45
Congenital Optic Disc Pits, Morning Glory Disc Anomaly, Optic Nerve Coloboma, and Peripapillary Staphyloma
Dolores Berger  John B. Kerrison
John B. Kerrison  Arthur Korotkin
Arthur Korotkin
CONGENITAL OPTIC DISC PITS
Congenital pits of the optic nerve head are rare congenital anomalies. Although the pathogenesis of optic disc pits is unclear, the great majority of reports in the literature describes optic disc pits as being the mildest variants in the spectrum of optic nerve head colobomas, which are attributed to imperfect closure of the upper end of the embryonic fissure (1). They appear as localized depressions typically measuring from one to several diopters in depth, with a mean of 5 diopters (2). They can be yellow-white, gray, or black in color (Fig. 45-1). It has been suggested that optic disc pits are the mildest manifestation in the spectrum of colobomas involving failure of closure of the embryonic fissure. There are several observations that are inconsistent with this hypothesis. While many colobomas are bilateral and often associated with other abnormalities, optic nerve pits are more typically unilateral and not associated with other findings. The vast majority of pits are solitary, but as many as three pits have been reported in the same optic nerve. There is no known teratogen or genetic inheritance described. Congenital optic disc pits have been associated with trisomy 18 and Alagille syndrome (3).
Optic disc pits were first described in 1882 by Wiethe (4). Although these lesions also were called crater-like holes, cavities, and congenital holes of the optic nerve head, the term “optic disc pit” has become widely accepted (5).
Macular detachment is the most common complication (Fig. 45-2A and B). Kranenburg (6) reviewed the world literature in 1960 and discovered 123 cases of optic disc pit, of which 25% had various types of macular lesions. Additional reports have described serous detachment of the macula secondary to congenital optic disc pits (2, 6–9); however, the source of the subretinal fluid is still uncertain. The detachment typically extends from the retina adjacent to the optic disc pit into the macula, where it may remain asymptomatic or cause visual field defects and diminished central acuity. This typically occurs within the 2nd to 4th decade, although detachments have been reported in children as young as 6 years old (7). Detachments have been primarily associated with optic disc pits that are adjacent to the rim. The detachment is typically not associated with a posterior vitreous detachment and usually involves the macula within the boundaries of the temporal arcades.
Clinical Features
Optic disc pits are considered by most authors to be on the spectrum of embryological anomalies that ranges from small asymptomatic pits to morning glory disc syndrome. Brown and Tasman (5) estimated the incidence of optic disc pits to be approximately one per 10,000 people in the general population, although there is considerable variance among studies (8). Men and women are equally affected. The defect generally ranges in size from 0.25 to 0.40 disc diameters (5). More than 50% are located on the temporal aspect of the disc, but approximately one-third are situated centrally; the remainder are found inferiorly, superiorly, and nasally (5, 10–15). It is rare to find more than one pit, but as many as three have been reported in the same eye (6, 16). Optic disc pits are unilateral in approximately 85% of patients, and the affected disc is larger than the unaffected disc in about 80% of cases (15).
Patients may be asymptomatic or have a visual field defect. With macular involvement, patients may present with loss of central vision. Visual acuity may vary depending on the extent of macular involvement. Visual field defects tend to be located superiorly and temporally as most pits are located inferiorly and nasally in the optic nerve. Arcuate scotomas, Bjerrum-type scotomas, altitudinal defects, paracentral scotomas, enlarged blind spot, generalized scotomas, nasal and temporal steps have all been documented (7). Natural history of pits with symptomatic retinal detachment tends to be that of progressive loss of vision with persistent submacular fluid.
The incidence of posterior vitreous detachment associated with optic disc pits has not been determined (10, 17–21). Brown and Tasman (6) observed posterior vitreous separation in 81%. Vitreous strands are observed occasionally extending from the pit into the vitreous gel. Bonnet (18) reported that 25 eyes with macular detachments associated with optic disc pits did not have posterior vitreous detachments at presentation, and two eyes had spontaneous reattachment of the macula following development of posterior vitreous detachment. Akiba et al. (19) demonstrated posterior vitreous detachments in only two (12%) of 17 eyes with optic disc pits and serous detachments of the macula.
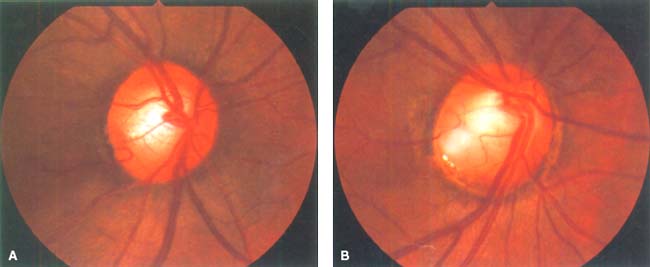
Figure 45-1. Round gray (A) or yellow-white (B) congenital pits of the optic nerve head are present on the temporal aspect of the disc. Peripapillary pigmentary changes and enlarged disc are found.
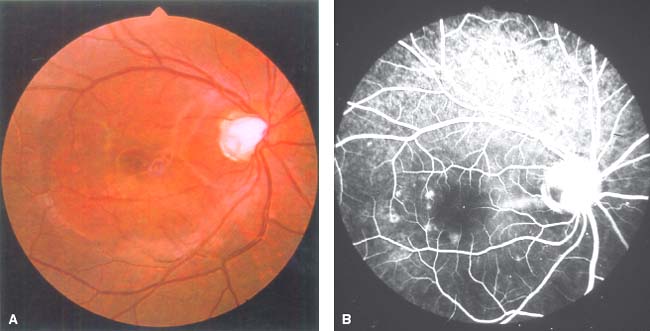
Figure 45-2. A: Color fundus photograph with an optic nerve pit showing subretinal fluid with macular detachment. B: Fluorescein angiogram reveals hypofluorescence of the optic disc pit in the early stage.
Peripapillary retinal pigment epithelial disturbances usually are seen in eyes with optic disc pits along the rim of the disc (20). These peripapillary changes may develop over time with or without central serous retinal detachment.
Macular lesions, such as macular detachment, cystoid degeneration, macular edema, and schisis-like changes, occur in 30% to 50% of eyes with a congenital optic disc pit (6, 15). Among them, serous retinal detachment that may mimic central serous chorioretinopathy is known to be a common complication.
Approximately 40% of eyes have an associated or previous serous detachment of the sensory retina (15). The serous detachment communicates with the optic disc (Figs. 45-2A and B and 45-3). Most of the retinal detachments are temporal to the disc and confined between the superior and inferior vascular arcades. If the pit is present on the nasal side of the disc, a serous retinal detachment is located outside the arcuates. The serous macular detachment generally is shallow (less than 1.0 mm in height) (20). Cystic changes within the detached macula are found in two thirds of cases, and a macular hole develops in about 25%.
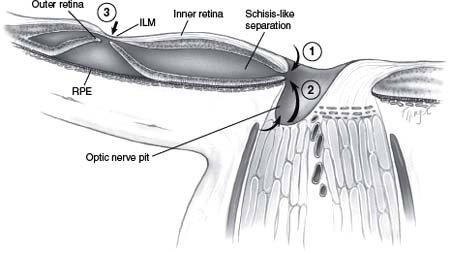
Figure 45-3. Schematic drawing of an axial view of the optic nerve head and surrounding tissues. Various theories describe the mechanism by which fluid enters into the intraretinal space to produce a schisis-like splitting of the neurosensory retina from the vitreous (1) or the cerebrospinal fluid (2). As a late complication, a true macular hole may develop (3). ILM, internal limiting membrane; RPE, retinal pigment epithelium.
A splitting of the retinal layers also has been described in eyes with congenital optic disc pits and retinal detachment (14, 21). Although most authors have assumed that macular detachments are a result of fluid entering directly into the subretinal space, Lincoff et al. (14) proposed that the primary macular lesion is frequently a retinal schisis-like separation that communicates with the optic disc pit. In such eyes, true retinal detachment is regarded as a secondary phenomenon, typically localized to the central macula without connection to the pit. The fluid beneath the photoreceptors is more opaque than the relatively transparent zone of the elevation owing to the schisis-like cavity. Studies by Rutledge et al. (10), using optical coherence tomography (OCT), supported the concept of a bilaminar structure, in which a macular detachment develops secondarily to a pre-existing schisis-like lesion consisting of severe outer retinal edema.
The age of onset of the retinal detachment is variable, with the mean age being about 30 years (15). It has been seen in children within the first decade of life. Centrally located optic nerve head pits generally are not associated with detachment; retinal detachment is seen more commonly with larger, temporally located pits and usually involves the macula (15).
Tiny subretinal precipitates are visible in about one-third of eyes (5). In contrast to most lamellar holes, in which absence of the inner retinal layers is observed, the macular holes noted in conjunction with optic nerve head pits tend to involve the outer retina, giving the appearance that the internal limiting membrane is intact.
Fluorescein Angiography
Fluorescein angiography has shown a variety of findings in patients (17). The optic nerve pit typically appears hypofluorescent in the early phase of the angiogram (Fig. 45-2B), with staining occurring later in the study. It was thought that blood vessels in this area leaked the fluid that entered into the subretinal space (22–25). Brown et al. (5, 15) observed apparent leakage of dye into the subretinal fluid in three eyes with macular detachments and reported a higher incidence of pits in eyes with serous detachments than in eyes without subretinal fluid. There is usually no evidence, however, of dye passing from the pit into the adjacent subretinal fluid in the majority of cases (17).
Visual Field Defects
The optic disc pit can be associated with visual field defects. The most common type of visual field defect is an arcuate scotoma, which occurs in about 25% of cases (2). Arcuate scotomas probably reflect the absence of the wedge of nerve fibers displaced by the optic disc pit. Larger pits may be associated with large Bjerrum-type scotomas or even altitudinal visual field defects. Paracentral scotomas, generalized and peripheral localized constrictions, sector defects extending from the disc, and nasal or temporal steps also may be seen (15).
Central and paracentral scotomas can result from serous macular detachment or retinoschisis (21). Central field loss associated with pure retinoschisis is relatively mild, presumably because many neural pathways remain intact (21). Bridging retinal elements were proposed to explain why an absolute scotoma is not produced by the schisis-like elevation (14, 20).
Optical Coherence Tomography Findings
OCT significantly increased our understanding of ultrastructural features of pit-associated neurosensory detachments. One of the earliest reports by Linkoff et al. (9) demonstrated a division between outer and inner layers of the retina connected to the optic disc pit, which subsequently resolved after pneumatic displacement. Detachment may be associated with retinal edema and cystic degeneration imaged by OCT. The most prominent edema is present in the outer retina at the level of the outer plexiform layer, mimicking a true retinoschisis cavity (10). By OCT, the schisis-like cavity or edematous retina communicates with the optic disc. While some studies report no direct communicant between the optic pit and the subretinal space (10), other studies report that such a communication exists (11).
Systemic Association
In general, systemic abnormalities have not been observed in association with congenital optic disc pits. Nevertheless, basal encephalocele and agenesis of the corpus callosum have been reported (22, 23). A hereditary pattern is not usually present, although an autosomal dominant inheritance that is not associated with mutation in the PAX2 gene has been noted (24).
Many reports in the literature suggest that the pathogenesis of pits of the optic nerve head involves incomplete closure of the embryonic fissure and represents the mildest variant in the spectrum of optic disc colobomas (1). Clinical evidence, however, including the fact that there are few systemic associations, is inconsistent with this hypothesis (1):
 Optic disc pits are usually unilateral, sporadic, and not associated with systemic anomalies. In contrast, colobomas are bilateral as often as they are unilateral and may be associated with a variety of systemic anomalies.
Optic disc pits are usually unilateral, sporadic, and not associated with systemic anomalies. In contrast, colobomas are bilateral as often as they are unilateral and may be associated with a variety of systemic anomalies.
 More than 50% of optic nerve head pits are located on the temporal aspect of the disc, and one third are at the center of the disc, locations that are unrelated to the embryonic fissure.
More than 50% of optic nerve head pits are located on the temporal aspect of the disc, and one third are at the center of the disc, locations that are unrelated to the embryonic fissure.
On the other hand, congenital optic disc pits sometimes are seen in combination with optic nerve colobomas. Furthermore, one or more cilioretinal arteries emerge from the majority of pits. These observations suggest that congenital pits of the optic nerve head may be pathologically related to colobomas of the optic nerve head, despite uncertainty regarding their respective pathogeneses.
Pathogenesis of Serous Detachment
The pathogenesis and pathologic nature of the associated macular lesions and the origin of subretinal fluid remain controversial.
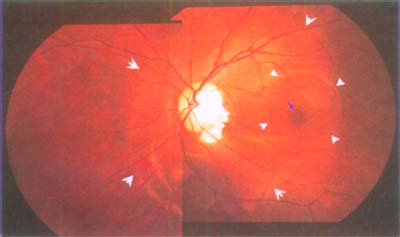
Figure 45-4. Fundus photograph demonstrating an optic disc pit, an inner-layer separation (large arrowheads), an outer-layer macular hold (open arrowhead), and an outer-layer sensory detachment (small arrowheads).
Although evidence in a model using collie dogs suggests that subretinal fluid originates from the vitreous cavity (26), no firm evidence for such a communication in humans has been found (5). There are several reports suggesting the existence of direct communication between the vitreous cavity and subretinal space. Sugar (12) proposed that fluid from the vitreous cavity leaks through the optic nerve head pit to fill the subretinal space (subretinal channel). Bonnet (18) found that none of their patients with macular detachments associated with optic nerve head pits had posterior vitreous detachments, and they observed a small hole in the roof of the pit in several cases. A small bubble of gas was observed to pass from the vitreous cavity into the subretinal space via the optic nerve head pit in a patient who underwent vitrectomy and gas injection without photocoagulation. Thus, Bonnet concluded that macular detachment combined with an optic disc pit has a rhegmatogenous component associated with vitreous traction.
Other possible sources of subretinal fluid in humans include cerebrospinal fluid from the subarachnoid space, leakage from choroidal vessels, leakage from small vessels located at the base of the pit into subretinal space (15), and entrance of fluid from the vitreous cavity through a secondary macular hole (27, 28). Because an increase in vascular permeability is not observed by fluorescein angiography in many cases, most authors agree that the subretinal fluid originates from either the vitreous or cerebrospinal fluid (1) (Fig. 45-3).
Subretinal fluid accumulation resulting from leakage of cerebrospinal fluid through the optic disc pit first was noted by Regenbogen et al. (29). Neither experimental studies nor histopathologic evaluations, however, have demonstrated such a pathway. Intrathecal injections of fluorescein in humans and animals have not shown passage of dye into the subretinal fluid (26, 30). Such a communication was demonstrated, however, by Chang et al. (31) in an eye with a retinal detachment associated with morning glory anomaly. Irvine and associates (32) demonstrated communication between the vitreous cavity and the orbit via a morning glory disc anomaly and the subarachnoid space of the optic nerve. During surgery, gas injected into the vitreous cavity escaped from the eye through a surgical window in the optic nerve sheath.
Regardless of the presumed source of fluid, most authors have assumed that macular detachments were the result of fluid entering directly into the subretinal space at the site of the optic disc pit. Macular edema, cystoid degeneration, and schisis-like changes were considered to be secondary effects from longstanding macular detachment (2). Recent data, however, have suggested the converse. Lincoff and associates (14), using stereoscopic examination of the macula in conjunction with kinetic perimetry, suggested that the macular elevation in the early stage of the disease is a separation of the inner retinal layers to produce a schisis-like splitting of the neurosensory retina, which emanated from the optic disc pit. At a later stage, an outer-layer macular hole and an outer-layer retinal detachment would develop (Fig. 45-4).
Pathology
Peterson (33) reported that marked edema of the temporal lesion from the optic disc, particularly in the outer plexiform layer, was observed histopathologically, although a macular lesion was not identified clinically. Ferry (8) examined histologically two eyes that had been enucleated for the suspected clinical diagnosis of choroidal malignant melanoma. Both eyes had retinal detachments temporal to the optic disc. He showed herniation of dysplastic retina through a defect in the lamina cribrosa into a collagen-lined pocket. The progressive gliosis and “contraction of the retinal elements” contained in the pit may have produced a traction detachment of the macula. There were patchy photoreceptor degeneration, depigmentation of the retinal pigment epithelium, edema, and cystoid degeneration. Gass (2) noted cystic degeneration, partial splitting of the outer plexiform layer in the perifoveal area, and dysplastic tissue encapsulated in a multiloculated space that was separated from the subretinal space by multiple thin septa.
These reports demonstrate varying degrees of edema and cystic changes in the retina adjacent to the optic disc pit with or without retinal detachment. These findings are not contradictory to the concept of a bilaminar macular structure, as proposed by Lincoff et al. (14) or suggested by studies using OCT (10, 11).
Natural Course
The natural course of retinal detachment associated with optic disc pits is variable (1, 17). The patient usually presents with symptoms of blurred vision and metamorphopsia secondary to foveal involvement. Sobol et al. (34) followed 15 eyes with optic nerve head pits and macular detachments for an average of 9 years and found that most patients with optic nerve head pits presented with visual acuities of about 20/40 to 20/60, with each patient losing three or more lines of vision within the next 6 months.
The subretinal fluid may be absorbed and then recur after a prolonged time. Chronic or intermittent macular detachment may be associated with long-term macular changes including full-thickness or outer-layer macular holes, cystic degeneration, retinoschisis with or without an outer-layer macular hole, and retinal pigment epithelial changes that reduce visual acuities (20, 35).
Sobol et al. (34) found that 80% of 15 eyes lost vision to 20/200 or worse at the time of the last evaluation. The visual loss was generally complete within 6 months of presentation. Subretinal fluid absorbed spontaneously in four eyes (27%). Brown and Tasman (5) reported that among 20 untreated eyes followed for at least 1 year, the visual acuity was 20/100 or worse in 55%. The mean visual acuity at the end of the evaluation was about 20/80. They noted that, although some detachments resolved spontaneously, others persisted for years. After 5 years, most patients still had some subretinal fluid present.
Treatment
Multiple treatment options are available for the retinal detachment associated with an optic disc pit. Detachments that do not involve the macula and those that do involve the macula and not the fovea can be observed without intervention. Macular detachments have been reported to resolve spontaneously up to 25% of the time.
If vision is decreased because of serous macular retinal detachment, laser treatment along the edge of the pit has been recommended to induce reattachment of the retina to the underlying retinal pigment epithelium and subsequent resorption of the subretinal fluid (Fig. 45-5). A few reports have documented a favorable response with such treatment, although some cases require multiple sessions (13, 14, 36–38). Laser treatment sometimes is performed with the krypton laser to minimize damage to the inner retinal layers (37). This may be followed by bedrest and bilateral eye patching. The difference in final visual outcome between treated and untreated groups, however, was not pronounced (15). Brown and Tasman (5) concluded that laser therapy is effective for flattening the retinal detachment but not for improving final visual outcome.
In eyes with severe visual loss that do not respond to laser therapy, the possibility of repeat laser treatment in conjunction with either injection of a long-acting gas into the vitreous cavity or pars plana vitrectomy with fluid-gas exchange may be considered (14, 38, 39). Yanyali and Bonnet (40) discussed their therapeutic results in 19 eyes with serous macular detachments associated with optic disc pits. Photocoagulation of the temporal margin of the nerve head was combined with intravitreal gas injection. Eight eyes (42%) required more than one procedure. At last examination, the macula was reattached in 17 (94%) of the 18 eyes with adequate follow-up, and visual acuity improved in 12 eyes (67%). Persistent subretinal fluid not involving the central macula was evident following successful surgery in three (17%) of the 18 patients. In 1995, Brown and Brown (39) described treatment outcomes in four cases in which laser therapy alone did not cure retinal detachments associated with optic disc pits. Pars plana vitrectomy, fluid-gas exchanges, and additional laser treatments were successful in reattaching the retina in all four eyes, although 7 months were required for complete resolution of subretinal fluid in one case.
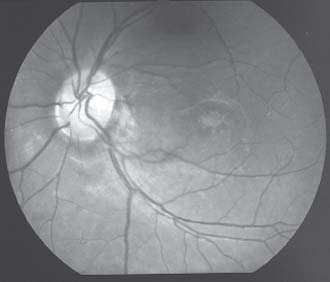
Figure 45-5. Fundus photograph showing photocoagulation scars along the edge of a pit.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


