11
Clinical Evaluation of the Cranial Nerves
Abraham Jacob and D. Bradley Welling
Diagnostic evaluation of the cranial nerves (CNs) begins with understanding their anatomy, requires obtaining a detailed patient history, and calls for a thorough bedside evaluation. Cranial base imaging (Chapter 7) and the use of neuro-diagnostic electrical tests are becoming common clinical adjuncts for evaluating neural integrity. In modern otology and neurotology, the preoperative and intraoperative assessment of CN integrity may help optimize each patient’s post-operative outcome.
 Anatomy and Bedside Evaluation of Cranial Nerves
Anatomy and Bedside Evaluation of Cranial Nerves
The first step in assessing the CNs is understanding the anatomy and performing a basic bedside evaluation. Fig. 11–1 illustrates the topographic anatomy of the brainstem. CNs I and II are direct extensions of the central nervous system (CNS), CNs III and IV arise from the midbrain, CNs V to VIII originate in the pons, and CNs IX to XII arise from the medulla.
Cranial Nerve I: Olfactory Nerve
The olfactory system is made up of specialized olfactory epithelium, olfactory bulbs, olfactory tracts, and their central projections. This epithelium, present along the superior concha, superior nasal septum, and nasal vault, is made up of bipolar sensory receptors that also serve as first-order neurons. Approximately 20 filaments traverse the cribriform plate and enter the anterior cranial fossa on each side of the crista galli. These first-order axons synapse with mitral and tufted cells (second-order neurons) in the olfactory bulbs. Central projections from the olfactory bulbs then travel primarily to the limbic system. These projections, termed olfactory tracts, arise from the posterior aspect of each olfactory bulb and project to the lateral (primary), intermediate, and medial olfactory areas. Periamygdaloid and prepiriform areas are thought to make up the primary olfactory cortex, whereas the entorhinal area functions as a secondary olfactory cortex.1 The bedside evaluation of olfaction begins with a complete (including endoscopic) nasal, sinus, and nasopharyngeal examination. The patient is then asked to identify familiar aromatic odors delivered separately to each nostril. A variety of odorant delivery devices are commercially available.
Cranial Nerve II: Optic Nerve
Visual inputs, transformed into electrical signals by the retina, are transmitted centrally via the optic nerve (Fig. 11–2). This nerve enters the middle cranial fossa through the optic canal, an opening in the lesser wing of the sphenoid bone. It unites with the contralateral optic nerve at the optic chiasm where fibers from the medial (nasal) half of each retina cross into the contralateral optic tract. Each optic tract, central to the chiasm, travels to the lateral geniculate nucleus of the thalamus. Optic radiations then leave the thalamus, pass through the internal capsule, and terminate in each occipital lobe’s primary visual cortex. The bedside evaluation of CN II includes testing basic visual acuity (Snellen chart), performing an ophthalmoscopic examination, testing pupillary response to light (afferent limb of a neural arc involving the second CN), and testing the patient’s visual fields. Visual field defects can help localize the “site of lesion” along the visual pathway. A more detailed evaluation generally requires consultation with the ophthalmology service.
Cranial Nerves III, IV, and VI: Oculomotor Complex and Abducens Nerves
The oculomotor complex (oculomotor and Edinger-Westphal nuclei) is located in the midbrain ventral to the cerebral aqueduct (Fig. 11–3). The oculomotor nerve itself emerges ventrally from the caudal midbrain, passes between the posterior cerebral and superior cerebellar arteries, and enters the lateral aspect of the cavernous sinus. It then enters the orbit through the superior orbital fissure. Just inside the orbit, CN III splits into superior and inferior divisions. The superior division supplies motor input to the superior rectus and levator palpebrae muscles, whereas the inferior division innervates the medial rectus, inferior rectus, and inferior oblique. This inferior division also carries preganglionic parasympathetic fibers from the Edinger-Westphal nucleus to the ciliary ganglion. Postganglionic fibers travel to the ciliary body and constrictor pupillae muscles.
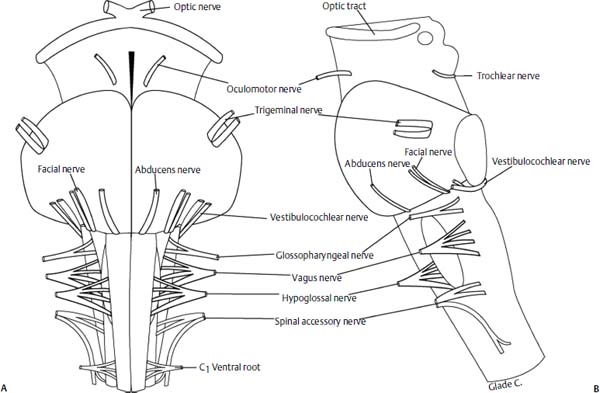
Figure 11–1 Topographic anatomy of the cranial nerves (CNs) at the brainstem in frontal (A) and lateral (B) views. Note that CNs I and II are direct extensions of the central nervous system, CN III and IV arise from the midbrain, CN V to VIII originate in the pons, and CN IX to XII arise from the medulla. (See Figure 11–3 for CN I)
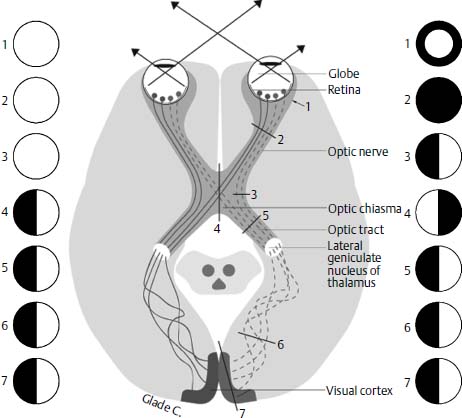
Figure 11–2 The optic pathway. As shown, injuries at various locations along the pathway result in characteristic visual field defects, noted by the darkened areas.
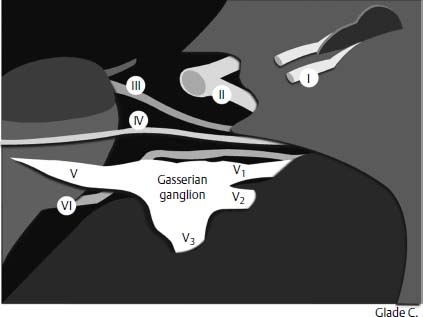
Figure 11–3 Diagram of the anterior and middle cranial fossae depicting the first (olfactory), second (optic), third (oculomotor), fourth (trochlear), fifth (trigeminal), and sixth (abducens) CNs. Note the dorsal origin of the trochlear nerve as well as the ascent of the abducens nerve along the clivus.
The trochlear nerve innervates the superior oblique muscle. Its fibers originate in the midbrain caudal to the oculomotor complex. Interestingly, this nerve decussates within the brainstem before exiting on its dorsal surface. The trochlear nerve travels along the lateral wall of the cavernous sinus just inferior to the oculomotor nerve prior to entering the orbit through the superior orbital fissure. This nerve has the longest intracranial course of any CN.
The abducens nerve provides motor input to the lateral rectus muscle. Its nucleus is located in the pons anterior to the fourth ventricle and adjacent to the facial motor nucleus. Axons from the ipsilateral seventh CN loop around the abducens nucleus prior to leaving the brainstem. CN VI exits the ventral pontomedullary junction, travels rostrally along the clivus, passes through Dorello’s canal, and emerges within the cavernous sinus. It enters the orbit through the superior orbital fissure.
CNs III, IV, and VI move the globe, regulate pupil diameter, and help retract the upper eyelid. The bedside evaluation of these nerves requires inspection of the upper eyelids for ptosis, assessment of each upper lid for adequate lid retraction during eye opening, testing extraocular motion, measuring pupil size and symmetry, and testing both the direct and consensual pupillary response to light.
Cranial Nerve V: Trigeminal Nerve
The principal brainstem nuclei of CN V are the motor (masticator) nucleus and the pontine (sensory) trigeminal nucleus (Figs. 11–3 and 11–4). A rostral extension of the pontine nucleus makes up the mesencephalic nucleus, whereas its caudal extension into the dorsal gray matter of the spinal cord is called the nucleus of the spinal trigeminal tract. The trigeminal nerve emerges from the mid-lateral pons as a large sensory and smaller motor root. Its principal sensory ganglion, the semilunar or Gasserian ganglion, is situated in Meckel’s cave along the anterior-medial floor of the middle cranial fossa. From the ganglion, three divisions of the nerve (ophthalmic V1, maxillary V2, and mandibular V3) exit the intracranial space through the superior orbital fissure, foramen rotundum, and foramen ovale, respectively. The ophthalmic division divides into its four terminal branches (the frontal nerve, nasociliary nerve, lacrimal nerve, and a meningeal branch) within the orbit. The maxillary division splits into a meningeal branch, the zygomatic nerve, infraorbital nerve, and the superior alveolar nerve within the pterygopalatine fossa. The peripheral ganglion of the maxillary nerve, the pterygopalatine ganglion, is located within the pterygopalatine fossa. The mandibular nerve traverses the foramen ovale and enters the infratemporal fossa. Here it divides into its terminal branches, the auriculotemporal nerve, the buccal nerve, the lingual nerve, and the inferior alveolar nerve. The peripheral ganglion of the trigeminal nerve, the otic ganglion, is situated in the infratemporal fossa. The trigeminal nerve provides motor innervation to the muscles of mastication, the mylohyoid, the anterior belly of the digastric muscle, the tensor tympani, and the tensor veli palatini muscles. It also receives general sensory information from the face and scalp (up to the vertex of the head) ocular conjunctiva, paranasal sinuses and nasal cavity, oral cavity (including tongue and dentition) anterior ear canal, lateral surface of the tympanic membrane, and the meninges of the anterior and middle cranial fossa.
Primary bedside evaluation of the trigeminal nerve assesses cutaneous sensation of the face and scalp, intraoral sensation along the tongue, buccal mucosa, floor of mouth, and alveolar ridges, and evaluates the corneal reflex (afferent limb mediated by CN V1). The muscles of mastication can be tested for symmetry by having patients clench their teeth.
Cranial Nerve VII: Facial Nerve
CN VII emerges from the caudal pons, passes through the cerebellopontine angle (CPA), and enters the internal auditory canal (IAC), where it assumes an anterior-superior position at the fundus (Fig. 11–5). Several named segments characterize its intratemporal course, including the labyrinthine, geniculate, tympanic (horizontal), and mastoid (vertical) segments. The nerve exits the temporal bone through the stylomastoid foramen and divides at the pes anserinus into temporozygomatic and cervicofacial trunks. These primary branches then split into five terminal branches: the frontal (temporal), orbital, buccal, marginal mandibular, and cervical nerves.
The facial nerve contains parasympathetic fibers from the superior salivatory nucleus, motor fibers from the facial motor nucleus, taste afferents to the nucleus solitarius, and general sensory afferents to the spinal trigeminal tract. The nerve is motor to the stapedius muscle, the stylohyoid, the posterior belly of digastric, the auricular muscles, muscles of facial expression, the buccinator, and the platysma. Parasympathetic innervation of the lacrimal gland occurs via the greater superficial petrosal nerve. The chorda tympani nerve stimulates salivation from the submandibular and sublingual glands. Special sensory fibers within the chorda tympani also transmit taste afferents from the anterior two-thirds of the tongue, whereas the greater superficial petrosal nerve mediates taste from the posterior soft palate. General sensation from the posterior meatal skin of the ear canal is also carried by the facial nerve.
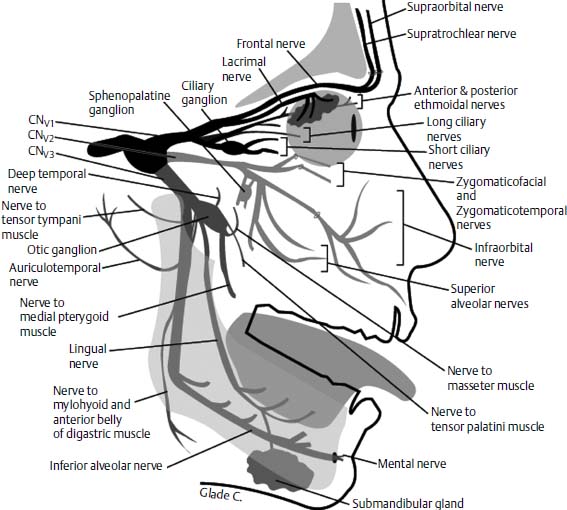
Figure 11–4 Diagrammatic representation of the V1, V2, and V3 divisions of the trigeminal nerve.
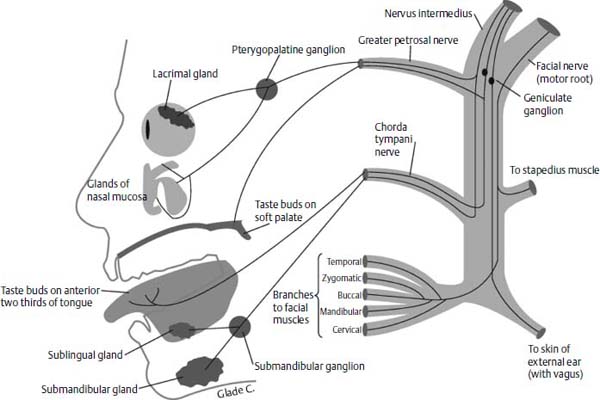
Figure 11–5 Facial nerve innervation. This nerve stimulates lacrimation and nasal secretions, contributes to taste sensation along the soft palate and anterior tongue, is motor to the mimetic facial musculature, and sensory to the skin of external auditory meatus.
The initial patient examination should classify the extent of facial weakness (House-Brackmann scale) and approximate the location of nerve injury. The upper face enjoys bilateral central motor innervation. As a result, brainstem and peripheral facial nerve injuries cause a complete, unilateral paralysis, whereas injuries rostral to the facial motor nucleus spare the upper face. Because the facial and abducens nuclei are in close proximity within the pons, concomitant facial paralysis and lateral rectus palsy suggest a brainstem lesion. Involvement of the facial nerve in the CPA usually occurs late in CPA diseases. Other CNs, especially CN VIII, are typically involved prior to the onset of facial weakness. The physical examination may help localize the site of intratemporal facial nerve injury. Disruption of the nerve at the stylomastoid foramen causes facial paralysis without changes in taste, lacrimation, or salivation. Lesions near the geniculate ganglion result in facial paralysis, altered lacrimation, decreased salivation, and taste dysfunction. Injuries distal to the geniculate ganglion but proximal to the chorda tympani nerve cause facial paralysis, loss of taste, and diminished salivation but do not affect lacrimation. Injuries distal to the stylomastoid foramen affect specific peripheral branches of the nerve.
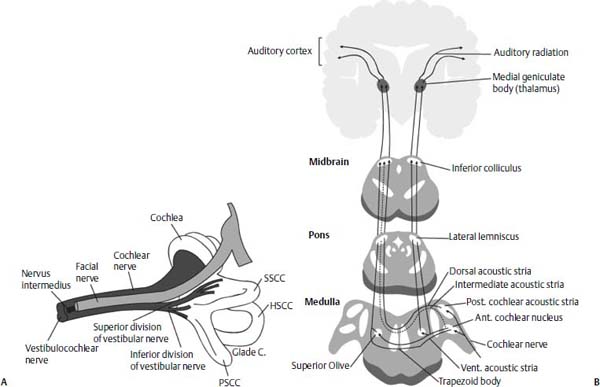
Figure 11–6 (A) Anatomy of the seventh (facial) and eighth (vestibulocochlear) CNs. At the fundus of internal auditory canal, the facial nerve is in the anterior-superior quadrant, the cochlear nerve is in the anterior-inferior quadrant, and the superior and inferior vestibular nerves are in the posterior-superior and posterior-inferior quadrants. (B) The central auditory pathways. Note the bilateral representation of auditory inputs at multiple levels within the brainstem. SSCC, HSCC, PSCC; superior, horizontal, and posterior semicircular canals.
Cranial Nerve VIII: Vestibulocochlear Nerve
The vestibulocochlear nerve (Fig. 11–6) exits the brainstem as one nerve but separates into the cochlear nerve, superior vestibular nerve, and inferior vestibular nerve as it approaches the IAC. The cochlear nerve is initially inferior to the vestibular nerve within the CPA but rotates into an anterior-inferior position by the time it reaches the IAC. The superior and inferior vestibular nerves are situated in the posterior-superior and posterior-inferior quadrants, whereas the facial nerve is located in an anterior-superior position at the fundus. Nerve cell bodies in the spiral ganglion (hearing) and Scarpa’s ganglion (balance) transmit information from specialized sensory end-organs within the cochlea (organ of Corti), the utricle and saccule (maculae), and the semicircular canals (cristae).
The auditory pathway begins with cochlear hair cells that transduce mechanical energy into electrical impulses. These impulses are transmitted along the auditory nerve to the ipsilateral cochlear nucleus by the neurons of the spiral ganglion. From the cochlear nucleus, ipsilateral and contralateral auditory pathways are generated. The majority of fibers cross the brainstem and synapse in the contralateral superior olivary complex or pass through the lateral lemniscus to the inferior colliculus. Information is then relayed to the medial geniculate body of the thalamus from which it is transmitted to the primary auditory complex of the temporal lobe.
The bedside evaluation for hearing includes the whisper test and a tuning fork examination. A 512-Hz tuning fork lateralizes toward the ear with a conductive hearing loss and away from the ear with a sensorineural hearing deficit. The Rinne is positive if air conduction (tuning fork next to the pinna) is greater than bone conduction (tuning fork placed on the antrum or mastoid tip). Bone conduction greater than air conduction typically reflects a 25-dB conductive hearing loss (negative Rinne). Bedside balance testing includes evaluating the patient’s gait and performing the Rhomberg or tandem Rhomberg tests. Spontaneous, gaze, positional, and positioning nystagmus should also be sought. A post-head-shake nystagmus will beat away from an ear with unilateral vestibular loss. The presence of a post-head-thrust refixation saccade reflects a vestibular weakness in the ear toward which the head is thrust. Detailed descriptions regarding these and other tests are covered in other chapters.
Cranial Nerve IX: Glossopharyngeal Nerve
The ninth CN provides motor innervation to the stylopharyngeus muscle (nucleus ambiguus), supplies parasympathetic input to the parotid gland (inferior salivatory nucleus), innervates the carotid body and carotid sinus (nucleus solitarius), provides general sensation (trigeminal tract) and taste (nucleus solitarius) to the posterior third of the tongue, and is sensory to a portion of the ear canal and internal surface of the tympanic membrane (trigeminal tract). It exits the medulla as rootlets, which enter the jugular foramen. Superior and inferior glossopharyngeal ganglia are present within the foramen. As the nerve enters the jugular foramen, the tympanic branch (Jacobson’s nerve) separates and enters the middle ear through the inferior (hypotympanic) canaliculus. A plexus is formed on the promontory of the cochlea after which the nerve reconstitutes as the lesser petrosal nerve. This petrosal nerve enters the middle cranial fossa, descends through the foramen ovale, and synapses with the otic ganglion in the infratemporal fossa. Parasympathetic fibers from CN IX eventually join the auriculotemporal nerve (V3) within the otic ganglion.
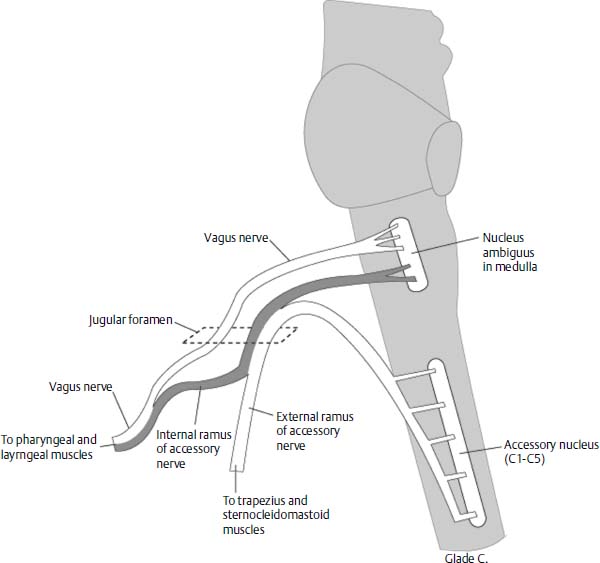
Figure 11–7 The tenth (vagus) and eleventh (spinal accessory) CNs. Note that some fibers initially traveling with the eleventh nerve join the vagus nerve distal to the jugular foramen.
Bedside examination of CN IX involves testing the afferent limb of the oropharyngeal gag reflex and evaluating supraglottic sensation during flexible fiberoptic laryngoscopy. Xerostomia, particularly during mastication, may reflect parotid dysfunction secondary to CN IX palsy.
Cranial Nerve X: Vagus Nerve
A complete description of CN X (Fig. 11–7) anatomy is beyond the scope of this text. In brief, vagal rootlets emerge from the medulla and join as they enter the jugular foramen. The superior (jugular) and inferior (nodose) ganglia of CN X are located within this foramen. Some fibers from the caudal aspect of the nucleus ambiguus exit the brainstem within the spinal accessory nerve (CN XI) but later join CN X after it exits the skull base. Motor branches from the vagus nerve (nucleus ambiguus) include the pharyngeal branch, the superior laryngeal nerve, and the recurrent laryngeal nerve. Parasympathetic fibers (dorsal vagal nucleus) innervate glands within the pharyngeal, laryngeal, gastric, and intestinal mucosa. Visceral sensation from the gut is transmitted to the nucleus solitarius. General sensory afferents from the pharynx, larynx, skin of the external auditory canal (auricular branch), external surface of the tympanic membrane (auricular branch), and meninges of the posterior fossa travel with CN X to the trigeminal tract and nucleus.
Bedside otolaryngologic testing of the vagus nerve includes inspection of the palate during swallowing or phonation; a bedside swallow evaluation to rule out aspiration; appraisal of voice quality for hypernasality, hoarseness, or breathiness; and fiberoptic laryngoscopy to examine vocal cord motion.
Cranial Nerve XI: Spinal Accessory Nerve
The accessory nucleus is located within the spinal cord. Axons from lower motor neurons emerge as rootlets that ascend through the foramen magnum into the posterior cranial fossa. These are joined by fibers of the nucleus ambiguus to form CN XI (Fig. 11–7). The spinal accessory nerve exits the posterior fossa through the jugular foramen and provides motor innervation to the sternocleidomastoid (SCM) and trapezius muscles. Dysfunction of this nerve is manifest by a winged scapula, shoulder weakness, an inability to abduct the arm past 100 degrees, and weakness when turning the head toward the contralateral side.
Figure 11–8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


