and symptoms are pain, photophobia, foreign-body sensation, copious tearing, redness, lid edema, and subconjunctival hemorrhages (Figure 5–11). Chemosis sometimes also occurs. The subconjunctival hemorrhages are usually diffuse but may be punctate at onset, beginning in the upper bulbar conjunctiva and spreading to the lower. Most patients have preauricular lymphadenopathy, conjunctival follicles, and epithelial keratitis. Anterior uveitis has been reported; fever, malaise, and generalized myalgia have been observed in 25% of cases; and motor paralysis of the lower extremities has occurred in rare cases in India and Japan.
The virus is transmitted by close person-to-person contact and by such fomites as common linens, contaminated optical instruments, and water. Recovery occurs within 5–7 days, and there is no known treatment. In the United States, at times closure of schools has been needed to stop epidemics.
A molluscum nodule on the lid margins or the skin of the lids or brow may produce unilateral chronic follicular conjunctivitis, superior keratitis, and superior pannus that resembles trachoma. The inflammatory reaction is predominantly mononuclear (unlike the reaction in trachoma), and the round, waxy, pearly-white, noninflammatory lesion with an umbilicated center is typical of molluscum contagiosum (Figure 5–12). Biopsy shows eosinophilic cytoplasmic inclusions that fill the entire cytoplasm of the enlarged cell, pushing its nucleus to one side.
Excision or simple incision of the nodule, thus allowing peripheral blood to permeate it, or cryotherapy cures the conjunctivitis. On very rare occasions, molluscum nodules have occurred on the conjunctiva. In these cases, excision of the nodule has also relieved the conjunctivitis. Multiple lid or facial lesions of molluscum contagiosum occur in patients with AIDS.
Hyperemia and an infiltrative conjunctivitis—associated with the typical vesicular eruption along the dermatomal distribution of the ophthalmic branch of the trigeminal nerve (Figure 5–13) —are characteristic of ophthalmic (herpes) zoster (shingles), due to reactivation of varicella-zoster virus infection. The conjunctivitis is usually papillary, but follicles, pseudomembranes, and transitory vesicles that later ulcerate have all been noted. A tender preauricular lymph node occurs early in the disease. Scarring of the lid, entropion, and the misdirection of individual lashes are sequelae.
The lid lesions of varicella, which are like the skin lesions (pox) elsewhere, may appear on both the lid margins and the lids and often leave scars. A mild exudative conjunctivitis often occurs, but discrete conjunctival lesions (except at the limbus) are very rare. Limbal lesions resemble phlyctenules and may go through all the stages of vesicle, papule, and ulcer. The adjacent cornea becomes infiltrated and may vascularize.
In both zoster and varicella, scrapings from lid vesicles contain giant cells and a predominance of polymorphonuclear leukocytes; scrapings from the conjunctiva in varicella and from conjunctival vesicles in zoster may contain giant cells and monocytes. The virus can be recovered in tissue cultures of human embryo cells.
In the immunocompetent, oral antiviral therapy (acyclovir 800 mg orally five times daily, famciclovir, 500 mg three times daily, or valacyclovir, 1 g three times daily, all for 7 days), if started within 72 hours after appearance of the rash, reduces the incidence of ocular complications but not necessarily of postherpetic neuralgia. The value of supplementary therapy with oral prednisone, initially 60 mg per day reducing over 3 weeks, is uncertain. In the immunocompromised, oral antiviral therapy should be continued for up to 2 weeks and may need to be given intravenously if there is evidence of progression of disease. Oral prednisone is contraindicated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree