Purpose
To determine the clinical and ultrasound biomicroscopy (UBM) features associated with growth in iris melanocytic lesions.
Study Design
Retrospective case series analysis.
Methods
We included all iris melanocytic lesions that were monitored between January 2005 and November 2009. At the end of the analysis, 44 eyes of 44 patients were included in the final analysis. The clinical features analyzed were: iris color, largest base diameter, radial location of the lesion epicenter, circumferential location of the lesion epicenter, lesion configuration, lesion pigmentation, intrinsic vascularity within the lesion, presence of associated pigmentation, the impact on the pupil, presence of iris atrophy, and lesion-induced localized cataracts. The UBM features included lesion thickness, presence of corneal touch, presence of surface plaque, internal structure, and internal reflectivity. Regression analysis was performed to define the features associated with growth.
Results
Twenty-three percent of the lesions showed documented growth. Mean follow-up was 21.4 months (range: 10-48). Clinical features associated with growth were a large basal diameter at baseline ( P = .004) and inferior location ( P = .004). UBM features associated with growth were: a greater baseline thickness ( P = .01), presence of corneal touch ( P = .007), an irregular internal structure ( P = .0001), and the presence of dots and linear streaks ( P < .0001). Clinical features that were not associated with growth were the radial location of the lesion in the iris ( P > .999), lesion configuration ( P > .999), lesion pigmentation ( P > .999), the presence of pigment dispersion ( P = .70), iris freckles ( P = .15), corectopia ( P > .999), ectropion ( P > .999), and intrinsic vascularity ( P = .70). UBM features not associated with growth were the presence of a surface plaque ( P = .07) and the internal reflectivity ( P = .77).
Conclusion
Substantial growth in iris melanocytic lesions is associated with original larger basal diameter and inferior lesion location. On UBM growth is associated with greater original thickness, presence of corneal touch, and an irregular internal structure. Presence of these features could modify the frequency of observation of those lesions.
Iris melanocytic lesions are present in 5% of the population. Most of these lesions present benign cytologic features. Malignant melanocytic iris lesions may arise de novo or from a preexisiting benign lesion. Differentiating between a benign and a malignant lesion may be difficult on clinical grounds alone at initial examination, since no specific features are pathognomonic, particularly in smaller lesions Fine-needle aspiration biopsy (FNAB) of iris melanocytic lesions may yield inaccurate results owing to the cellular hetereogeneity of those lesions or insufficient biopsy material; in addition, there is inherent risk to an invasive ocular procedure.
Uveal nevi may grow over time, which makes the diagnosis even more challenging. However, this growth is generally slow and not progressive. Documented substantial growth remains the main indicator of malignancy.
Several clinical features such as a large basal tumor diameter, presence of pigment dispersion, high intraocular pressure, tumor intrinsic vascularity, and ocular symptoms related to the tumor have been associated with growth. One study demonstrated that the presence of pigment dispersion and medial location of a melanocytic lesion in the iris are associated with growth.
Anterior segment photography and ultrasound biomicroscopy (UBM) are important in monitoring growth in iris melanocytic lesions.
The aim of this study is to evaluate the clinical and UBM features associated with growth in iris melanocytic lesions.
Methods
We retrospectively reviewed the electronic patient records of all consecutive patients with the diagnosis of iris melanocytic lesion (nevus, suspicious nevus, questionable small melanoma), who underwent UBM examination at their initial visit, and we elected to follow to document growth at the ocular oncology department of Princess Margaret Hospital/University Health Network between January 2005 and November 2009.
The exclusion criteria included: 1) follow-up periods shorter than 12 months; 2) nonmelanocytic lesions; and/or 3) lesions with significant ciliary body involvement. Patient demographics, diagnosis at the time of the initial visit, clinical features of the lesion, UBM features, follow-up period, and date of the first documented growth were recorded.
Clinical Features
The clinical features included iris color, largest base diameter (LBD), radial location of the lesion epicenter (iris root, midzone, collarette, pupillary margin, angle/iris root), circumferential location of the lesion epicenter (between clock-hour positions 10:30 and 1:30; 1:30 and 4:30; 4:30 and 7:30; and 7:30 and 10:30), lesion configuration (dome, flat, tapioca, irregular), lesion pigmentation (mixed pigmentation, mainly melanotic, amelanotic), intrinsic vascularity within the lesion, presence of associated pigmentation (iris freckles, pigment dispersion), impact on the pupil (corectopia, ectropion uveae), presence of iris atrophy, and lesion-induced localized cataracts.
The iris lesions were measured using the Visupac software (version 4.3; Carl Zeiss Meditec, Jena, Germany). All of the iris lesions were measured using the same magnification (10×). The photographs before August 2008 were taken using a Nikon D1 camera (Nikon, Tokyo, Japan) mounted on a Nikon FS-3 – zoom photo slit lamp (capture dimension of 23.6 mm × 17.7 mm with a magnification of 1.5 mm). Later, photographs were taken using a Canon EOS 40D camera (Canon, Tokyo, Japan) mounted on a slit lamp Haag-Streit Bx900 (capture dimension of 22 mm × 14.8 mm with a magnification of 1.6 mm) (Haag-Streit, Koeniz, Switzerland). Correction for the difference in the crop factor between both cameras was made (pixel equivalent for the Nikon camera: 1 mm = 59.2 pixels; for the Canon camera: 1 mm = 47.3 pixels).
High-Frequency Ultrasound Biomicroscopy Features
All patients were evaluated using the prototype UBM machine (Paradigm Medical Industries Inc, Salt Lake City, Utah, USA). UBM features included: 1) lesion thickness, which was measured using the calipers of the UBM machine; 2) corneal touch; 3) surface plaque, shown as a superficial layer of hyporeflectivity beneath the surface of the lesion; 4) internal structure (regular and irregular) (in those cases in which an irregular internal structure was noted, we also recorded the presence of linear streaks or dots); and 5) internal reflectivity, which was arbitrarily divided into 3 categories (high, medium, and low reflectivity), determined by comparison to the reflectivity of the iris stroma, which was considered as medium.
Definition of Growth
A substantial growth was defined if the iris lesion showed an increase in basal diameter and/or thickness (assessed by UBM) of ≥20% from the previous visit (6 months earlier), or if there was a progressive increase in a basal diameter or thickness over 2 or more consecutive visits.
Statistical Analysis
Descriptive statistics, including medians, minimums, maximums, and percentages, were used to describe the patient population. Frequency differences between subgroups were analyzed using Fisher exact test. Wilcoxon rank sum test was used for comparing the continuous variables of the larger basal diameter and lesion thickness between subgroups. All P values were 2-sided. Results were considered significant if the P value was less than or equal to .05. Statistical analysis was performed using Version 9.2 of the SAS system and User’s Guide (SAS Institute, Cary, North Carolina, USA).
Results
Forty-five patients did not meet the inclusion criteria as described above. Forty-four patients were included in the analysis. Mean follow-up was 33.6 months (range 12−51 months). The mean number of visits was 4.2 (range 2−8). The average age at the time of the first visit was 59.67 years (range 32−90), with 18 patients (41%) being male. Twenty-six patients (59%) had the iris lesion in the right eye. Forty-three eyes (98%) had a blue-green iris. The most common diagnosis at the time of the first visit was iris nevus in 30 eyes (68%).
The summary of all clinical and UBM features for the 44 patients is shown in Tables 1 and 2 respectively.
| Characteristics | Entire Cohort (n = 44) | Lesions That Grew (n = 10) | P Value |
|---|---|---|---|
| Larger basal diameter at baseline, mean (range) (mm) | 3.63 (1.1−10.3) | 5.06 (1.9−7.2) | .004 |
| Epicenter clock hour | |||
| 10:30 to 1:30 | 1 | 1 | |
| 1:30 to 4:30 | 13 | 1 | .004 |
| 4:30 to 7:30 | 19 | 8 | |
| 7:30 to 10:30 | 11 | 0 | |
| Location of the epicenter of the lesion | |||
| Collarete | 10 | 1 | >.999 |
| Midzone | 20 | 7 | |
| Root | 7 | 0 | |
| Root/angle | 7 | 2 | |
| Involvement of the pupil and/or angle | |||
| Either | 5 | 1 | |
| Angle | 15 | 1 | .15 |
| Pupil | 15 | 4 | |
| Both | 9 | 4 | |
| Configuration of the lesion | |||
| Dome | 11 | 3 | |
| Flat | 19 | 2 | .19 |
| Tapioca | 2 | 0 | |
| Irregular | 12 | 5 | |
| Lesion pigmentation | |||
| Partially melanotic | 8 | 2 | |
| Melanotic | 28 | 6 | >.999 |
| Amelanotic | 8 | 2 | |
| Pigment dispersion | |||
| Absent | 32 | 8 | 0.7 |
| Present | 12 | 2 | |
| Other frekles | |||
| Absent | 19 | 2 | 0.15 |
| Present | 25 | 8 | |
| Corectopia | |||
| Absent | 27 | 6 | >.999 |
| Present | 17 | 4 | |
| Ectropion uveae | |||
| Absent | 26 | 6 | >.999 |
| Present | 18 | 4 | |
| Intrinsic vessels | |||
| Absent | 30 | 6 | .7 |
| Present | 14 | 4 |
| Characteristics | Entire Cohort (n = 44) | Lesions That Grew (n = 10) | P Value |
|---|---|---|---|
| Thickness at baseline, mean (range) (mm) | 0.96 (0.5−2.3) | 1.3 (0.6−2.2) | .01 |
| Corneal touch | |||
| Absent | 39 | 6 | .007 |
| Present | 5 | 4 | |
| Surface plaque | |||
| Absent | 21 | 2 | .07 |
| Present | 23 | 8 | |
| Internal structure | |||
| Regular | 32 | 2 | .0001 |
| Irregular | 12 | 8 | |
| Linear streaks | |||
| Absent | 35 | 2 | <.0001 |
| Present | 9 | 8 | |
| Dots | |||
| Absent | 33 | 2 | <.0001 |
| Present | 11 | 8 | |
| Internal reflectivity | |||
| High | 2 | 0 | .77 |
| Medium | 36 | 8 | |
| Low | 6 | 2 |
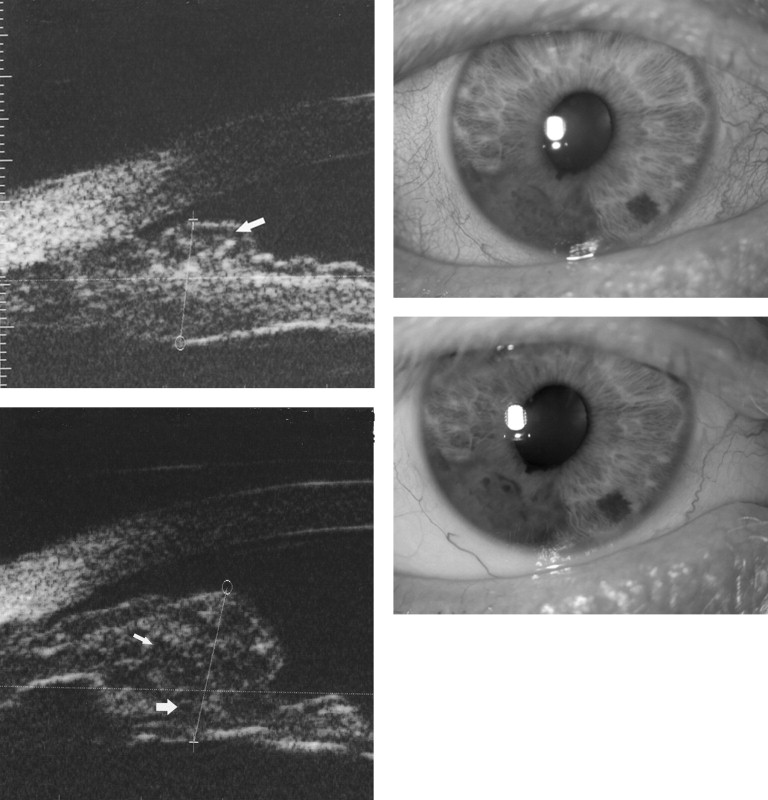
Cases With Documented Growth
Of the 44 eyes included in the study, 10 (23%) demonstrated documented growth clinically, noted by an increase in the largest basal diameter as previously defined ( Figure 1 ) . The mean follow-up period was 21.4 months (range 10−48 months) prior to the documented growth. All of these eyes had blue/green irides. The mean largest basal diameter at baseline was 5.06 mm (range 1.9−7.2 mm) for the lesions that grew, compared to 3.63 mm (range 1.1−10.3 mm) for the complete cohort ( P = .004). The mean thickness was 1.36 mm (range 0.6−2.2 mm) for the lesions that grew, compared to 0.96 (range 0.5−2.3) of the complete cohort ( P = .01).