Congenital and Pediatric Retinal Diseases
Nikolas J.S. London
Richard S. Kaiser
Retinopathy of Prematurity
Retinopathy of prematurity (ROP) is a proliferative retinopathy of premature, low-birth-weight infants.
Epidemiology and Etiology
Despite recent advances, ROP remains a leading cause of visual loss in children. Infants born at less than 30 weeks gestation and/or those with a birth weight of 1500 g or less should be examined by indirect ophthalmoscopy. Infants who are born weighing 1000 g or less are at particularly high risk of developing severe ROP.
The retinal vasculature of infants born prematurely has not completed its growth to the ora serrata. The developing vasculature is susceptible to capillary endothelial cytotoxicity. Pre-existing vessels are damaged and neovascularization develops off the surface of the retina. Continued growth and contraction of fibrovascular tissue may lead to retinal detachment.
History
The critical components of the history are the birth weight, the gestational age at birth, the current postmenstrual age, and the current chronological age. One should also inquire regarding the use of mechanical ventilation and/or supplemental oxygen, the length of stay in the neonatal ICU, blood transfusions, the presence of any bronchodysplasia or hyaline membrane disease. Pregnancy history, maternal health, and family history are also often obtained.
Diagnostic Evaluation
Careful examination of neonates with indirect ophthalmoscopy in the intensive care nursery or at discharge is essential to detect ROP at a stage where treatment can be applied.
Examinations should start at 31 weeks postmenstrual age or by 4 weeks chronological
age, based on gestational age, and should continue every 1 to 3 weeks, until one of the following occurs:
There is vascularization of zone III without prior zone I or II disease.
Postmenstrual age 45 weeks is achieved with no prethreshold ROP.
The retina is completely vascularized.
There is total regression of treated ROP.
Important Clinical Signs
The posterior segment signs of ROP follow a progression of increasing severity that were classified according to the International Classification of ROP (ICROP).
Associated Clinical Signs
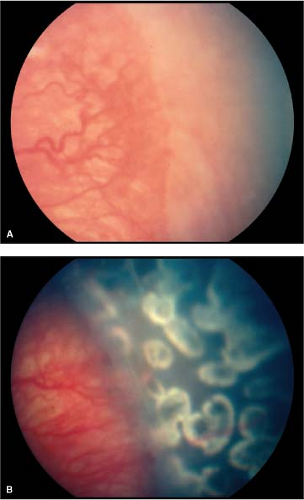
“Plus” disease denotes increased severity. When an eye has dilation and tortuosity of the retinal vessels in the posterior pole, then it is said to have plus disease and has a poorer prognosis (Fig. 7-6). When vascularization is only present in zone I and there is plus disease, then a very poor prognosis exists because of the risk of rapid progression (“rush” disease).
“Threshold” disease is a level of ROP at which it is predicted that there is a 50% chance of progression to retinal detachment without treatment. It was defined in the CRYO-ROP study as 5 contiguous clock hours of extraretinal fibrovascular proliferation (ERFP) with plus disease or 8 accumulated clock hours of ERFP with plus disease (Fig. 7-7). When threshold disease is reached, treatment is recommended. In addition, current guidelines indicate treatment within 72 hours for the following clinical situations:
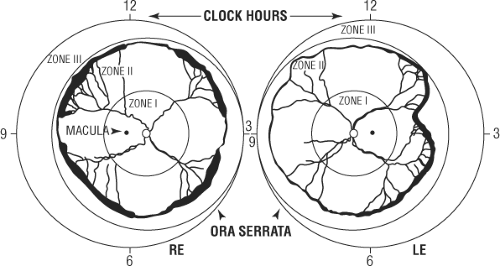
Table 7-1. International Classification of Retinopathy of Prematurity (ICROP)
Location
Zone I
Posterior circle of retina centered on the optic nerve with a radius of twice the disc-fovea distance
Zone II
Circular area of retina from the edge of zone I to the nasal ora serrata
Zone III
Remaining temporal crescent of retina
Extent
Number of clock hours or 30-degree sectors involved
Severity
Stage 1
Demarcation line between posterior vascularized retina and anterior avascular retina
Stage 2
Demarcation line with height, width, and volume (ridge)
Stage 3
Ridge with extraretinal fibrovascular proliferation (ERFP); may be mild, moderate, or severe
Stage 4
Subtotal retinal detachment
4A
Extrafoveal
4B
Involving the fovea
Stage 5
Total retinal detachment; always funnel-shaped
Open anteriorly, open posteriorly
Open anteriorly, narrow posteriorly
Narrow anteriorly, open posteriorly
Narrow anteriorly, narrow posteriorly
Zone I, any stage, with plus disease
Zone I, stage III, with or without plus disease
Zone II, stage II or III, with plus disease
Occasionally neovascular tissue may form buds of vascular proliferation behind the ridge or demarcation line. These lesions are called “popcorn” because of their similarity to popped corn (see Fig. 7-3A). These lesions do not carry any prognostic significance unless they are a part of ERFP at the advancing border of vascularization. Vitreous hemorrhage and preretinal hemorrhage can occasionally be seen in eyes with severe ERFP.
In early cicatricial ROP (after resolution of the acute phase) there may be a variety of tractional complications. A hallmark finding of regressed cicatricial ROP is temporal retinal dragging (Fig. 7-8).
After regression of ROP, either spontaneously or with treatment, several associated abnormalities may occur.
Myopia
Astigmatism
Strabismus
Amblyopia
Cataract
Glaucoma
Macular ectopia
Retinal fold
Retinal detachment—rhegmatogenous or exudative
Differential Diagnosis
The clinical setting usually aids in the diagnosis of ROP. Infants are born prematurely and are of low birth weight with a history of oxygen exposure.
Differential diagnosis depends on the stage of the disease. In less severe ROP, conditions that cause peripheral retinal vascular changes and retinal dragging should be considered.
Familial exudative vitreoretinopathy (FEVR)
Incontinentia pigmenti (Bloch–Sulzberger syndrome)
X-linked retinoschisis
Norrie’s disease
In advanced cicatricial ROP, the differential diagnosis is that of retinal detachment or a white pupillary reflex, or both.
Cataract
FEVR
Persistent fetal vasculature (PFV)
Ocular toxocariasis
Intermediate uveitis
Coats’ disease
Retinoblastoma
Vitreous hemorrhage
Retinal detachment
Endophthalmitis
Prognosis and Management
The majority of infants who develop ROP undergo spontaneous regression (85%). However, 7% of infants weighing less than 1251 g at birth will develop threshold ROP.
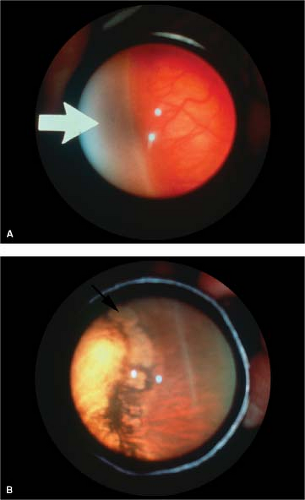
Cryotherapy to the anterior avascular zone (Fig. 7-9) has been shown to reduce the likelihood of an unfavorable outcome (retinal fold through zone I, retinal detachment, or retrolental fibroplasia) by 50% in the cryotherapy for ROP Study. Visual results are commensurately improved.
Laser photocoagulation delivered with an indirect ophthalmoscope to the anterior avascular zone has virtually replaced cryotherapy for threshold ROP (Fig. 7-10). Laser burns should be spaced evenly, approximately one-half burn width apart, with particular attention to the most posterior avascular retina. Better visual outcomes have been achieved with laser treatment.
Antiangiogenic injection therapy for ROP is being investigated, with early reports of success. Bevacizumab eliminates the angiogenic threat of ROP is a randomized trial comparing intravitreal bevacizumab to conventional laser treatment.
More advanced stages of ROP (stages 4 and 5 retinal detachment) can be treated with scleral buckling or vitrectomy, or both. The prognosis for visual recovery after retinal detachment remains poor.
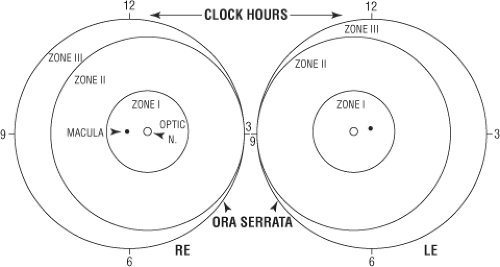 Figure 7-1. Retinopathy of prematurity (ROP). Schematic diagram of division of fundus into zones for defining location of involvement with ROP. |
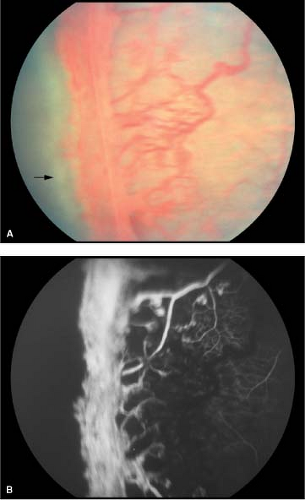
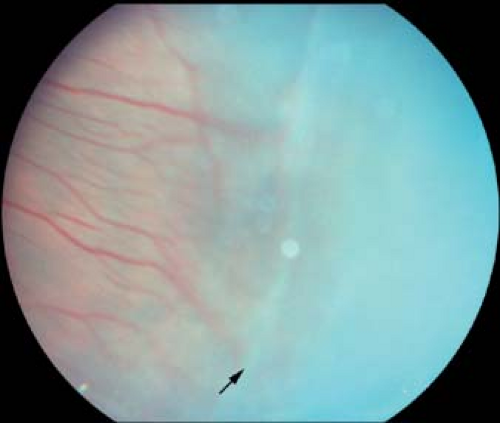 Figure 7-2. ROP, stage 2. The demarcation line (arrow) between posterior vascularized and anterior avascular retina is elevated as a ridge. |
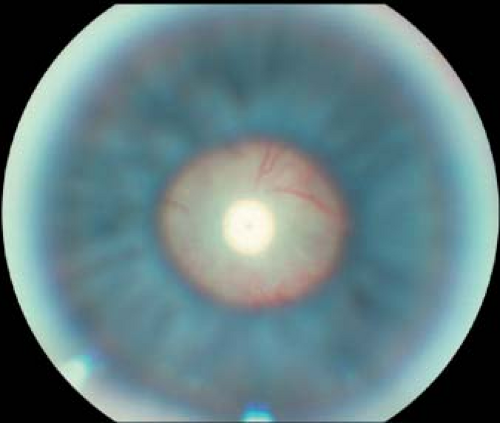
 Figure 7-4. ROP, stage 5. Eye with shallow total retinal detachment. Note loss of choroidal detail due to shallow subretinal fluid accumulation in posterior pole. |
 Figure 7-6. ROP, plus disease. Dilation and tortuosity of vessels in the posterior pole denotes progressive disease and is known as “plus” disease. |
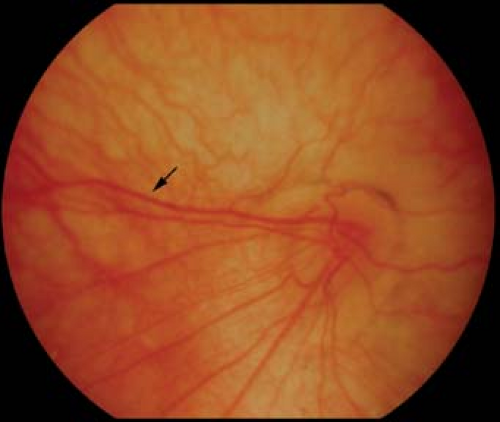 Figure 7-8. ROP. Severe dragging of the temporal retina with vascular straightening (arrow) is a late cicatricial complication of ROP. Compare with familial exudative vitreoretinopathy, in Figure 7-18A. |
Incontinentia Pigmenti
Incontinentia pigmenti, or Bloch–Sulzberger syndrome, is a rare X-linked dominant condition that includes ocular, skin, central nervous system, skeletal, dental, and other systemic abnormalities.
Epidemiology and Etiology
The pathogenesis of incontinentia pigmenti is unknown. It is an X-linked dominant condition that is usually lethal in males and thus usually only seen in female infants. However, an affected male with Klinefelter syndrome (XXY) or a genetic mosaicism may survive.
History
Characteristic skin changes usually start days after birth, with ophthalmic findings developing in infancy or even later in life.
Important Clinical Signs
Approximately one-third of infants with incontinentia pigmenti have ocular findings. Fundus abnormalities include dilated, tortuous retinal vessels, peripheral retinal capillary nonperfusion with arteriovenous anastomoses and neovascularization (Figs. 7-11 and 7-12), foveal hypoplasia, branch artery occlusions, neovascularization of the disc, retinal dragging, tractional and rhegmatogenous retinal detachments, retinal folds, vitreous hemorrhage, and optic disc pallor.
The ocular abnormalities are often extremely asymmetric.
Associated Clinical Signs
Other ocular findings include cataract, conjunctival pigmentation, and strabismus. Skin findings, for which the disease is named, include vesicular skin eruptions (Fig. 7-13) that later turn into depigmented lesions (Fig. 7-14). These changes start days after birth.
Dental abnormalities consisting of missing or cone-shaped teeth are present in approximately two-thirds of affected individuals (Fig. 7-15). Associated central nervous system abnormalities include seizures, spastic paralysis, and mental retardation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree