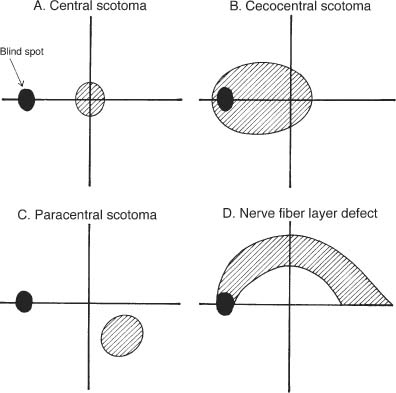
Chapter 22 Masses impinging on the intraorbital or intracranial optic nerves, the optic chiasm, or the optic tracts may cause compressive damage to the anterior visual pathways. The initial evaluation involves confirmation of visual dysfunction, localization of the lesion, and neuroimaging to determine the nature, location, and extent of the compressing lesion.1 Treatment is then directed to the specific etiology. Compressive optic neuropathy is usually a slowly progressive process occurring over many months. Acute and subacute visual loss may occur, however, which requires urgent evaluation. Patients often describe dim or foggy vision with “washed out” color vision. Visual loss generally occurs gradually over months to years in most cases of compressive optic neuropathy. Acute and subacute visual loss is less common, and may occur acutely due to sudden enlargement of the compressive mass such as hemorrhage in pituitary apoplexy,2 an expanding carotid-ophthalmic aneurysm, an enlarging mucocele, or expansion of the cystic component of a craniopharyngioma. Occasionally, subacute visual loss may occur over several days to weeks due to infiltrative optic neuropathies, metastasis, and in malignant optic nerve glioma of adulthood.3 Intraorbital tumors may affect the extraocular muscles or their innervation. Intracranial tumors or orbital tumors with intracranial extension may impinge the ocular motor cranial nerves in the cavernous sinus or superior orbital fissure. Headache or eye pain may occur with both intracranial and orbital processes; however, most cases of orbital compressive optic neuropathy present with painless slowly progressive visual loss.1 Pituitary dysfunction including amenorrhea, galactorrhea, decreased libido, and acromegaly may occur in association with chiasmal involvement. A variety of other symptoms may occur dependent on the location of the lesion. A diminished sense of smell may accompany olfactory grove meningioma. If the compression is associated with a systemic malignancy, weight loss may occur. A variety of other neurologic symptoms can occur with diffuse lesions such as leptomeningeal metastasis. The magnitude of central acuity loss varies with the extent and location of the compressive lesion. Lesions that compress the retrobulbar or intracranial optic nerve cause central, cecocentral, or nerve fiber layer defects associated with varying degrees of central acuity loss and dyschromatopsia.1 Very rarely, small arcuate defects may occur with preservation of central visual function. This is in contrast to chiasmal and optic tract lesions in which central acuity is often maintained. Visual field defects that develop due to compression of the anterior visual pathways are important in the localization of the lesion. Retrobulbar and intracranial optic nerve compression commonly produce central, cecocentral, paracentral, and nerve fiber layer bundle defects (Fig. 22–1). Chiasmal compression produces bitemporal hemianopias and junctional scotomas (Chapter 28), whereas optic tract lesions produce incongruous homonymous hemianopias (Chapter 29). A relative afferent pupillary defect is present with unilateral disease but may be subtle in mild cases or in asymmetric bilateral disease. Bilateral disease producing symmetric impairment may not produce a relative afferent pupillary defect, although both pupils may react sluggishly. Proptosis and/or resistance to retropulsion may be seen with orbital tumors such as a cavernous hemangioma or with thyroid eye disease. Enophthalmos can rarely occur with metastatic scirrhous carcinoma.4 Eyelid abnormalities may be present such as ptosis, with third nerve involvement, and lid lag and lid retraction with thyroid eye disease. Orbital processes may not produce a pattern of extraocular movement abnormalities referable to a cranial nerve. With thyroid disease, restriction in upgaze and lateral gaze is most common due to enlargement and greatest restriction of the inferior and medial rectus muscles. With intracranial or orbital apex lesions, specific oculomotor palsies may occur. The optic disc may appear normal early in the clinical course. Most commonly there are signs of optic atrophy with chronic compression (Fig. 22–2). Bowtie atrophy may be seen with chiasmal or optic tract compression in the eye with a temporal field defect due to loss of the nasal crossing fibers (fibers entering the nasal disc fibers of the papillomacular bundle entering the temporal disc), resulting in a horizontal “bow-tie” region of disc atrophy (Fig. 22–3).5 Optic disc edema may occur with orbital or canalicular compression, but not with intracranial lesions.6 True papilledema (disc edema due to increased intracranial pressure) may rarely occur due to compression of the anterior third ventricle with secondary hydrocephalus by tumors such as craniopharyngioma. Chronic compression primarily from optic nerve sheath meningiomas and rarely optic nerve glioma may cause impaired venous outflow yielding optociliary shunt vessels on the surface of the optic disc (Fig. 22–4 and Fig. 22–5).7 Patients with slowly progressive visual decline and typical findings of unilateral or bilateral optic neuropathy should be assumed to have a compressive etiology until proven otherwise and require neuroimaging. The following features should raise the question of alternative diagnosis: FIGURE 22–1
COMPRESSIVE OPTIC NEUROPATHY
URGENCY OF EVALUATION
DIAGNOSIS
SYMPTOMS
Visual Loss
Diplopia
Pain
Pituitary Dysfunction
Other Symptoms
SIGNS
Visual Acuity
Visual Field
Pupils
Orbital and Eyelid Signs
Extraocular Movement Abnormalities
Optic Disc
Red Flags
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree