Fig. 10.1
CLASS OT-135 system (“IOPtiMate”; IOPtima Ltd., Ramat Gan, Israel) consists of a Beam Manipulator System conjugated with a CO2 laser
CLASS: Surgical Procedure
The procedure is performed under sub-conjunctival anesthesia with 2 % lidocaine without epinephrine. The perilimbal conjunctiva and Tenon’s capsule are dissected. A half-thickness 5 × 4 mm superior scleral flap is fashioned with a crescent knife. A red laser (HeNe) aiming beam is used to mark the scanning area boundaries, with four clear red dots at the corners. Scan dimensions (width and length) can be changed within the range of 1–4 mm. Initially a wide scan area is used to repeatedly remove layers of sclera until a percolation zone can be readily identified. The CO2 laser is repeatedly applied with time intervals of 2–3 s between applications to allow percolation to take place and be detected until sufficient percolation zone of at least 3 mm in region length is clearly evident. The scleral flap is then repositioned and sutured with 10-0 nylon sutures. Figure 10.2 demonstrates the CLASS steps.
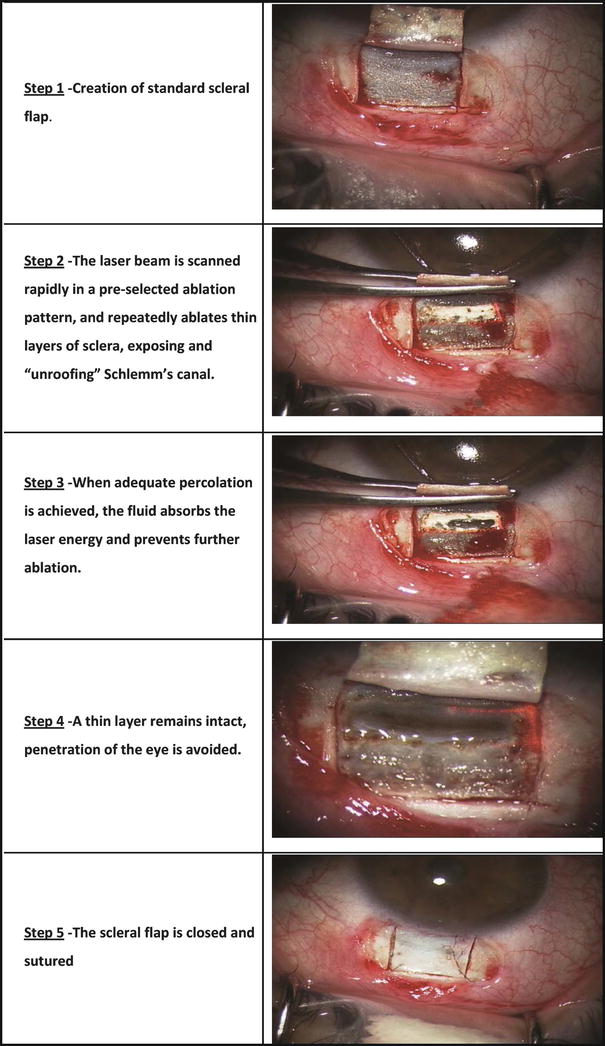
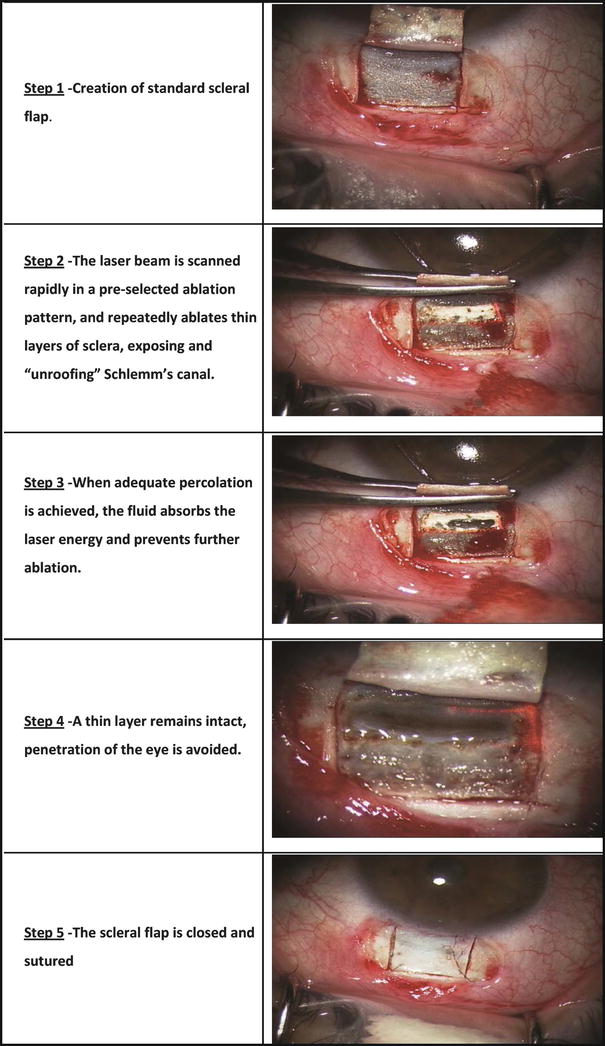
Fig. 10.2
CLASS – surgical procedure steps
Preclinical and Clinical Studies
The preclinical studies (which took place at Goldschleger Eye Research Institute, Sheba Medical Center, Israel; at the Laboratory for Intraocular Microsurgery and Implants, Meir Medical Center, Kfar Saba, Israel; and at the Center for Research on Ocular Therapeutics and Biodevices, Storm Eye Institute, Medical University of South Carolina, USA) were performed on varied experimental models [25]: enucleated pig eyes, live rabbit eyes, and human cadaver eyes. Scleral ablation and aqueous percolation were repeatedly achieved in all models. Histology in each case demonstrated deep scleral craters with thin intact sclera-corneal tissue layer at the ablation area (Fig. 10.3), while the neighboring structures (including sclera, cornea, iris base, and ciliary body) remained undamaged. The results of these experiments indicated that CLASS is a safe and effective procedure for achieving effective fluid percolation.
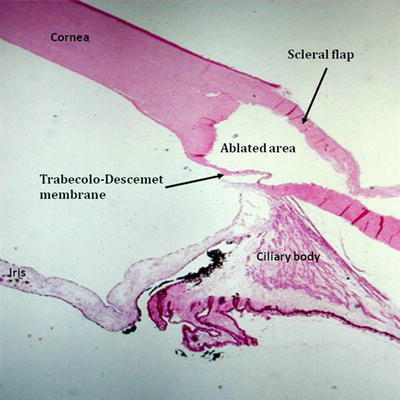
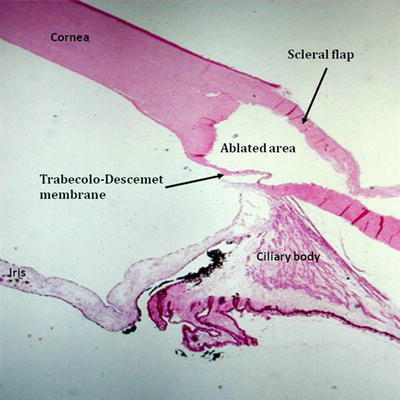
Fig. 10.3
Histological section of a human cadaver eye after CLASS. A half depth scleral flap covers a residual thin intact layer overlying the trabecular meshwork and peripheral Descemet’s membrane
Most of the experiments used prior models of the system (OT-133 and OT-134 “IOPtiMate”; IOPtima Ltd., Ramat Gan, Israel) which were involved with several drawbacks, such as an excessive charring and a tissue coagulation around the treated area, which cause early fibrosis, adhesions, and surgery failure, as reported previously in sporadic cases [24, 25]. Based on the lessons learned, an improved Beam Manipulator System version (OT-135) (Fig. 10.1) was developed using a higher power laser with the ability to diminish localized heating and tissue photocoagulation, increase the control on the ablation process, and minimize the adverse effects to neighbor tissues.
The preclinical experiments have led the way to multicenter clinical trials to come.
Up to now, the technology was clinically tested in several multicenter and multinational studies. Some have already been published in peer-reviewed literature [26, 27].
Studies were done in nine sites: Israel, Tel Hashomer (Prof. Melamed and Dr. Skaat); Israel, Kfar Saba (Prof. Assia and Dr. Geffen); Mexico, Mexico City (Dr. Gil); India, Madanapalle (Dr. Naveen); Russia, Moscow (Dr. Anisimova); Italy, Ancona (Dr. Mariotti); Spain, Valencia (Dr. Muñoz); Swiss, Genève (Dr. Shaarawy); and Swiss, Lausanne (Dr. Mermoud).
A total number of 111 patients with either primary open-angle glaucoma (POAG) or exfoliative glaucoma (PEXG) who were candidates for primary glaucoma filtration surgery were included in the studies. Inclusion and exclusion criteria are shown in Table 10.1. Demographic data is shown in Table 10.2. Comprehensive ophthalmologic examination was performed before and at intervals of 1 day, 1 week, and 1, 3, 6, 12, and 24 months after the surgical procedure. The examination included assessment of best-corrected visual acuity, IOP measurement using Goldmann applanation tonometry (average of three repeated measurements taken at the same time of the day ±1 h), slit-lamp examination, optic disc evaluation, and posterior pole examination. Patients also underwent gonioscopy and assessment of central corneal thickness (average of three repeated measurements). Intraoperative and postoperative complications were documented. The incidence of intraoperative macro-perforations, defined as perforations accompanied by iris prolapse or anterior chamber swallowing or both, was also recorded.
Table 10.1
CLASS studies inclusion and exclusion criteria
Inclusion criteria |
1. Patient age 18 years or older |
2. Patient must have primary open-angle glaucoma or pseudoexfoliative glaucoma in the study eye; diagnosis is based on glaucomatous optic neuropathy, Shaffer angle of +2, and visual field defect attributed to glaucoma (at least two consecutive abnormal visual field test results, defined as a pattern SD (PSD) outside the 95 % normal confidence limits and/or glaucoma Hemifield Test (Carl Zeiss Meditec, Inc.)) |
3. Treated eye must be phakic or pseudophakic eye with no ocular disorder or ocular diseases but cataract and no prior surgical intervention in study eye but cataract surgery with clear corneal incision and trabeculoplasty performed >3 months ago |
4. Patient is indicated for filtration surgery |
5. Presence of ocular hypertension, defined as an intraocular corrected pressure (IOP) ≥21 mmHg in the study eye while on maximal tolerated medications.a This IOP level of above or equal 21 mmHg must be verified and recorded in the most recent two consecutive measurements (but not taken on the same day) prior to operation |
6. Best-corrected visual acuity (BCVA) better than 20/200 in the fellow eye |
7. Optic neuropathy is attributed exclusively to glaucoma |
aPatients on maximal tolerated medications refer to those patients who cannot or will not use medications due to cost issues, memory problems, difficulty of instillation, or inability to tolerate medications |
Exclusion criteria |
1. Diagnosis of glaucoma other than primary open-angle glaucoma or pseudoexfoliative glaucoma |
2. History of previous intraocular surgery in the study eye, referring to but not limited to glaucoma filtering surgery (penetrating and non-penetrating), laser gonioplasty, corneal transplant, and history of any other laser ocular procedures except for laser trabeculoplasty surgery |
3. Laser trabeculoplasty surgery within the last 3 months in the study eye |
4. Study eye is aphakic |
5. Patients with previous cataract extraction with scleral tunnel and or conjunctival incision in the study eye |
6. Proliferative or severe nonproliferative retinopathy in either eye |
7. Eyes with (dilated) pupil diameter of less than 2 mm in the study eye |
8. Discernable congenital anomaly of the anterior chamber angle in the study eye |
9. Patients with neuropathy other than glaucoma in the study eye |
10. Patient with RVO (retinal vein occlusion) or RAO (retinal artery occlusion) in the study eye |
11. History of prior vitrectomy or vitreous hemorrhage (VH) in the study eye |
12. Patient with media opacification which may interfere with optic nerve evaluation in the study eye |
13. Patient with ocular malformations such as microphthalmia in the study eye |
14. Patient with concurrent inflammatory/infective eye disorder (e.g., episcleritis, scleritis) in the study eye |
15. Patient with any sign of past or present uveitis (anterior/posterior) |
16. Patient with known allergy to the study medications |
17. Patient with severe systemic disease or disabling conditions such as chronic renal failure requiring dialysis, severe and disenabling neurological disease, and post organ transplants |
18. Patient participating in another clinical trial or participation in another clinical trial is <3 months |
19. Patient is pregnant or breastfeeding |
Table 10.2
Demographic data of CLASS group
n
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| ||
|---|---|---|