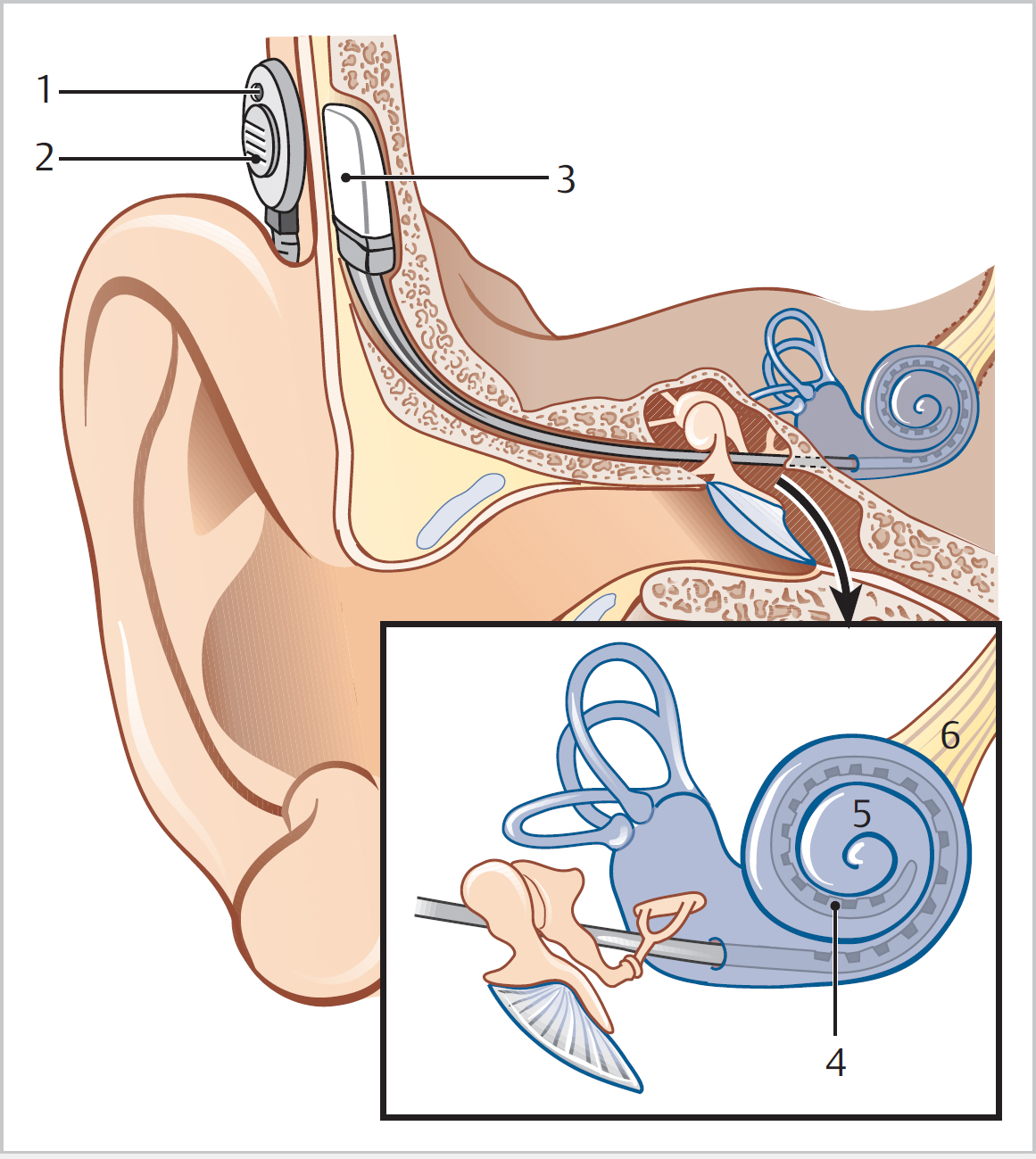
16 Cochlear Implantation • A CI is a device implanted into the cochlea that directly stimulates nerve fibres within the auditory system, allowing the perception of sound (Fig. 16.1) • Paediatric: children with pre-lingual deafness have a critical period in which they can be usefully implanted (<2 years) for greatest benefit; those children (or adults) who lost hearing after language acquisition have established central auditory pathways so can be implanted up to 10 years after the onset of deafness: • Adult >18 years: • Audiometric: • Medical: • Procedure: • Device: • Does not provide normal hearing • Gradual improvement in performance especially in first 6 months, but for up to 2 years • 95% adults have improved lip-reading, 50% have acquired open-set speech discrimination, 35% can use telephone • 90% children aided <2 years enter mainstream education • Reliability: 97 to 99% functioning at 10 years • Which ear? • Bimodal stimulation; HA one ear, CI in the other • Bilateral CIs • Hybrid implants, “electroacoustic stimulation”
16.1 Principles
 Stimulates cochlear n fibres (spiral ganglion cells) with acoustic sounds that have been processed into electrical energy
Stimulates cochlear n fibres (spiral ganglion cells) with acoustic sounds that have been processed into electrical energy
 Primary aim is to provide user with greater speech recognition ability than is possible with conventional amplification
Primary aim is to provide user with greater speech recognition ability than is possible with conventional amplification
 Microphone (worn like an HA) converts sound into electrical signals; speech processor analyzes and digitizes this information into coded signals (splitting into frequency bands); transmitter is held over receiver by a magnet and sends the code across the skin as radiofrequency waves; coded signal is converted to electrical signals that pass to the electrode to allow for stimulation of the nerve fibres (tonotopic arrangement)
Microphone (worn like an HA) converts sound into electrical signals; speech processor analyzes and digitizes this information into coded signals (splitting into frequency bands); transmitter is held over receiver by a magnet and sends the code across the skin as radiofrequency waves; coded signal is converted to electrical signals that pass to the electrode to allow for stimulation of the nerve fibres (tonotopic arrangement)
 Goal in children: to achieve age-appropriate speech, language, and listening skills; to reduce intervention over time; to have mainstream education; to be fully integrated into hearing world
Goal in children: to achieve age-appropriate speech, language, and listening skills; to reduce intervention over time; to have mainstream education; to be fully integrated into hearing world
 Goal in adults: to support lip-reading; to improve communication ability and develop telephone and open-set speech; to reduce effort of communication; to be in touch with surroundings
Goal in adults: to support lip-reading; to improve communication ability and develop telephone and open-set speech; to reduce effort of communication; to be in touch with surroundings
16.2 Indications
 Profound sensorineural hearing loss in both ears (e.g., unaided >90 dB across speech frequencies)
Profound sensorineural hearing loss in both ears (e.g., unaided >90 dB across speech frequencies)
 Lack of progress in the development of auditory skills
Lack of progress in the development of auditory skills
 No medical contraindications
No medical contraindications
 High motivation and appropriate expectations from family
High motivation and appropriate expectations from family
 Precise audiometric inclusion criteria vary from centre to centre and as experience in CI grows
Precise audiometric inclusion criteria vary from centre to centre and as experience in CI grows
 Assess speech, language, and listening skills appropriate for age, developmental stage, and cognitive ability
Assess speech, language, and listening skills appropriate for age, developmental stage, and cognitive ability
 Pre-linguistic or post-linguistic onset of severe-to-profound hearing loss
Pre-linguistic or post-linguistic onset of severe-to-profound hearing loss
 Audiometric criteria and exact test used to make assessment vary between centres
Audiometric criteria and exact test used to make assessment vary between centres
 Consider when hearing worse than 90 dB HL at 2 and 4 Hz; adequate benefit from a conventional HA considered when >50% score on BKB (Bamford-Kowal-Bench) sentence testing at sound intensity of 70 dB SPL, so needs to be worse to justify CI
Consider when hearing worse than 90 dB HL at 2 and 4 Hz; adequate benefit from a conventional HA considered when >50% score on BKB (Bamford-Kowal-Bench) sentence testing at sound intensity of 70 dB SPL, so needs to be worse to justify CI
 No medical contraindications
No medical contraindications
 A desire to be part of the hearing world
A desire to be part of the hearing world
16.3 Contraindications
 Presence of significant residual hearing
Presence of significant residual hearing
 Active infection (acute or chronic OM)
Active infection (acute or chronic OM)
 Ossified cochlea
Ossified cochlea
 Cochlea non-development
Cochlea non-development
 Unrealistic expectations
Unrealistic expectations
16.4 Surgery
 General anaesthesia, mastoidectomy with posterior tympanotomy
General anaesthesia, mastoidectomy with posterior tympanotomy
 Cochleostomy anteroinferior to round window membrane
Cochleostomy anteroinferior to round window membrane
 Multi-channel electrodes generally used, with variable number of specific electrodes depending upon device used
Multi-channel electrodes generally used, with variable number of specific electrodes depending upon device used
 Intra-operative testing with neural response telemetry, checks that implant is working and in contact with auditory n endings
Intra-operative testing with neural response telemetry, checks that implant is working and in contact with auditory n endings
 Post-operative switch-on usually after ~4 to 6 weeks with continued “remapping” over next few years
Post-operative switch-on usually after ~4 to 6 weeks with continued “remapping” over next few years
 Facial paresis/paralysis (temporary or permanent): 1:500 to 1:1000
Facial paresis/paralysis (temporary or permanent): 1:500 to 1:1000
 Taste disturbance (temporary): 10%
Taste disturbance (temporary): 10%
 Loss of residual hearing: dependent on surgical technique and implant used
Loss of residual hearing: dependent on surgical technique and implant used
 Balance dysfunction/vertigo—temporary: most patients; long-term balance dysfunction rare
Balance dysfunction/vertigo—temporary: most patients; long-term balance dysfunction rare
 Infection: <1% but may/usually necessitate removal of implant
Infection: <1% but may/usually necessitate removal of implant
 Meningitis—perioperative: 1:5000 (vaccinate vs. pneumoncoccus, Hib); long-term risk similar to general population
Meningitis—perioperative: 1:5000 (vaccinate vs. pneumoncoccus, Hib); long-term risk similar to general population
16.5 Expected Outcomes
16.6 Special Considerations
 Better-hearing or worse-hearing ear, depending if plan for bimodal stimulation
Better-hearing or worse-hearing ear, depending if plan for bimodal stimulation
 HA use in implanted ear usually predictive of better performance than non-aided ear
HA use in implanted ear usually predictive of better performance than non-aided ear
 Vestibular function
Vestibular function
 Helps in background noise, for sound localization, and allows for better music appreciation
Helps in background noise, for sound localization, and allows for better music appreciation
 Improved sound localization, speech understanding in quiet and noise
Improved sound localization, speech understanding in quiet and noise
 Guaranteed to implant better ear
Guaranteed to implant better ear
 Improved speech, language, and auditory development in children
Improved speech, language, and auditory development in children
 If one fails, not completely isolated
If one fails, not completely isolated
 Simultaneous bilateral CI recommended in adults and children, especially when codisability (e.g., blindness)
Simultaneous bilateral CI recommended in adults and children, especially when codisability (e.g., blindness)
 Shorter electrodes used for high tone loss with conventional HA for lower frequencies
Shorter electrodes used for high tone loss with conventional HA for lower frequencies
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree