Purpose
To investigate the impact of clinical factors on the recurrence of anterior segment neovascularization after intravitreal bevacizumab injection.
Design
Retrospective, consecutive, interventional case series.
Methods
Charts of 54 eyes of 54 consecutive patients who received intravitreal bevacizumab injections (1.25 mg) for the treatment of anterior segment neovascularization were reviewed. The mean follow-up period ± standard deviation was 16 ± 8 months (range, 4 to 31 months). For eyes with incomplete panretinal photocoagulation, additional retinal ablation was performed within 1 month after bevacizumab injection. Differences in clinical factors were compared between eyes with and without recurrence. Baseline clinical factors were age, gender, predisposing diagnosis, status and clinical stages of anterior segment neovascularization, fundus neovascularization, visual acuity, baseline intraocular pressure, previous retinal ablation, previous intraocular surgeries, lens status, history of glaucoma, hemoglobin A1c level, hypertension, and creatinine level. Factors after intravitreal bevacizumab administration were additional retinal ablation, intraocular surgeries, mean intraocular pressure until recurrence, and visual acuity. Univariate and multivariate Cox proportional hazards regression analyses were performed to evaluate the contribution of these factors to recurrence. Kaplan-Meier survival analysis with the log-rank test was performed with recurrence as the end point.
Results
Recurrence occurred in 26 (48%) eyes a mean ± standard deviation of 4.7 ± 3.0 months (range, 2 to 11 months) after bevacizumab injection. Multivariate analysis identified trabeculectomy after bevacizumab injection as the primary inhibitory factor for recurrence (hazard ratio, 0.23; 95% confidence interval, 0.094 to 0.55; P = .001). Kaplan-Meier survival analysis showed that trabeculectomy after bevacizumab injection provided a significantly better survival rate ( P < .001).
Conclusions
Recurrence of anterior segment neovascularization after intravitreal bevacizumab injection occurs despite intensive retinal ablation: trabeculectomy may suppress recurrence.
Bevacizumab, a humanized monoclonal antibody against vascular endothelial growth factor (VEGF) that was developed for the treatment of metastatic colorectal cancer, has been reported to cause rapid and consistent regression of anterior segment neovascularization when administered into the vitreous cavity or anterior chamber. However, because the aqueous half-life of a single intravitreal bevacizumab injection in human eyes is approximately 10 days, the inhibitory effect of bevacizumab is regarded as transient. In fact, more than half of patients with iris neovascularization or open-angle neovascular glaucoma (NVG) showed recurrence of anterior segment neovascularization 1 to 4 months after intravitreal bevacizumab injections. Such recurrence may promote obstruction and closure of the angle and may raise the intraocular pressure (IOP) and is regarded as a sign of deterioration of NVG. Therefore, additional retinal ablation is recommended after a bevacizumab injection for eyes with insufficient retinal ablation.
However, recurrence of anterior segment neovascularization was reported even in eyes that received extensive panretinal photocoagulation (PRP) after intravitreal bevacizumab injection. Currently, it is unknown what clinical factors are associated with recurrence except for the lack of sufficient retinal ablation. In the current study, we investigated the recurrence of anterior segment neovascularization after intravitreal bevacizumab injection and the relationships between recurrence and various clinical factors such as patient background and those occurring after bevacizumab intervention.
Methods
We retrospectively reviewed the charts of 81 eyes of 66 consecutive patients with anterior segment neovascularization who received intravitreal bevacizumab injections (1.25 mg/0.05 mL Avastin; Roche Pharmaceuticals, Basel, Switzerland) at Kanazawa University Hospital from November 2006 through March 2009. We classified all cases into the following 3 clinical stages of anterior segment neovascularization: (1) preglaucoma stage (IOP ≤ 21 mm Hg with no medication); (2) NVG stage with limited peripheral anterior synechia (PAS; IOP > 21 mm Hg and PAS ≤ 50%); and (3) NVG stage with advanced PAS (IOP > 21 mm Hg and PAS > 50%). IOP was measured using Goldmann applanation tonometry.
Of the 66 patients reviewed, 5 were excluded from the study because of insufficient follow-up (< 4 months). Three patients were excluded because they received intravitreal bevacizumab before referral to our department. Three patients were excluded because they underwent a second intravitreal bevacizumab injection for cystoid macular edema before any recurrence of anterior segment neovascularization was detectable. One patient whose eye received no retinal ablation combined with intravitreal bevacizumab before the recurrence was excluded. When a patient had bevacizumab treatment in both eyes, only the first eye was included in the study sample. When the first eye met the exclusion criteria, the second eye was considered for inclusion. Accordingly, a total of 54 eyes of 54 patients were included in this study.
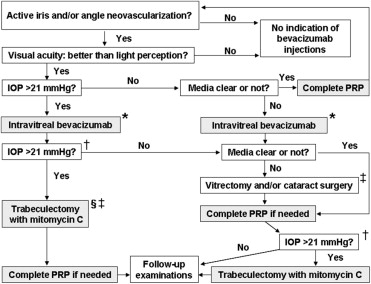
Our treatment strategies of active anterior segment neovascularization are shown in Figure 1 . For eyes with visual acuity better than light perception, intravitreal bevacizumab injection was considered when IOP was more than 21 mm Hg (i.e., NVG stage) or when opaque media prevented completion of transpupillary PRP in the preglaucoma stage. Before bevacizumab injection, transpupillary PRP was performed where possible. Intravitreal bevacizumab injections were performed as previously described. As an intervention after bevacizumab injection, trabeculectomy with mitomycin C was performed as described previously when IOP under maximum medication remained at more than 21 mm Hg. Before trabeculectomy, transpupillary PRP was performed where possible. Trabeculectomy was combined with vitrectomy, cataract surgery, or both when completion of transpupillary PRP was not expected to be possible after surgery. After trabeculectomy, PRP was performed if needed. For eyes with IOP under control after bevacizumab injection, vitrectomy, cataract surgery, or both were indicated when opaque media persisted and prevented completion of PRP. PRP was added during surgery when vitrectomy was performed. After these surgeries, PRP was performed if needed, and trabeculectomy was indicated when IOP under maximum medication remained at more than 21 mm Hg. For all eyes, completion of PRP was planed within 1 month after intravitreal bevacizumab.
The interval between bevacizumab injections and trabeculectomy (mean ± standard deviation, 13 ± 19 days; range, 1 to 83 days) was dependent on IOP level and the severity of glaucomatous optic nerve damage. Transscleral cyclophotocoagulation was performed when trabeculectomy was not indicated because of patient conditions. When recurrence of anterior segment neovascularization was detected, the eyes were treated with PRP, additional injections of intravitreal bevacizumab, or both.
The iris and the angle were examined carefully by slit-lamp biomicroscopy under high magnification using a Goldmann 2-mirror gonio lens to check for the presence of neovascularization before bevacizumab injection and at follow-up visits monthly for the first year and once every several months thereafter. Neovascularization at baseline was graded according to the classification of Teich and Walsh. Iris grading was as follows: grade 0, no neovascularization present; grade 1, fine surface neovascularization of the pupillary zone of the iris involving fewer than 2 quadrants; grade 2, surface neovascularization of the pupillary zone of the iris involving 2 quadrants or more; grade 3, neovascularization of the ciliary zone of the iris, ectropion uveae involving 1 to 3 quadrants in addition to the pupillary zone, or both; and grade 4, neovascularization of the ciliary zone of the iris, ectropion uveae involving more than 3 quadrants in addition to the pupillary zone, or both. Anterior chamber angle grading was as follows: grade 0, no neovascularization; grade 1, fine neovascularization twigs that cross the scleral spur and ramify on the trabecular meshwork involving fewer than 2 quadrants; grade 2, neovascularization twigs across the scleral spur that ramify on the trabecular meshwork involving 2 quadrants or more; grade 3, PAS involving 1 to 3 quadrants as well as the trabecular meshwork neovascularization; and grade 4, PAS involving more than 3 quadrants in addition to neovascularization of the trabecular meshwork. Regarding the status of fundus neovascularization, we defined the advanced stage of neovascularization as presence of vitreous hemorrhage or neovascular membrane with or without tractional retinal detachment.
Recurrence of neovascularization after intravitreal bevacizumab injection was defined as reappearance of neovascular vessels in the iris or the angle of eyes with complete regression of neovascularization. In eyes with incomplete regression of neovascularization, recurrence was defined as a marked increase in visibility of anterior segment neovascular vessels. To detect recurrence uniformly in all cases, we used a standardized procedure of observation: all patients had the same follow-up schedule and all observations were carried out using the same type of gonio lens at the same magnification. For 1 patient, 1 glaucoma specialist performed all follow-up examinations at all visits.
Data Analysis
The main outcome measure was the recurrence of anterior segment neovascularization after intravitreal bevacizumab injection. We investigated the relationships between recurrence and various clinical factors. Baseline clinical factors that we explored were: age, gender, predisposing diagnosis, clinical stage of anterior segment neovascularization, sites and grade of anterior segment neovascularization, status of fundus neovascularization, IOP before bevacizumab injection, number of glaucoma medications, previous glaucoma surgery, previous PRP, previous vitrectomy, lens status, previous diagnosis of other glaucoma types, hemoglobin A1c level, hypertension, and creatinine level. Postintravitreal bevacizumab clinical factors tested were: additional PRP, vitrectomy, cataract surgery, trabeculectomy, cyclophotocoagulation, and mean IOP during the period between bevacizumab injections and recurrence. For PRP, we used fewer than 1000 as the number of photocoagulation spots to indicate insufficient PRP before bevacizumab injection and also 1000 or more for significant addition of PRP after intravitreal bevacizumab.
Best-corrected visual acuity (VA) was measured using the Landolt C acuity chart at baseline and the final visit. BCVA was converted into logarithm of the minimal angle of resolution format (counting fingers, 2.3; hand movements, 2.6; light perception, 3.0; no light perception, 3.6). A marked decrease in BCVA was defined as an increase in logarithm of the minimal angle of resolution of more than 0.3.
The Fisher exact probability test was performed to examine the difference in the sites of anterior segment neovascularization at baseline and recurrence and to compare the recurrence rates between cases with trabeculectomy only and combined surgery and between complete and incomplete regression cases. The Wilcoxon signed-ranks test was used to compare grades of neovascularization at baseline and recurrence and to compare IOP data between just before and at recurrence in cases with recurrence. To examine the difference in clinical factors between eyes with and without recurrence, the Fisher exact probability test or Mann–Whitney U test was used. Cox proportional hazards regression analysis was used to examine the contribution of clinical factors to the recurrence of anterior segment neovascularization after bevacizumab injection. Individual clinical factors were subjected to univariate Cox proportional hazards regression analysis and subsequently were entered in the multivariate analysis in a forward stepwise manner if the P value was less than .2. If a clinical factor occurred infrequently (n < 5), the factor was excluded from the univariate analysis. The criterion for retention in the multivariate model was P < .05. A Kaplan-Meier survival analysis with log-rank test was performed with the recurrence of anterior segment neovascularization as the end point.
Statistical analyses were performed using SPSS statistical software version 17.0J for Windows (SPSS, Inc, Chicago, Illinois, USA). P < .05 was considered statistically significant for all analyses.
Results
The baseline patient characteristics are shown in Table 1 . Mean IOP ± standard deviation before intravitreal bevacizumab injection was 18 ± 4 mm Hg, 31 ± 9 mm Hg, and 37 ± 12 mm Hg in eyes with stages of preglaucoma, glaucoma with limited PAS, and glaucoma with advanced PAS, respectively. All cases showed regression of anterior segment neovascularization after bevacizumab injection. Recurrence of neovascularization appeared in 26 (48%) cases a mean ± standard deviation of 4.7 ± 3.0 months (range, 2 to 11 months) after bevacizumab injection. Of 26 eyes, 21 (81%) eyes recurred as a result of complete regression, whereas 5 (19%) eyes occurred as a result of incomplete regression. At 1 month after bevacizumab injection, 40 (74%) cases showed complete regression, whereas 14 (26%) cases showed incomplete regression. Among 40 complete cases at 1 month, 17 (43%) cases showed recurrence. Among 14 incomplete cases at 1 month, neovascularization in 9 cases became complete regression at 2 to 9 months after bevacizumab injection. Among these cases, 4 (44%) cases showed recurrence. The remaining 5 cases all showed recurrence from incomplete regression. The recurrence rate was significantly higher in cases with incomplete regression (100%) than in those with complete regression (43%; P = .021).
| Recurrence | ||||
|---|---|---|---|---|
| Factors | Yes (n = 26) | No (n = 28) | P Value | All Cases (n = 54) |
| Mean age ± SD, yrs | 63 ± 13 | 63 ± 13 | .85 a | 63 ± 13 |
| Range | 35 to 85 | 31 to 84 | 31 to 85 | |
| Gender | .36 b | |||
| Male | 18 (69%) | 17 (61%) | 35 (65%) | |
| Female | 8 (31%) | 11 (39%) | 19 (35%) | |
| Predisposing diagnoses | .21 b | |||
| Proliferative diabetic retinopathy | 16 (62%) | 21 (75%) | 37 (69%) | |
| Central retinal vein occlusion | 6 (23%) | 6 (21%) | 12 (22%) | |
| Ocular ischemic syndrome | 3 (12%) | 0 (0%) | 3 (6%) | |
| Central retinal artery occlusion | 0 (0%) | 1 (4%) | 1 (2%) | |
| Radiation retinopathy | 1 (4%) | 0 (0%) | 1 (2%) | |
| Clinical stages | .082 a | |||
| Preglaucoma | 4 (15%) | 2 (7%) | 6 (11%) | |
| NVG with PAS ≤ 50% | 15 (58%) | 12 (43%) | 27 (50%) | |
| NVG with PAS > 50% | 7 (27%) | 14 (50%) | 21 (39%) | |
| Sites of neovascularization | .19 b | |||
| Iris only | 1 (4%) | 6 (21%) | 7 (13%) | |
| Angle only | 6 (23%) | 5 (18%) | 11 (20%) | |
| Iris and angle | 19 (73%) | 17 (61%) | 36 (67%) | |
| Grade of iris neovascularization | .59 a | |||
| Grade 0 | 6 (23%) | 5 (18%) | 11 (20%) | |
| Grade 1 | 8 (31%) | 9 (32%) | 17 (31%) | |
| Grade 2 | 10 (38%) | 10 (36%) | 20 (37%) | |
| Grade 3 | 1 (4%) | 2 (7%) | 3 (6%) | |
| Grade 4 | 1 (4%) | 2 (7%) | 3 (6%) | |
| Grade of angle neovascularization | .88 a | |||
| Grade 0 | 1 (4%) | 6 (21%) | 7 (13%) | |
| Grade 1 | 7 (27%) | 4 (14%) | 11 (20%) | |
| Grade 2 | 9 (35%) | 5 (18%) | 14 (26%) | |
| Grade 3 | 5 (19%) | 6 (21%) | 11 (20%) | |
| Grade 4 | 4 (15%) | 7 (25%) | 11 (20%) | |
| Advanced stage of fundus neovascularization | 7 (27%) | 4 (14%) | .21 b | 11 (20%) |
| Best-corrected visual acuity | .91 a | |||
| Counting fingers or worse | 9 (35%) | 7 (25%) | 16 (30%) | |
| 0.01 to 0.1 | 6 (23%) | 9 (32%) | 15 (28%) | |
| 0.2 to 0.5 | 5 (19%) | 7 (25%) | 12 (22%) | |
| 0.6 to 1.0 | 6 (23%) | 5 (18%) | 11 (20%) | |
| Mean IOP ± SD before bevacizumab injection, mm Hg | 30 ± 13 | 34 ± 10 | .078 a | 32 ± 12 |
| Range | 14 to 60 | 12 to 58 | 12 to 60 | |
| Mean number of glaucoma medications ± SD | 1.9 ± 1.5 | 2.5 ± 1.3 | .092 a | 2.2 ± 1.4 |
| Range | 0 to 4 | 0 to 4 | 0 to 4 | |
| Previous glaucoma surgery | 2 (8%) | 3 (11%) | .54 b | 5 (9%) |
| Previous PRP (< 1000 shots) | 9 (35%) | 8 (29%) | .43 b | 17 (31%) |
| Previous vitrectomy | 1 (4%) | 5 (18%) | .11 b | 6 (11%) |
| Lens status | .041 b | |||
| Phakia | 18 (69%) | 11 (39%) | 29 (54%) | |
| Intraocular lens | 8 (31%) | 16 (57%) | 24 (44%) | |
| Aphakia | 0 (0%) | 1 (4%) | 1 (2%) | |
| Previous diagnosis of other glaucoma types | 2 (8%) | 6 (21%) | .15 b | 8 (15%) |
| Diabetes mellitus | 20 (77%) | 24 (86%) | .32 b | 44 (81%) |
| HbA1c (%) | .49 a | |||
| Nondiabetic patients | 6 (23%) | 4 (14%) | 10 (19%) | |
| 4.3 to 5.8 (excellent control) | 1 (4%) | 3 (11%) | 4 (7%) | |
| 5.9 to 6.4 (good control) | 1 (4%) | 5 (18%) | 6 (11%) | |
| 6.5 to 7.9 (fair control) | 7 (27%) | 8 (29%) | 15 (28%) | |
| 8.0 or more (poor control) | 11 (42%) | 8 (29%) | 19 (35%) | |
| Hypertension | 16 (62%) | 17 (61%) | .59 b | 33 (61%) |
| Renal dysfunction (creatinine > 1.5 mg/dL) | 3 (12%) | 4 (14%) | .54 b | 7 (13%) |
| Mean follow-up ± SD (mos) | 15 ± 8 | 16 ± 8 | .83 a | 16 ± 8 |
| Range | 4 to 31 | 4 to 29 | 4 to 31 | |
In 26 recurrent eyes, sites and grades of anterior segment neovascularization at the recurrence were significantly different from those at baseline ( Table 2 ). Although most cases showed neovascularization in both the iris and angle at baseline, recurrence frequently was restricted to either the iris or the angle. Half of the cases had recurrence limited to the angle.
| Baseline | Recurrence | P Value | |
|---|---|---|---|
| Sites of neovascularization | < .001 a | ||
| Iris only | 1 (4%) | 7 (27%) | |
| Angle only | 6 (23%) | 15 (58%) | |
| Iris and angle | 19 (73%) | 4 (15%) | |
| Grade of iris neovascularization | .001 b | ||
| Grade 0 | 6 (23%) | 15 (58%) | |
| Grade 1 | 8 (31%) | 9 (35%) | |
| Grade 2 | 10 (38%) | 1 (4%) | |
| Grade 3 | 1 (4%) | 0 (0%) | |
| Grade 4 | 1 (4%) | 1 (4%) | |
| Grade of angle neovascularization | .047 b | ||
| Grade 0 | 1 (4%) | 7 (27%) | |
| Grade 1 | 7 (27%) | 8 (31%) | |
| Grade 2 | 9 (35%) | 3 (12%) | |
| Grade 3 | 5 (19%) | 5 (19%) | |
| Grade 4 | 4 (15%) | 3 (12%) |
a Fisher exact probability test.
Among 26 cases with recurrence of anterior segment neovascularization, 10 (38%) cases received additional injections of intravitreal bevacizumab and PRP to treat the recurrence. The second injections were performed a mean ± standard deviation of 3.7 ± 1.5 months (range, 2 to 7 months) after the first injection. Three cases received a third injection 3 to 5 months after the first injection to treat a second recurrence. The remaining 16 cases were treated with transpupillary PRP.
There were no significant differences in baseline factors between eyes with and without recurrence except for lens status ( Table 1 ). Regarding fundus neovascularization, the proportion of eyes with advanced stage of neovascularization (i.e., vitreous hemorrhage or neovascular membrane with or without tractional retinal detachment) was not significantly different between eyes with and without recurrence. However, all eyes with neovascular membrane in the fundus showed recurrence (n = 4). The proportion of eyes with neovascular membrane was significantly higher in eyes with recurrence than in eyes without ( P = .041). Among factors occurring after intravitreal bevacizumab treatment, trabeculectomy was performed more frequently in eyes without recurrence ( P < .001; Table 3 ). Regarding the combined surgeries, 7 cases underwent combined trabeculectomy with cataract surgery, vitrectomy, or both, whereas 21 cases underwent trabeculectomy only. Recurrence of neovascularization occurred in 1 (14%) and 6 (29%) cases in the combined surgery and trabeculectomy alone groups, respectively. The difference was not statistically significant ( P = .42). Mean IOP until recurrence was higher in eyes with recurrence than in eyes without ( P = .014; Table 3 ). The IOP course after bevacizumab injection is shown in Figure 2 . The IOP in eyes with recurrence was significantly higher than in eyes without recurrence at 2 to 5 months after injection. Mean IOP ± standard deviation at recurrence (19 ± 9 mm Hg; range, 5 to 47 mm Hg) was significantly higher than just before recurrence (16 ± 5 mm Hg; range, 7 to 27 mm Hg; P = .002). With respect to BCVA, a marked decrease in BCVA occurred in 4 (15%) eyes with recurrence and in 3 (11%) eyes without recurrence. The difference was not statistically significant ( P = .46).



