26 (Central) Auditory Processing Disorders
We hear with our brain! Of course, our sensory organ for audition, the ear, plays an important role in the transduction of sound to a neural signal. There is also a considerable processing of the main properties of sound (intensity, frequency, and temporal cues) before the neural signal reaches the central auditory nervous system (CANS). However, auditory processing essential for meaningful hearing and everyday communication takes place along the pathways and within the centers of the auditory brainstem and cortex. Examples of auditory processes include auditory discrimination, auditory pattern recognition, temporal (timing) aspects of audition, temporal ordering, auditory performance in competing acoustic signals (e.g., noise), and auditory performance with degraded acoustic signals.
Role of the Central Auditory Nervous System in Hearing
Hearing versus Hearing Sensitivity
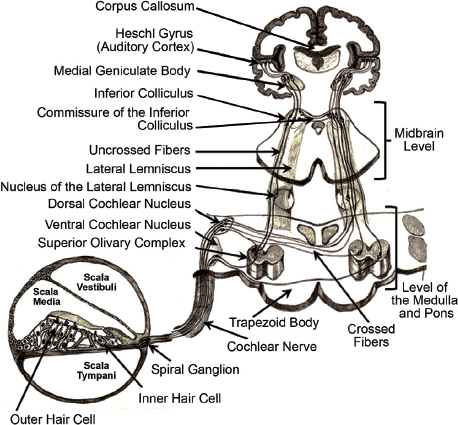
A discussion of the functional anatomy of the CANS is far beyond the scope of this chapter. (Auditory system anatomy and physiology is reviewed in Chapter 4 “Physiology of Hearing.”) We will provide a brief overview here. The major structures within the ascending auditory pathways are shown schematically in Fig. 26.1. Of course, no drawing or diagram can capture the remarkable anatomic and, especially, physiologic complexity of the auditory nervous system (ANS). Behavioral and electrophysiological auditory procedures are now available for clinical evaluation of the full extent of the auditory system depicted in Fig. 26.1. Clinical assessment of the CANS is enhanced by an appreciation of at least four principles. First, tonotopic organization (representation of frequency specialization) is maintained throughout the system, from the cochlea to the primary auditory cortex. Second, the number of neurons increases dramatically from the cranial nerve VIII (auditory) (approximately 30,000 neurons) to the auditory cortex (over 10 million neurons). Third, and related to the number of neurons, there is remarkable redundancy in the CANS, as evidenced by the multiple pathways crossing from one side to the other. And finally, the CANS is characterized by plasticity, that is, the capacity for change and restoration of function following an insult.
Even though comprehensive evaluation of hearing should include an assessment of auditory processing and CANS function, audiologists and otolaryngologists typically focus almost exclusively on estimating hearing sensitivity. It would be useful here to distinguish between the terms hearing versus hearing sensitivity. Hearing sensitivity is measured with pure tone audiometry. Reports of hearing assessment, based on an audiogram, often included a statement such as “pure tone thresholds were within normal limits consistent with normal hearing.” A claim of normal hearing based on a normal audiogram is not justified, and is misleading. Persons with normal findings on pure tone audiometry may have normal hearing sensitivity, but a normal audiogram does not necessarily reflect normal hearing. Used properly, the phrase normal hearing implies entirely normal auditory processing at all levels of the auditory system, including the highest regions of the cortex and for even complex and demanding auditory tasks. Pure tone audiometry is a very basic form of auditory processing requiring only the detection of a simple rather long-duration sound. Normal hearing thresholds have no value in describing performance on complex auditory processing tasks involved in hearing. Persons with normal hearing sensitivity and with normal cochlear function can, and sometimes do, have major hearing problems associated with very poor speech perception that produce serious hearing handicap and disability. It is critical for audiologists and otolaryngologists to go beyond the audiogram in evaluating hearing status of patients with auditory complaints, particularly when the patient is at risk for CANS dysfunction, either by history or by medical or by audiologic test findings.
Neuroscience of Central Auditory Processing
Since the 1990s, the “decade of the brain,” basic neuroscience research has generated progressively greater evidence in support of the nature and anatomic origins of (central) auditory processing disorders (C) APDs, sometimes referred to as simply APD. Hundreds of published papers reported clinical investigations employing neuroanatomic techniques, such as functional magnetic resonance imaging (fMRI) and cortical auditory-evoked responses, have unequivocally documented neuroanatomical and neurophysiological correlates of auditory processing and related disorders. Research in auditory neuroscience has also described the neural representation of speech perception, and established the neural link between auditory processing and reading. And, importantly, formal clinical research has shown that intensive intervention for APDs can improve the speed and efficiency of auditory processing, with secondary benefits on related disorders (e.g., reading). The work of Kraus and colleagues at Northwestern University during the past 15 years provides an excellent example of the innovative applied research, that is, helping to explain APDs, and how they can be remediated.1–5
Audiologists and otolaryngologists can quickly and easily document the rather voluminous auditory neuroscience literature by conducting via the Internet a Medline search for health professionals at the Web site www.nlm.nih.gov, using relevant keywords such as “auditory,” “auditory processing,” “fMRI,” “auditory-evoked responses,” and many others. Support for the scientific legitimacy and the neuroscience bases of APDs or (C) APD is also evident by the allocation of resources of professional organizations for task forces charged with the development of technical statements6 and evidence-based clinical guidelines for assessment and management of (C) APDs.7
Definition of (Central) Auditory Processing Disorders
We will interchangeably use the terms APD and (C) APD in our review reflecting the usage of terminology in contemporary literature on the subject. One of simplest, yet most clinically useful, definitions of APD was developed in 2000 at a conference organized by Jerger: “APD is broadly defined as a deficit in the processing of information that is specific to the auditory modality.”8 Readers will notice that this definition does not limit auditory processing to the CANS. Deficits in auditory processing can occur anywhere along the auditory pathways, and even in multiple regions. Indeed, deficits in one region of the auditory system can interact in dynamic ways with function in another region. Taking a clinical perspective, severe peripheral hearing loss in children may impact the development of normal central auditory processing. Conversely, elderly individuals with a modest degree of peripheral hearing loss will experience considerably greater impairment if they also have ineffective and/or inefficient central auditory processing, for example, difficulty with hearing in noise. Another important component of the 2000 definition of APD is the requirement that the disorder be auditory specific. Some coexisting disorders, such as cognitive abnormalities, language impairments, and attention deficits, may masquerade as APDs. The diagnosis of APD, however, requires documentation of a deficit specific to the auditory system. Of course, the same patient may also be diagnosed with one or more of the other problems.
Definitions of auditory processing are also available from two comprehensive evidence-based documents that are readily available via the Internet. A task force commissioned by the American Speech-Language-Hearing Association (ASHA) developed in 2005, a peer-reviewed technical statement on APD (see APD link at the Web site www.asha.org). The ASHA referred to (C) APD as “the efficiency and effectiveness by which the central nervous system utilizes auditory information.”6 How does this definition help to identify patients with possible APD? In the clinical setting, you will encounter patients who at first appear to be communicating effectively. Close questioning and clinical observation, however, reveals that the patient is struggling to hear in most settings, and unable to effectively communicate in demanding listening conditions. For example, the patient reports inability to carry on a conversation in a noisy restaurant, or with a person who is speaking rapidly, or with a person who has a distinct foreign dialect.
We strongly recommend that readers with an interest in auditory processing and APD review closely another very up-to-date peer-reviewed and evidence-based document: the Guidelines for the Diagnosis, Treatment, and Management of Children and Adults with Central Auditory Processing Disorder. It was prepared in 2010 by a task force of experts at the request of the American Academy of Audiology (AAA),7 and is available to all at the organization’s Web site: www.audiology.org. The guidelines expand on the ASHA 2005 definition of APD by stating: “(C) APD is seen in a wide array of populations, including children and adults. It can be the result of a number of different etiologies that involve deficits in the function of the central auditory nervous system. Neurological involvement ranging from degenerative diseases to exposure to neurotoxic substances can result in (C) APD.”7
Test Battery for (Central) Auditory Processing Assessment
The intrinsic redundancy in the CANS, as a result of convergence and divergence of neural networks, enables complex auditory functioning, but also poses significant challenges for clinical identification and diagnosis of (C) APD. Multiple information pathways enable basic auditory functions to remain intact in persons with clinically documented (C) APD. Two important concepts clearly explain the reasons why audiological assessment of (C) APD is complex and necessitates specially designed tests. They are the subtlety and bottleneck principles put forth by Jerger.9 According to the subtlety principle, “the subtlety of the auditory manifestation increases as the site of lesion progresses from peripheral to central.”9 Stated differently, the more peripheral a lesion the more easily it is detected on basic audiological tests.
(C) APD often remains undetected on a routine audiological test battery consisting of a combination of pure tone audiometry, basic speech audiometry (e.g., word recognition in quiet), and tympanometry. Dysfunction within the auditory brainstem and more rostral regions of the CANS may be found in patients with normal peripheral hearing sensitivity.10,11 A rare exception is the patient with bilateral lesions of the auditory cortex (often involving the subcortex or brainstem) that result in central deafness, manifesting as severe to profound hearing loss on a pure tone audiogram.11,12 Thus, to reiterate a point we made already, normal hearing sensitivity on an audiogram does not imply a normally functioning CANS or normal hearing.
Jerger’s bottleneck principle makes it clear why conventional speech audiometry would also dysfunction rostral to the lower brainstem. According to this concept, “… the process of transmitting the informational content of a complex auditory stimulus (i.e., speech) encounters a very real bottleneck in the eighth nerve and lower brain stem. Lesions at these sites limit the ability to understand speech drastically.”9 Lesions in the higher brainstem and beyond typically do not affect speech recognition in quiet because of the ease of this task, which results from a combination of intrinsic redundancy in the auditory neural pathways, as well as the linguistic and acoustic cues within the speech stimulus. Hence, normal findings might be obtained on basic speech audiometry, including procedures such as speech detection threshold, speech recognition threshold, and word recognition score at a single intensity level. (Note: Diagnostic audiometry procedures and protocols are reviewed in chapter “Comprehensive Diagnostic Audiology.”) If the site of dysfunction is rostral to the superior olivary complex, it would not be detected even on acoustic reflex testing, because the neural tracts and nuclei underlying this reflex are more caudal. (C) APD can affect both children and adults.13 While children are generally not able to report their auditory problems, even adults may find it difficult to describe the exact nature of their auditory problems. Typical complaints may be, “I am fine when the room is quiet but I just cannot understand anything if it is noisy;” “I find it tough to learn even the simplest tunes;” “I often get confused on where a sound is coming from.” Unless a specific (C) APD test battery is administered in such cases, auditory dysfunction will go undiagnosed or will be confused with functional hearing loss (e.g., malingering). The key issue for an audiologist or otologist is to know when to limit testing to a basic audiological assessment and when to refer for a (C) APD evaluation. A thorough patient history, and reliance on risk factors, are helpful in determining which patients require formal and comprehensive assessment for (C) APD.
Risk Factors for (Central) Auditory Processing Disorders
Constraints on clinical time and resources preclude routine comprehensive assessment of auditory processing in every patient presenting with hearing complaints. Hearing loss encountered clinically is commonly because of peripheral auditory dysfunction involving either the middle ear or the cochlea. Hearing loss can often be adequately documented with an audiogram supplemented with objective procedures that are highly sensitive to middle ear dysfunction (acoustic immittance) or outer hair cell dysfunction within the cochlea (otoacoustic emissions [OAEs]). We describe these and other diagnostic auditory procedures in chapter “Comprehensive Diagnostic Audiology.”
Patients at risk for CANS dysfunction and related APDs can be identified by systematic application of a series of indicators, summarized for children and adults in Table 26.1. Children who are performing poorly in school with no obvious explanation, especially those described as poor listeners, are at considerable risk for auditory processing deficits. Any insult to the nervous system, beginning in the perinatal period, increases the chance of possible CANS dysfunction. Consistent reliance on risk factors will contribute to early identification, accurate diagnosis, and appropriate management of APDs in children. For the adult population, one of the most important risk factors is patient difficulty with listening and communication that is greater than anticipated from their audiogram. This includes poor performance with appropriate amplification. A history of traumatic brain injury is high on the list of risk indicators for APD.
Children • Poor academic performance • Diagnosis of coexisting disorders, e.g.,
• Neurologic disorders, e.g.,
• Chronic otitis media with associated conductive hearing loss • Head injury • Perinatal history of neurological insult or risk
Adults • Aging • Head injury, including traumatic brain injury • Listening problems greater than expected from the audiogram • Poor benefit from amplification of peripheral hearing loss • Dementia and other neuropsychiatric diseases, e.g.,
|
• Inappropriate or inconsistent responses to questions especially those asked without visual or contextual cues.
• Patient is described as a “poor listener.”
• Frequent requests for repetition of orally presented information.
• Difficulty in listening over the telephone.
• Inattention, boredom, and avoidance of tasks involving listening.
• Difficulty in comprehending speech in adverse listening environments (e.g., noisy or reverberant surroundings, multiple talkers, unfamiliar talkers, and groups).
• Difficulty in understanding fast rates of speech.
• Difficulty in remembering auditory instructions, especially if they are long or complex, with no comparable problems with written instructions.
• Tendency to mix up similar sounding words, for example, pest versus pets.
• Difficulty in localizing sounds.
• Poor musical ability, poor prosody in speech (monotonous voice), inability to recognize simple sound patterns or rhythms, difficulty in learning nursery rhymes or songs that are easily learned by peers.
• Difficulty in comprehending suprasegmental aspects of speech, such as differences in pausing or emphasis (“Can’t you go tomorrow?” with emphasis on “you” versus “Can’t you go tomorrow?” with emphasis on “tomorrow”) that can change the meaning of an utterance.
• Difficulty in academics (reading, writing, and spelling), learning problems.
Some of the above signs and symptoms are commonly reported by patients with peripheral hearing loss. The important distinguishing feature in individuals with (C) APD is that the symptoms exist even when pure tone audiometry has confirmed normal hearing sensitivity. Thus, the importance of ruling out hearing loss before undertaking (C) APD assessment cannot be overemphasized. A routine audiological test battery to eliminate or quantify peripheral hearing loss is mandatory. (C) APD can however, coexist with hearing loss or several other conditions with overlapping symptoms. Isolating the effects of (C) APD from those of a peripheral hearing loss is possible but warrants extreme caution as described further in this review.
Before the commencement of formal testing, a thorough case history is necessary which should probe the following areas7,14:
• Family history of auditory processing, learning, or hearing problems.
• Prenatal, perinatal, and postnatal medical history, which should include otological and neurological aspects.
• History of motor development, speech, and language milestones.
• General behavior, socialization, and relationship with peers.
• Auditory behavior (based on previously described signs/symptoms) and communication problems faced by the individual.
• Educational history and details of performance/work history.
• Language and cultural background.
Musiek, Baran, and Pinheiro describe three types of (C) APD: “cases with neurological disorder, neuromaturational lag, and cerebral morphological abnormalities.”11 The first type includes individuals who have a definite neurological base to their (C) APD, for example, tumors, demyelinating disease, epilepsy, cerebrovascular accident, sectioned corpus callosum, and lesions secondary to trauma. While neurological disorders are comparatively less common in children, they must be considered when signs and symptoms indicate the need for (C) APD assessment.13 The second type includes those who manifest characteristics of (C) APD in early childhood because of delayed neurological maturation, and eventually achieve age-appropriate levels of auditory processing ability. Such children may show remarkable improvement in auditory processing skills in short time periods, a feature that is not seen when there is a neurological base to the (C) APD.11 The third type includes individuals whose (C) APD has a morphological basis which means that the structure (and therefore function) of certain brain areas is abnormal. Such abnormalities have been reported in children and adults with learning disabilities,15–17 attention deficit hyperactivity disorder,15,18 and even stuttering.19–21 Earlier studies on brain morphology (e.g., Galaburda and colleagues17) were conducted posthumously. Recent trends in structural and functional neuroimaging have increasingly enabled longitudinal and cross-sectional studies in various age groups and clinical populations.
Any single central auditory process among those listed in the introductory paragraph of this chapter (and also, described in the AAA guidelines7) may be functionally independent of others. In other words, a patient may exhibit an abnormality with one auditory process in isolation, with normal performance on other auditory processing tasks. There is no single best test or gold standard test for (C) APD assessment.13 The literature6,7,22,23 consistently supports a test battery approach. According to the AAA guidelines,7 the sensitivity of (C) APD assessment increases when a combination of tests is used. It is important to use tests that have normative data for the specific age group, clear cutoffs for normal scores, and preferably data on reliability, sensitivity, and specificity. The guidelines also articulate clear goals of assessment: (1) to identify the presence of abnormalities in or dysfunction of the CANS and diagnose (C) APD, and (2) to describe the nature and extent of the disorder for purposes of developing management and intervention programs for affected individuals.7 The ASHA6 position statement recommends a combination of tests such that each auditory process is represented by at least one test. As speech and nonspeech sounds are processed in different areas of the brain, a combination of tests using speech and nonspeech stimuli is also recommended. The most common categories of tests, with examples of versions available in English, their application to (C) APD assessment, and results in clinical populations, are described in the following section on “Behavioral Tests.” A detailed review of all available tests is beyond the scope of this chapter. The interested reader is referred to some recent excellent references for additional information.22,24 Interpretation of test battery findings is discussed after the description of individual tests.
Behavioral Tests
Behavioral tests, also known as subjective tests, require a motivated, alert, and cooperative patient who is willingly to make an effort to give a response to the stimulus. A common criticism25 of behavioral tests of (C) APD is dependence on not only auditory skills, but also nonauditory abilities such as cognition, attention, memory, and language comprehension. Although nonauditory factors play a role in behavioral test performance, a multidisciplinary approach to assessment can eliminate confounding effects in the diagnosis of (C) APD. Despite the advent of electrophysiological tests of hearing and sophisticated neuroimaging techniques, behavioral tests of (C) APD continue to be of great clinical importance. Behavioral procedures, especially those involving speech stimuli, have greater face validity in assessing the ability to function in different types of difficult listening environments. It is perhaps stating the obvious to reiterate that the negative impact of APDs on normal communication arises mostly from difficulty with speech perception. Because of a vast range of possible manipulations in test stimuli, behavioral tests can assess a wide range of central auditory skills.
Various types of nonspeech stimuli (e.g., clicks, noise, tones, and tone bursts) and speech stimuli (e.g., nonsense syllables, monosyllabic words, spondees, natural sentences, synthetic sentences, and digits) can be used in (C) APD assessment. The difficulty level of a test can be increased or decreased by manipulating the redundancy or other test conditions (e.g., introduction of background noise or a competing message). Linguistic redundancy is an important aspect of a speech stimulus that determines accuracy and ease of identification. This term refers to the background linguistic knowledge that helps the listener to predict the stimulus from available speech cues. Speech stimuli become increasingly intelligible, and therefore easier to recognize, as the meaningful (linguistic) information contained in them increases.26 Natural sentences, compared with single words, provide greater opportunity for the listener to use linguistic content for recognition.14 Linguistic redundancy is especially important in recognizing a speech stimulus, that is, not clearly audible or is made difficult to perceive in some way. The CANS relies on a combination of top-down skills (e.g., cognitive and linguistic) and bottom-up skills (e.g., auditory perception) in processing speech stimuli. As a result, the linguistic redundancy of a particular speech stimulus is an important consideration that determines performance for a particular presentation condition.
Response mode is another variable in (C) APD assessment. Responses can be verbal or nonverbal. They can also be within a closed set task (involving choice from a limited set of possible responses) or an open set task (any response is possible). Over the years, the focus in the clinical application of (C) APD tests has shifted from attempting to determine the site of lesion to the diagnosis of functional deficits in auditory processing, a more generalized (C) APD.7,27 Behavioral tests are now most often used to assess auditory processing in populations that do not have accompanying neurologic disorders. However, investigations involving individuals with confirmed brain lesions continue to be an important strategy for validating (C) APD tests.7
Tests of Dichotic Listening
The term dichotic listening refers to a situation in which similar stimuli (e.g., two syllable words or sentences) are presented simultaneously to both ears, but the stimulus is different in each ear. The concept of testing dichotic listening was first introduced by Broadbent.28 However, Kimura is credited with the first series of comprehensive clinical studies on dichotic listening29–32 that resulted in a permanent place for these paradigms in (C) APD assessment. Kimura noted that “each ear has connections with the auditory receiving area in each hemisphere, but the pathways connecting the ears to their opposite hemispheres are apparently more effective than the ipsilateral pathways.”32 The ipsilateral pathways are temporarily “suppressed” during dichotic stimulation,29,30 thus forcing the auditory system to rely mostly on the contralateral pathways. In a dichotic listening paradigm, the left ear has access to the left hemisphere only through an “indirect pathway,” that is, information from the left ear travels first to the right temporal cortex and then on to the left auditory cortex through the corpus callosum (Fig. 26.2). The same is true for access of the right ear to the right temporal cortex. However, importantly, information presented to the right ear has direct access to the typically language-dominant left temporal cortex. In dichotic tests with speech stimuli, scores for the right ear, which is contralateral to the language dominant (usually left) hemisphere, are typically higher. This phenomenon is called the right ear advantage (REA). A left ear advantage may be observed for nonverbal stimuli, such as musical notes and rhythms, owing to the dominance of the right temporal lobe for such tasks.33 The REA is not observed for monaural presentation of speech stimuli. It is only typical of difficult listening paradigms such as dichotic presentation. Its magnitude is influenced by factors such as age and type of speech stimulus.
Tasks of dichotic listening may incorporate a variety of nonspeech (e.g., tones and melodies) or speech (e.g., nonsense syllables, consonant-vowel syllables, digits, words, natural sentences, and synthetic sentences) stimuli. There is general agreement6–8 that dichotic listening tests are an important, really mandatory, component in the clinical (C) APD test battery.
Within the past 50 years, a variety of dichotic listening tests have been introduced clinically. The dichotic digits test (DDT) is a very popular test of (C) APD. One of its prime strengths is the low linguistic complexity of the stimuli. This test uses digit-pairs as stimuli. In English, the stimuli include monosyllabic digits between 1 and 10 (7 is excluded because it has two syllables). The digits are aligned such that the onset of the digits in each ear is within 70 ms of the other ear.34 The DDT’s relative resistance to mild-moderate cochlear hearing loss is a useful feature as peripheral hearing loss can coexist with (C) APD. It is recommended by Musiek and Chermak as a first-order test for (C) APD in individuals with or without neurological lesions.35 The DDT has been successfully used with children aged 7 years and above. Age-wise normative data are mandatory for the specific test version used.
The Staggered Spondaic Word Test (SSW), first introduced by Katz,36
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Specific language impairment
Specific language impairment Attention deficit hyperactivity disorder
Attention deficit hyperactivity disorder Reading impairment
Reading impairment Seizures
Seizures Premature birth
Premature birth Asphyxia (low Apgar scores)
Asphyxia (low Apgar scores) Hyperbilirubinemia
Hyperbilirubinemia Alzheimer disease
Alzheimer disease Parkinson disease
Parkinson disease