Cochlear Implantation and Implantable Hearing Aids
Joseph B. Nadol, Jr.
Since early attempts at experimental electrical stimulation of the auditory nerve in deaf patients (1, 2, 3), there have been rapid advances in electrode and processing technology, and three implant systems (Nucleus, Clarion, and Med-El) have been approved by the Food and Drug Administration (FDA) for rehabilitation of individuals with severe to profound sensorineural hearing loss in both ears.
Study of temporal bones from individuals profoundly deaf during life (4) has demonstrated that despite great variability, the mean number of remaining spiral ganglion cells ranges from 28% to 75% of normal, suggesting that an “adequate” number of ganglion cells is available for stimulation in most patients with profound deafness. The most significant determinant of the number of remaining spiral ganglion cells appears to be the cause of deafness. Thus individuals who are deafened by aminoglycoside toxicity generally have a higher individual cell count than those who became deafened from postnatal viral or bacterial labyrinthitis. However, the minimum requisite number of functioning spiral ganglion cells and their optimal distribution within the cochlea are as yet undetermined. Nevertheless, cochlear implantation is a rehabilitative option in the majority of both prelingually and postlingually deafened individuals. Because of the tonotopic arrangement of receptor units within the organ of Corti and the low electrical impedance encountered in the scala tympani, contemporary electrode arrays are designed to be placed into the scala tympani via the round window.
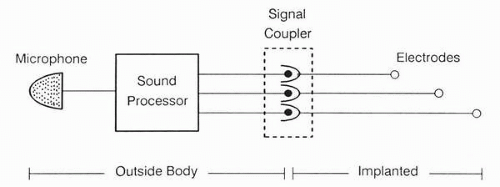
Despite a variety of electrode arrays and strategies for speech processing, all cochlear implants have several elements in common (Fig. 27.1). A microphone, usually at ear level, detects acoustic energy, which is then encoded into an electrical signal by the external sound processor. The electrical stimulus is then transmitted to the implanted electrode array either in the middle ear or inner ear through some form of signal coupler. This may take the form of a direct (percutaneous) or induction-coupled (transcutaneous) system. The most commonly used commercially available implants in the United States are those manufactured by Clarion (Advanced Bionics Corporation) with eight pairs of electrodes and by Nucleus (Cochlear Corporation) with 22 or 24 active electrodes. Both systems employ a transcutaneous signal coupler. The most important difference between sound processors is the use of single-channel versus multichannel strategies. A single-channel processor presents the same information to one or more electrodes, whereas in a multichannel processor each of the implanted electrodes receives a different stimulus based on its position within the cochlea. Both the Clarion and Nucleus devices are multichannel systems capable of a variety of processing strategies.
PREOPERATIVE EVALUATION AND PATIENT SELECTION
At present, cochlear implantation has clinical approval of the FDA for both prelingually and postlingually deafened children and adults.
Clinical Evaluation and Criteria
The first stage of evaluation includes an otologic and audiologic history and examination. Particularly for prelingually deafened individuals, the current preferred form of communication (oral or sign) will be important for evaluating candidacy for implantation. An evaluation of the daily social interaction of the candidate is important to assess the importance and motivation for oral communication. An audiologist, rehabilitation audiologist, and speech language pathologist will be valuable colleagues in this evaluation.
Clinical Auditory Testing and Criteria
All patients should receive a thorough behavioral audiometric examination including pure-tone thresholds and speech discrimination and, if necessary, confirmation by auditory
evoked response techniques. In the last several years, the threshold for candidacy for implantation based on audiometric results has been somewhat liberalized to include some patients with severe, as well as profound, sensorineural hearing loss. Individuals with a pure-tone average of greater than 80 dB in the better hearing ear and less than 30% open set speech recognition using sentence materials with the best fitting hearing aids are considered candidates for implantation (5).
evoked response techniques. In the last several years, the threshold for candidacy for implantation based on audiometric results has been somewhat liberalized to include some patients with severe, as well as profound, sensorineural hearing loss. Individuals with a pure-tone average of greater than 80 dB in the better hearing ear and less than 30% open set speech recognition using sentence materials with the best fitting hearing aids are considered candidates for implantation (5).
Radiologic Evaluation
Computed tomographic (CT) scanning of the temporal bone is useful for several purposes: (i) to determine the pneumatization of the mastoid; (ii) to evaluate the patency of the inner ear—that is, lack of labyrinthitis ossificans; and (iii) to evaluate the possibility of anomalies of the inner ear (6). Obliteration of part or all of the inner ear by new bone formation may occur in certain forms of deafness, particularly that due to bacterial meningitis (7) (Fig. 27.2), and may be detected by CT (8, 9, 10) (Fig. 27.3). CT may also be helpful in evaluating patients following cochlear implantation (8). Magnetic resonance imaging (MRI) may also be helpful in evaluating lesions of the inner ear (11).
Psychosocial and Educational Evaluation
Assessment of a patient’s motivation for implantation and its subsequent use and the potential effects of surgical success or failure on the patient and his or her family is important. For children, educational plans that include the cochlear implant must be formulated by educators, rehabilitative audiologists, and parents before cochlear implantation.
Informed Consent
In addition to the risks inherent in a mastoidotomy, the patient should be informed of the risks related to the cochlear implant. These include immediate or delayed mechanical or electric failure, infection, or extrusion of the implanted device. Most importantly, the patient should understand that any residual hearing in the operated ear will be lost following insertion of a multielectrode implant and that the hearing results achieved postoperatively are variable and may not include open set speech comprehension without lip reading. Postoperatively, there may be limitations on the ability to undergo an MRI because postoperative exposure to an MR scan may demagnetize the coupling magnet. Even with a removable magnet as available in the Nucleus device, the implanted electronics may be damaged if the power of the MRI exceeds 1.5 tesla. Hence, postoperative MR scanning is at least relatively contraindicated. Given the hearing status of the patient, a preprinted consent form is useful to ensure comprehension of these important issues.
SURGICAL PROCEDURE
The most commonly used surgical approach for cochlear implantation is the postauricular mastoidotomy and posterior tympanotomy for implantation of the scala tympani via the round window.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree