13 Clinical Management of Nonfunctioning Pituitary Adenomas
In the past, nonfunctioning pituitary adenomas were known as chromophobe adenomas based on characteristic results observed with standard hematoxylin and eosin staining. Subsequent refinements in immunohistochemical methods have demonstrated their relative heterogeneity. Clinically nonfunctioning adenomas (NFAs) include null-cell adenomas as well as silent adenomas with positive immunochemical staining. The clinical management of these tumors is discussed in this chapter.
 Epidemiology of Nonfunctioning Adenomas
Epidemiology of Nonfunctioning Adenomas
Pituitary adenomas have been reported to occur incidentally in up to 25% of the population, according to autopsy studies of the sellar region.1 One study of more than 12,000 pituitary specimens demonstrated an 11.3% incidence of adenomas, with the vast majority being microadenomas.2 A recent meta-analysis reported an estimated prevalence of pituitary adenomas in 16.4% of the population.3 NFAs are the most commonly encountered form of pituitary adenomas. According to previous reports, NFAs constitute 25 to 33% of surgically resected pituitary adenomas, making them the most common subtype requiring surgical intervention.4–6
Although NFAs have been labeled nonsecreting tumors (i.e., characterized by no functional oversecretion) in the past, they frequently do produce various hormonal glycoprotein subunits that have little known independent functional endocrine activity.7 On routine immunohistochemical testing, the majority of NFAs stain positive for at least one type of hormone, with gonadotropins being the most commonly produced.7,8 Other immunopositive subtypes of NFAs that are clinically “silent” include corticotroph and somatotroph adenomas.9 True null-cell adenomas are much rarer, representing approximately 6% of all NFAs.1–9 Furthermore, immunohistochemical staining for subunits, such as the α-and β-subunits, is positive in almost 70% of cases.7 Despite the ability to produce glycoprotein hormones and subunits in a majority of NFAs, the ability to secrete these proteins is significantly impaired, occurring in a minority of NFAs.10,11
 Clinical Manifestations of Nonfunctioning Adenomas
Clinical Manifestations of Nonfunctioning Adenomas
Rather than causing symptoms related to hormone oversecretion, as occurs with functional pituitary adenomas, NFAs typically present secondary to mass effect on surrounding structures. Although patients with NFAs frequently present with headaches and visual deficits, serum laboratory studies reveal hypopituitarism in a significant proportion of patients.12,13 In many cases, visual loss occurs secondary to mass effect on the optic chiasm from below, resulting initially in a superior bitemporal quadrantanopsia that frequently progresses to a classic bitemporal hemianopsia.14 The most frequent hormonal abnormalities associated with NFAs are hypogonadism and hyperprolactinemia, followed by growth hormone (GH) deficiency.12 The serum prolactin level is often elevated in patients with NFAs secondary to a “stalk effect,” which prevents the tonic inhibition of prolactinsecreting cells in the anterior pituitary gland via dopamine secretion from hypothalamic cells. Serum prolactin levels in patients with nonfunctioning macroadenomas are typically less than 150 ng/mL, as compared with a maximum value in the several hundred or even thousand range for equally sized prolactinomas.15,16
There is typically a gradual progression in symptoms in patients with NFAs, except in cases of pituitary apoplexy, where acute progression of symptoms is observed in many cases. The diagnosis of pituitary apoplexy is primarily a clinical diagnosis and has been reported in 1 to 21% of patients with NFAs, although the majority of series report an incidence of less than 5%.15,17,18 The clinical presentation of pituitary apoplexy frequently includes rapidly progressing headache, meningismus, visual field deficits, cranial nerve deficits, and symptoms related to hypopituitarism.15
 Preoperative Evaluation of Patients with Nonfunctioning Pituitary Adenomas
Preoperative Evaluation of Patients with Nonfunctioning Pituitary Adenomas
A complete endocrine evaluation is indicated in all patients presenting with symptoms of mass effect from an NFA. This typically includes measurement of serum GH and insulin-like growth factor-1 (IGF-1), morning cortisol, free thyroxine (FT4) and prolactin levels in all patients, luteinizing hormone/follicle-stimulating hormone (LH/FSH) levels in women, and testosterone levels in men. Furthermore, a standard Humphrey visual field examination should be performed by an ophthalmologist, as many visual field deficits are subtle on clinical examination. Standard radiographic workup includes magnetic resonance imaging (MRI) with and without contrast administration in axial, sagittal, and coronal sellar views. Key factors to consider on MRI when evaluating nonsecreting macroadenomas include the degree of extension into the infrasellar region and the thickness of the sellar floor, any evidence of cavernous sinus invasion and relationship to the internal carotid arteries and cranial nerves, the extent of suprasellar and subfrontal extension and relationship to the optic apparatus, the position of the normal pituitary gland relative to the lesion, and finally the degree of retrosellar extension and relationship to the clivus and brainstem (Fig. 13.1).
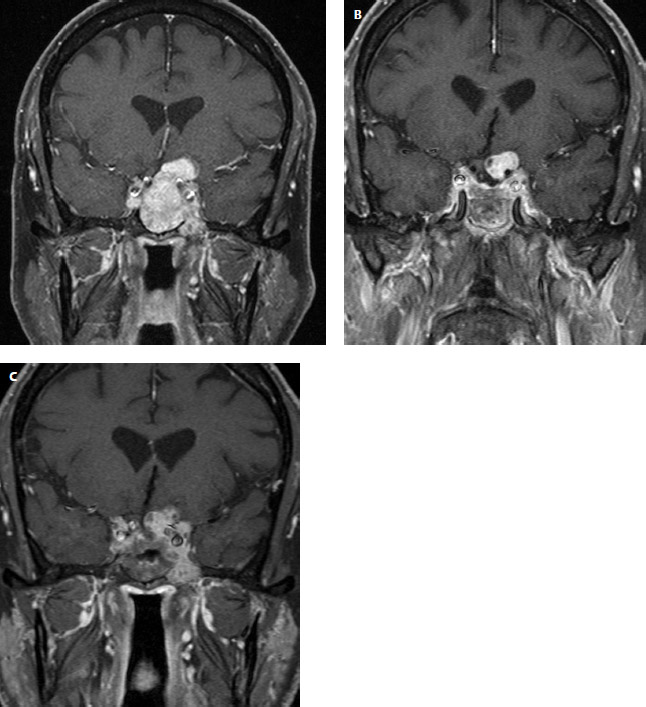
Fig. 13.1 (A) Preoperative coronal postgadolinium magnetic resonance imaging (MRI) showing a typical nonfunctioning pituitary adenoma with suprasellar extension in a 68-yearold man with visual loss. Note the degree of invasion of both cavernous sinuses and involvement of the internal carotid arteries. (B) Postoperative coronal gadolinium-enhanced MRI following transsphenoidal resection of the sellar component of the lesion. Residual lesion is identified in the suprasellar and parasellar regions, necessitating postoperative radiosurgery. (C) Coronal gadolinium-enhanced MRI of the same patient 1 year following transsphenoidal surgery and gamma knife radiosurgery. There is a small degree of progression in the left parasellar region, yet the tumor is otherwise controlled.
 The Natural History of Nonfunctioning Adenomas
The Natural History of Nonfunctioning Adenomas
The natural history of unresected pituitary adenomas has been reported in few studies. As expected, the major factor that determines patient outcome in these cases is tumor size. The authors of one study reviewed 40 patients with NFAs who did not undergo surgery for a variety of reasons.19 They determined that 19% of microadenomas and 44% of macroadenomas demonstrated interval growth on follow-up imaging at a 4-year follow-up. New or worsening visual deficits were observed in 67% of macroadenomas and were absent in all microadenomas. The authors recommended that a watchful waiting policy for nonfunctioning pituitary microadenomas is reasonable in the absence of significant symptoms, whereas macroadenomas should be evaluated for resection. In a separate study, the authors reviewed their experience with 28 patients with unresected nonfunctioning macroadenomas.20 Fifty percent of these patients had an increase in tumor size in a mean follow-up time of 85 months. In turn, 50% of the patients with enlargement in tumor size had progression of visual field deficits requiring surgery.
Our institutional preference has been to offer resection of nonfunctioning pituitary macroadenomas to patients who are acceptable surgical candidates, regardless of visual status. This avoids the potential for developing irreversible symptoms and provides for safer tumor resection, as well as decreases the risk of postoperative visual deterioration. Furthermore, the risk of developing pituitary apoplexy, which has been reported to be higher in patients harboring NFAs than in those with other adenomas, is reduced.15 In the absence of symptoms, nonfunctioning microadenomas can be observed with interval imaging, based on clinical status and patient preference. A possible exception to this rule is the category of primarily suprasellar NFAs. In this location, resection may be indicated in smaller lesions, based on the propensity of patients with these lesions for developing significant visual or hormonal deficits.9
 Medical Management of Nonfunctional Pituitary Adenomas
Medical Management of Nonfunctional Pituitary Adenomas
In general, the medical management of NFAs has been anecdotal and unsubstantiated. Dopamine agonists may decrease gonadotropin and α-subunit production, but their clinical efficacy in patients with NFAs has been marginal. Despite occasional declines in elevated serum prolactin levels caused by tumor stalk effect, tumor shrinkage has been the exception rather than the rule.3 Somatostatin analogues have also been used, with reports of mild visual improvement in 20 to 40% of cases, yet there is only anecdotal evidence of tumor regression.8
 Surgical Management of Nonfunctional Pituitary Adenomas
Surgical Management of Nonfunctional Pituitary Adenomas
The decision to offer resection of an NFA is based on careful evaluation of a patient’s clinical presentation, MRI, serum hormonal assessment, and formal visual field testing. This decision must be individualized to each patient’s particular situation and preferences. As in all cases, medical comorbidities and the patient’s overall clinical status must be carefully considered. Regarding age limitations for surgery, one study demonstrated that transsphenoidal surgery for NFAs in elderly patients (older than 70 years of age) is both safe and effective, with the only significant variation in outcome being a lower rate of hormonal axis recovery.21
In most cases, resection of NFAs can be safely accomplished via a transsphenoidal approach. Some tumors with primarily suprasellar, parasellar, or subfrontal extension require resection via a standard transcranial approach.9 In recent years, extended transsphenoidal techniques have been used to resect lesions with subfrontal and clival extension.22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


