54
Complications of Photocoagulation
María H. Berrocal  Virgilio Morales-Canton
Virgilio Morales-Canton
Photocoagulation of the retina has undergone significant advances and refinements since its initial application by Gerd Meyer-Schwikeratz in 1949 (1). Xenon arc light coagulators and ruby lasers have been replaced by argon, krypton, dye, and diode lasers. The new lasers allow for smaller, multiple, more precise burns and diverse delivery systems. Treatment can be applied through a slit lamp, indirect ophthalmoscope, intravitreally during vitrectomy surgery, and transsclerally. The diversity in modality and delivery options has expanded the potential applications for laser therapy. Photocoagulation is a minimally invasive treatment modality; nevertheless, complications are possible and diverse relative to the procedure employed.
GENERAL COMPLICATIONS
General complications of photocoagulation include incorrect focusing and improper intensity and size of the laser burns. Focusing problems can cause inadvertent photocoagulation of the iris, cornea or crystalline lens which can result in synechiae formation, corneal and lens opacities. Lens opacities are more common when blue-green argon is used in eyes with nuclear sclerosis lens opacities, but has also been described with krypton (2–4). Corneal epithelial abrasions can occur from the contact lens used in the treatment. These are more frequent with prolonged treatments in diabetic eyes. In the posterior segment misplaced laser spots can result in inadvertent foveal or optic nerve burns and may cause scotomas, decreased vision, and visual field defects. Focusing complications can be avoided by meticulous technique, foveal localization, and adequate patient cooperation. The use of a projected fluorescein angiogram during treatment can aid in avoiding foveal burns. In uncooperative patients, particularly when applying treatment in the macular area, akinesia by retrobulbar or subtenons injection may be necessary.
Very intense burns can rupture retinal vessels and Bruch’s membrane causing bleeding and potentially choroidal neovascular membranes and fibrovascular ingrowth. Bleeding is treated by applying pressure with the contact lens and photocoagulating the area with a larger spot size. A ruptured Bruch’s membrane can be readily apparent but can be inadvertent and occur without any bleeding or obvious sign (5, 6). This complication is more common when using small spot sizes and lasers with longer wavelengths (i.e., krypton and diode), but has also been described with argon (7, 8). Applying faint, light gray burns and avoiding small spot sizes can help reduce this complication. Special caution should be used when treating highly myopic or amelanotic fundi. The lack of pigment causes reduced uptake by the retinal pigment epithelium (RPE) and higher laser powers are often needed. These eyes have a propensity for bleeding during treatment.
Vessel occlusions can occur and are more frequent when more intense and confluent treatment is necessary, as when treating tumors or subretinal neovascular membranes (SRNVMs). Very intense burns can also cause breaks in the retina, expand over time, and cause thermal contraction with retinal traction. Enlargement of laser scars can occur over time with all laser modalities. Severe RPE and choriocapillaris damage has been reported with transpupillary thermotherapy (TTT) and during photodynamic therapy.
MACULAR EDEMA
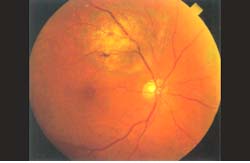
Treatment for diabetic macular edema and macular edema secondary to vein occlusions can be challenging, particularly since the foveal reflex is often obscured by edema, blood, or exudates. Identifying the patient’s fixation point is important to avoid foveal burns. Complications of focal and grid treatment include foveal burns (Fig. 54-1), scotomas, enlargement of burns over time, increased foveal ischemia, foveal migration and precipitation of hard exudate, increased macular edema, subretinal fibrosis, SRNVMs, premacular fibrosis, traction retinal detachment, and loss of central light sensitivity. Foveal burns can be avoided by finding the fixation point, projecting a fluorescein angiogram and using akinesia when cooperation is poor. Scotomas are best avoided by not treating near the foveal avascular zone (FAZ), using low energy, and avoiding the use of blue-green wavelength (9). Enlargement of burns over time can cause scotomas. This is more common in myopic eyes and a 5% incidence has been described with krypton grid (10). Precipitation of hard exudates, foveal migration, and subretinal fibrosis can occur in eyes with severe, chronic edema and with aggressive treatment (11). In these instances, treatment in multiple sessions is advised to allow gradual fluid resolution. Increase in macular edema can occur with aggressive treatment and concomitant panretinal photocoagulation (PRP). Treatment of the macular edema prior to PRP reduces this risk. Development of SRNVMs is a complication due to damage or breaks in Bruch’s membrane. Avoiding very small, intense, and short duration burns reduces this severe complication which carries a poor prognosis (5, 8). Thermal contraction of the retinal surface and premacular fibrosis can cause traction of the fovea and traction retinal detachment. This is best prevented by avoiding intense burns, treating over blood, and blue-green wavelength. Caution should be used when treating eyes with enlarged FAZ’s since treatment can compromise the existing capillaries leading to more ischemia. General recommendations to avoid complications include identifying the fixation point, treating with light burns in multiple sessions, and avoiding treating directly over blood or fibrovascular tissue.

Figure 54-1. Foveal burns.
IDIOPATHIC CENTRAL SEROUS CHOROIDOPATHY
Complications of the treatment of idiopathic central serous choroidopathy are similar to those of focal treatment and include scotomas, retinal wrinkling, metamorphopsia, subretinal hemorrhage, SRNVMs, and decreased visual acuity (12).
AGE-RELATED MACULAR DEGENERATION
In the treatment of age-related macular degeneration, laser has been used to treat drusen, SRNVMs, and pigment epithelial detachments (PED). Laser treatment of drusen can cause scotomas and SRNVMs (13). The benefit of this treatment has not been established. Complications of the treatment for SRNVMs are incomplete coverage of lesion, extension of treatment to the fovea, progression of disease in 50% of cases, subretinal fibrosis, retinal vessel occlusions, subretinal and vitreous hemorrhage, nerve fiber bundle defects, and enlargement of the burns over time (Fig. 54-2). The use of an enlarged fluorescein angiogram to guide treatment and correlating lesion size with post treatment scar by drawings can help ensure adequate treatment of the subretinal membrane margins. Careful foveal identification and patient cooperation are important in avoiding inadvertent foveal treatment. Foveal traction, subretinal fibrosis, and retinal vessel occlusions can occur with intensive treatment and when large membranes are treated. Retinal vessel occlusions may be reduced with the use of krypton (14). Hemorrhage can occur from the retinal vessels, the SRNVM, or the choroid. Avoiding small spot sizes and short exposure times may help reduce this complication.
Nerve fiber layer (NFL) damage is more common with treatment of juxtapapillary membranes and with short wavelength lasers. Enlargement of the burn size over time is more often seen in myopic eyes. Myopes can also experience expansion of lacquer cracks after photocoagulation (15). Large PED’s pose a special treatment problem since laser treatment can cause RPE rips with significant visual reduction. These rips can also occur spontaneously.
PANRETINAL PHOTOCOAGULATION
Treatment of proliferative diabetic retinopathy by PRP significantly reduces the risk of severe visual loss. Nevertheless, PRP has significant potential complications. Transient complications include choroidal and exudative retinal detachment (Fig. 54-3), angle shallowing, increased intraocular pressure, and macular edema (4, 16, 17). These complications are more common when extensive treatment is done in one session. The mechanism is possibly damaging to the RPE and choriocapillaris (18, 19). The incidence of some degree of cilioretinal effusion after PRP is between 59% and 90% and is increased with the number of applications, short axial length eyes, and percentage of area of retina treated (20, 21). These complications generally resolve within 14 days.
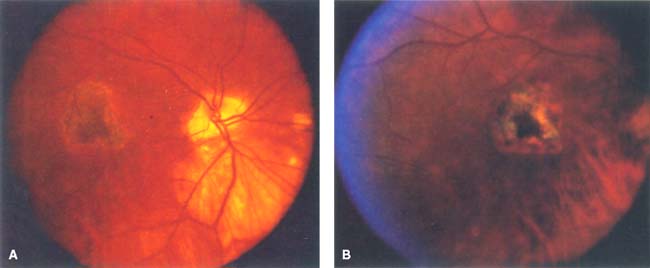
Figure 54-2. A: Laser photocoagulation scar in a myopic eye treated for a subretinal neovascular membrane. B: Laser scar 1 year after treatment. The scar has increased in size.
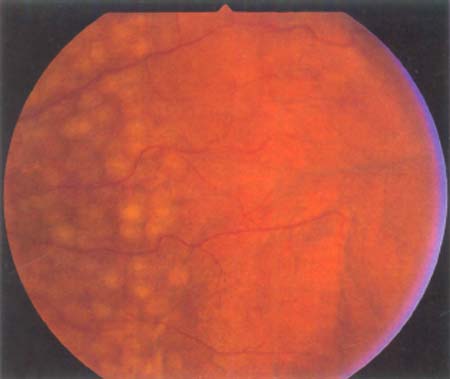
Figure 54-3. Choroidal detachment after panretinal photocoagulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


