18
Chronic Otitis Media
Peter C. Weber
This chapter discusses medical and surgical management of chronic otitis media (COM), including dry perforation, mucosal disease, cholesteatoma, surgical techniques, and surgical complications. Acute otitis media and meningeal complications of disease are covered in Chapters 17 and 19.
 Office Management
Office Management
Chronic Otitis Media Without Cholesteatoma
Tubotympanic disease as described in 1965 by Thorburn1 consists of two types.2 Type I is a chronic perforation that may occasionally drain due to colds, weather changes, or water in the ear but rarely presents significant problems to the patient. When the ear is dry the middle ear mucosa is pink, healthy, and normal (Fig. 18–1). Type II is a persistent mucosal infection. Typically the patient presents with a 3- to 6-month history of chronic discharge from the ear, which may or may not have been associated with a respiratory infection, and hearing loss (Fig. 18–2).
More than likely, the type II patient has already been treated for several months with multiple courses of systemic and topical antibiotics, and cultures have been obtained. Cultures can be helpful; however, sensitivities do not reflect that topical therapy results in concentrations much greater than those achieved by systemic antibiotics,3 and bacteria are usually known from published studies. Pseudomonas aeruginosa and Staphylococcus aureus are most common,4–7 and Escherichia coli and Streptococcus pneumoniae are less so. Foul-smelling drainage also suggests anaerobic Streptococcus or Bacteroides.8,9 Bacteroides often responds to chloramphenicol in drop or powder form, but Pseudomonas does not. Persistent drainage despite antibiotics may indicate Mycobacterium or even cerebrospinal fluid (CSF) leak.10,11 Cultures and ß2-transferrin testing are helpful in those cases.
Physical examination of the ear may demonstrate a perforation with significant granulation tissue and purulent discharge (Fig. 18–3). A high-resolution computed tomography (CT) scan usually shows middle ear soft tissue extending into the attic and often fluid within the mastoid air cells.12 I typically do not obtain a CT scan unless surgery is required (see below).
COM without cholesteatoma is distinctly different from persistent middle ear effusion requiring myringotomy and tube insertion and from a chronic draining tube requiring tube removal and antibiotics. Such treatment almost always results in a dry ear, although persistent perforation may sometimes occur. Instead, COM describes somebody who drains fluid time and again after a tube is placed then removed. The patient may have chronic eustachian tube dysfunction, chronic mucosal disease with attic block, or chronic serous mastoiditis. Many cases of COM can be traced back to an underperforming eustachian tube with effusion and drum retraction (Fig. 18–4).
Many patients with COM without cholesteatoma will need surgery; however, medical therapy should be tried first. The ear should be cleaned so that drops can reach the middle ear. Cleaning begins in the office and continues at home with irrigations of 50–50 alcohol and vinegar (essentially acetic acid). The patient repeats the washings several times daily with the ear turned up as described by Sheehy7 or turned down as preferred by others. The dropper and rubber bulb are filled with solution, the tip of the dropper is placed in the ear opening, and the bulb is compressed and decompressed gently, swishing the solution back and forth to clear the canal. The solution should be near body temperature to avoid dizziness. If acetic acid solution causes pain, Sheehy also has described using one-half strength Betadine (providine-iodine). Washings are continued for about 1 week. Steroid antibiotic drops are then added or can be started immediately after each washing.
The preferred medicated drop is a fluoroquinolone with steroid13 because it is not ototoxic and because corticosteroids can help reduce granulation tissue and edema in the middle ear as well as scaling and itching of the external canal (dexamethasone may be even better than hydrocortisone in this regard14). Rarely, a fungal infection can occur with fluoroquinolone drops. Potentially ototoxic drops (tobramycin, Cortisporin, Colimycin) have been used quite safely for decades, probably because a barrier over the round window membrane is formed by chronic disease. However, if middle ear mucosa heals with treatment but the patient continues to use ototoxic drops, they could then penetrate the inner ear and cause vestibulopathy or hearing loss. Thus, the clinician should inform the patient if a potentially ototoxic drop is to be used. However, risks are rare and if fluoroquinolones fail, it may be necessary to use these types of drops. Also, the author generally avoids Cortisporin (neomycin/polymixin/ hydrocortisone) in chronically draining ears because topical allergy to neomycin can occur and be difficult to recognize.

Figure 18–1 Near total perforation caused by “necrotizing otitis media” from ß-hemolytic streptococcus.

Figure 18–2 Chronic suppurative otitis media.

Figure 18–3 Chronic suppurative otitis media with granuloma.

Figure 18–4 Serous otitis media with retraction.
After washing, antibiotic powder may be useful. A mixture of chloramphenicol, amphotericin, and boric acid powder can be quite effective as it creates an environment that is very resistant to bacterial and fungal growth. If the patient has not had any oral antibiotic treatment prior to the first visit, I usually treat with one course. However, the topical drop is more important. Intravenous antibiotics are almost never needed unless there are complications such as petrositis, labyrinthitis, or meningitis. Surgery for COM without cholesteatoma usually is withheld until the ear is dry or maximum improvement is reached.
Cholesteatoma
Cholesteatomas grow by forming a keratinizing stratified epithelial layer and fibrous subepithelial layer called the matrix. The matrix is constantly desquamating sheets of keratin into the cholesteatoma sac. This keratin or dead skin accumulates in concentric layers. As the sac expands it erodes surrounding bone, even the hard bone of the labyrinth.
Cholesteatoma can be congenital or acquired. Congenital cholesteatomas almost always are seen in children, although adults may present with petrous apex or intracranial epidermoids. By definition, congenital cholesteatomas have no history of perforation, myringotomy, or otorrhea and have a normal tympanic membrane.15–19 The vast majority are found in the anterior-superior quadrant, although at times they may be found in the posterior-superior quadrant, within the tympanic membrane (TM) itself, or in the petrous apex. The pathogenesis of congenital cholesteatoma is controversial, although most theories have some merit: fetal epithelial cells are trapped in the middle ear; inflamed tympanic membrane cells invaginate into the middle ear; squamous metaplasia transforms middle ear mucosa into keratinizing epithelium.17
Acquired cholesteatoma is far more common than congenital, and usually results from retraction of the TM in the pars flaccida or posterior-superior quadrant (Figs. 18–5 through 18–7). This slowly occurs and may not be detected until the patient complains of drainage or hearing loss. Previous ear surgery or drum perforation may also be a site for acquired cholesteatoma as keratin can invaginate and proliferate on the undersurface of the perforation. Usually, however, epithelium from the lateral tympanic membrane, which goes around the edge of a perforation, stops growing 1–2 mm on the medial surface, where it abuts the mucosal layer.
Diagnosis of cholesteatoma is usually not difficult, as both congenital and acquired types usually can be seen on microscopic examination in the office. Patients with acquired disease usually complain of foul-smelling discharge and often bleeding. Normally, hearing is down and this can be verified with audiometric studies. Patients may have slight otalgia or headache and occasionally mild dizziness. Diseased mucosa, granulation tissue, and keratin debris may be confined to the epitympanum. Occasionally, drainage and granulation tissue can make it difficult to see the keratin sac (Fig. 18–3; also see Chapter 16, Fig. 16–8).

Figure 18–5 Cholesteatoma behind posterior drum.

Figure 18–6 Chronic otitis media with pars flaccida defect.
Cholesteatoma is a surgical disease, but again antibioticsteroid drops should be started to decrease the inflammation and granulation tissue prior to surgery. Although medical treatment will not cure cholesteatoma, it can decrease bleeding during surgery. Cholesteatoma still must be removed to obtain a safe, dry ear.
Although one could obtain culture and sensitivity studies, the most likely organisms are pseudomonas or a bacillus, and culture results do not alter the treatment. Culture and sensitivities often are obtained if a complication is suspected (see Chapter 19). Many otologists do not obtain CT scans of the temporal bones for cholesteatoma surgery, but I usually do to identify possible erosion of the tegmen, facial nerve dehiscence, and labyrinth fistula so that the patient may be better informed about the potential risks of surgery. The patient should know that cholesteatoma can cause not only hearing loss but also facial paralysis, dizziness, meningitis, and other intracranial complications.

 Surgical Management
Surgical Management
Whether treating chronic mucosal disease, cholesteatoma, or benign perforation, the surgeon’s primary goal is to obtain a safe, dry ear. The approach and technique vary depending on training and experience. However, basic principles apply to all procedures to achieve a good result. These principles and the author’s preferences are presented.
Preoperative Counseling
Patients should understand that a safe, dry ear is the primary goal of surgery so they do not have unrealistic expectations such as perfect hearing. Indeed, the treatment plan often requires two staged procedures and hearing will temporarily be worse because ossicular reconstruction often is delayed until the second step. Even without cholesteatoma, attic mucosal disease often requires incus removal; failure to do so may not completely eradicate disease or restore ventilation. Free flow of irrigant from the mastoid into the middle ear is a good indication that disease has been removed and aeration is adequate. The author performs second-look surgery with ossicular reconstruction 6 to 12 months after the first stage (see below). The patient should realize that hearing in the operated ear will not be perfect despite reconstruction, but optimally it will be better. The patient may wish to use amplification after repair.
Indications, risks, benefits, alternatives, and personnel are discussed. The success rate for a safe, dry ear is roughly 90%.20 Risks include but are not limited to partial or total hearing loss (which can occur 1–2% of the time), vertigo, disequilibrium, facial nerve paralysis, CSF leak, tinnitus, infection, bleeding, meningitis, perilymph fistula, otorrhea, stenosis/fistulization of the external auditory canal, pain, headaches, cosmetic deformities, loss of taste, and visual changes, all of which occur very infrequently.
Underlying sinonasal disease should be treated prior to ear surgery to improve postoperative eustachian tube function. Even if the eustachian tube is not blocked by sinonasal disease, its function is improved anyway by removing disease from the protympanum.
Terminology
Glasscock’s group20–23 well described the history of ear surgery. In chronic ear surgery, residual cholesteatoma refers to disease that is intentionally or unintentionally left behind after surgery, and recurrent cholesteatoma refers to that which forms in a postoperative retraction pocket.
Although many clinicians define tympanoplasty as closure of a TM perforation, it is really an operation that removes middle ear disease and reconstructs hearing with or without TM grafting. Tympanoplasty may be performed with or without mastoidectomy. Medial (underlay) grafting with temporalis fascia (or areolar tissue) was first performed by Storrs24 in 1961 in the United States and remains one of the most common techniques. Prior to this, early techniques employed a small rubber disk attached to a silver wire by Toynbee25 in 1853, skin grafts by Berthhold26 in 1878, and paper patch 10 years later.27 In the 1950s Wullstein28 and Zollner29 used split- and full-thickness skin grafts to repair chronically diseased ears, not just drum perforations, for better healing and hearing, and in 1967 Goodhill30 first described using tragal cartilage for attic reconstruction to minimize recurrent cholesteatoma. Approaches for repair include transcanal, Lempert incision, and postauricular31 procedures.
Atticotomy is appropriate for disease lateral to the incus body and malleus head, which does not extend anterior to the head of the malleus, posterior to the short process of the incus, or medial to either. It involves removal of the scutum to expose the attic tympanum. By removing this medial portion of the lateral epitympanic wall, the posterior external auditory canal wall is preserved, allowing removal of cholesteatoma confined to the epitympanum, repair of an attic retraction pocket, or gaining exposure for stapedectomy or lateral chain fixation procedures. Once disease is removed, reconstruction of the scutal wall is important to prevent recurrence of disease32 (see Tympanoplasty, later in chapter). Cartilage obtained from the tragus or cymba can be used to reconstruct the scutum (Fig. 18–8).
Cortical (simple) mastoidectomy removes the lateral aspect of mastoid bone with exposure of the middle fossa tegmen, sigmoid sinus, and antrum. Opening the facial recess can be performed if desired. This procedure is the workhorse for many ear surgeries in that it provides ventilation from the middle ear to the mastoid, eradicates disease, and provides exposure for many procedures including endolymphatic sac surgery, labyrinthectomy, and cochlear implantation. Intact canal wall tympanoplasty with mastoidectomy was first described by Jansen33 in the 1950s, a dramatic improvement over techniques and instrumentation34–37 since the first recorded mastoidectomy by Jean Louis Petit in 177438 in Paris.

Figure 18–8 Cartilage is evident in the posterior-superior quadrant after tympanoplasty.
Although surgeons prefer to keep the posterior canal wall up, indications to take it down include extensive disease, residual epithelium over a labyrinthine fistula, recurrent attic cholesteatoma, and patient inability to come for follow-up or unwillingness to undergo two-staged procedures. Removing the lateral attic wall minimizes the chance of recurrent attic disease.39 Recently, Gantz et al40 described a procedure of removing the canal wall, eradicating disease, and then replacing the canal wall.
The Bondy41 modified radical mastoidectomy, first performed in 1910, is rarely used today for attic cholesteatoma. The medial wall of the cholesteatoma sac is preserved over the intact TM and ossicular chain. Most otologists instead completely remove disease using an intact canal wall technique with second-stage ossicular reconstruction.
Radical mastoidectomy differs from modified radical mastoidectomy in that the TM is not grafted, that is, the middle ear space is not reconstructed and the eustachian tube is obliterated. The posterior canal wall is removed and meatoplasty performed. A radical mastoidectomy usually is performed in revision cases when disease (usually cholesteatoma) is so extensive that it cannot be completely removed.
Preoperative Preparation, Anesthesia, and Incisions
The operating theater is set up with the anesthesiologist at the foot of the patient and the scrub nurse directly opposite the surgeon so that instruments can be easily passed back and forth while working under the microscope. I prefer using general anesthesia for all patients, although transcanal surgery can easily be done under local anesthesia or monitored anesthesia care (MAC). The postauricular incision site is injected with 1% lidocaine–1/100,000 epinephrine, although other concentrations can be used. I do not shave any of the patient’s hair whatsoever on any otologic surgery, including chronic ear, skull base, and craniotomy surgery. Studies have indicated that the rate of infection is certainly no worse and may indeed be less than if one does shave the patient.42 The ear canal is injected with 1% lidocaine–1/40,000 epinephrine. The actual concentration of epinephrine for vasoconstriction may not matter significantly. Lidocaine does decrease some of the pain, and the patient does not have to be quite as deep in anesthesia. To monitor the facial nerve, I do not allow patients to be paralyzed for the procedure. However, a short-acting paralytic agent can be used for endotracheal intubation. Also, if a medial graft tympanoplasty is performed and the middle ear is packed with Gelfoam, nitrous oxide can be used because any lateral pressure will better adhere the graft to the undersurface of the tympanic membrane. However, for lateral graft tympanoplasty even with packing the middle ear, nitrous oxide should not be used because it may increase graft lateralization or blunting. I recommend extubation at the end of the procedure while the patient is “deep” to avoid an increase in middle ear pressure. Postoperatively, an anti-nauseant can be used to minimize straining.
After prepping with iodinated solution (Betadine), the microscope is used to make vascular strip and tympanomeatal incisions (Fig. 18–9). For transcanal work, a tympanomeatal flap incision is used (Fig. 18–10). Under direct vision the postauricular incision is then made (Fig. 18–11) a few millimeters behind the crease, which makes closure more cosmetic. A temporalis areolar tissue graft is harvested, saving fascia for revision should it be needed. A Palva flap is then raised (Fig. 18–12) by making cuts along the tegmen tympani line and mastoid tip, then connected posteriorly to create a rectangle of tissue. Many surgeons instead use a T incision; however, the Palva flap helps fill in a mastoid defect, especially in CWD surgery, and decreases caving in or cosmetic deformity postauricularly. Alternatively, if one is doing a lateral graft tympanoplasty without mastoidectomy, then a small curved linear incision just posterior to the external auditory canal may be made because no drilling will occur in the mastoid area.
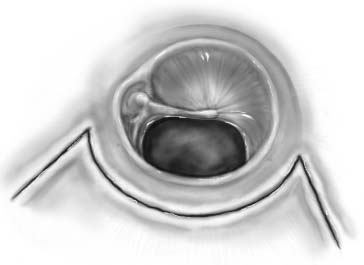
Figure 18–9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


