36

Bevacizumab (Avastin)
Monica Rodriguez-Fontal  Craig M. Greven
Craig M. Greven
INTRODUCTION
Bevacizumab is a monoclonal antibody to vascular endothelial growth factor developed for the treatment of cancer. Over the past years, it has been used in the management of complicated retinal and choroidal vascular conditions like diabetic retinopathy, retinal venous occlusive disease, retinopathy of prematurity, neovascular glaucoma, and exudative age-related macular degeneration (AMD). The following chapter will address the pharmacology and pharmacokinetics of Bevacizumab and its utility in the management of ophthalmic diseases.
BACKGROUND
The idea of using antibodies that target malignant tumor cells was originally suggested by Ehrlich at the beginning of the 20th century (1). Creation of somatic hybridization to generate “hybridoma” cell lines brought this idea closer to reality in 1976. Initially the monoclonal antibodies (mAbs) failed to show efficacy in clinical trials mainly due to intrinsic immunogenicity (rodent-derived mAbs). These issues were quickly overcome by newly developed molecular antibody engineering methods that allowed humanization of antibodies. The advance in technology led investigators to develop monoclonal antibodies for specific targets. Antibodies are currently engineered to customize their size, binding specificity, affinity, effectors function, and ability to be produced on a large scale suitable for clinical use.
Bevacizumab is a humanized antibody (IgG1) designed to recognize all isoforms of a diffusible endothelial cell-specific mitogen, the vascular endothelial growth factor (VEGF) with high affinity (Kd, 0.8 nM). Bevacizumab inhibits VEGF-induced proliferation of endothelial cells and VEGF-induced vascular leakage. Angiogenesis is an essential process required for tumor growth, as well as for new vessel formation. The VEGF pathway is well established as one of the key regulators of the angiogenesis process. Elevation of VEGF was found in aqueous humor and vitreous humor in human eyes with proliferative diabetic retinopathy and other retinal disorders. VEGF was also found to be elevated in surgically extracted choroidal neovascular membranes from AMD patients (2, 3).
Bevacizumab was Food and Drug Administration (FDA) approved in 2004 for first-line therapy in combination with irinotecan, 5-fluorouracil (5-FU), and leucovorin in metastatic colorectal cancer. This approval was based in the results of a phase III trial (4), where over 800 previously untreated metastatic colon cancer patients were given bolus irinotecan, 5-FU, and leucovorin plus placebo or bevacizumab. The overall response rate was 44.8% in the bevacizumab group and 34.8% in the placebo group, with duration of response of 10.4 and 7.1 months, respectively. The median progression-free survival (PFS) was 10.55 versus 6.24 months, and median survival was 20.34 versus 15.61 months. The main toxicities in the bevacizumab group were grade 3 hypertension (11% versus 2.3%), proteinuria, and arterial thromboembolic events (4.4% vs 1.9%). In 2006, bevacizumab was approved by the FDA for second-line treatment for metastatic colon cancer in combination with intravenous 5-FU-based chemotherapy, and first-line treatment for nonsmall cell lung cancer. In February 2008, the FDA granted accelerated approval of bevacizumab in combination with paclitaxel for first-line treatment of metastatic HER2-negative breast cancer.
Bevacizumab has structural and functional similarities to another anti VEGF agent, ranibizumab. When initial clinical trial data suggested a significant benefit with ranibizumab in AMD, and with ranibizumab unavailable for use because it was awaiting licensing approval by the FDA, ophthalmologists began treating AMD and subsequently diabetic retinopathy and macular edema with bevacizumab, When ranibizumab was eventually licensed for use in America, bevacizumab was already well established in the retina community as a potentially effective and apparently safe therapy. The use of the drug for intravitreous injection increased exponentially without the evidence base that usually guides the rational and safe use of new medicines, namely large randomized controlled clinical trials. The current Comparisons of Age-Related Macular Degeneration Treatments Trials (CATT) is a randomized controlled clinical trial designed to compare the efficacy and safety of two dosing strategies of bevacizumab and ranibizumab.
BEVACIZUMAB SYNTHESIS
Bevacizumab (rhuMAb VEGF) is a recombinant humanized IgG1 antibody derived from the murine VEGF monoclonal antibody A4.6.1 (5). It is a full-length antibody of 149 kilodaltons, bigger than ranibizumab (antibody fragment of 48 kilodaltons). Bevacizumab has 93% human and 7% murine protein sequences. The humanization process of bevacizumab was performed by site-directed mutagenesis of a human framework. Several framework residues and the six complementary-determining regions were changed from human to murine. The final result was a humanized anti-VEGF F(ab), rhuMAb VEGF, agent with the same biochemical and pharmacologic properties as the parental antibody, but with reduced immunogenicity, and a longer biological half-life (5).
Bevacizumab binds and inhibits all biologically active forms of VEGF, much like ranibizumab (6). It is a full-length, humanized monoclonal antibody, whereas ranibizumab is a humanized antigen-binding fragment. Both proteins were genetically engineered from the same murine monoclonal antibody against VEGF (5). Although bevacizumab has two binding sites for VEGF, ranibizumab has only a single binding site, which has been affinity matured to have an increased binding affinity for VEGF compared with the antigen-binding fragment derived from the original murine antibody (7).
BEVACIZUMAB CHARACTERISTICS: PHARMACOKINETICS, MECHANISM OF ACTION
Intravenous Pharmacokinetics
The pharmacokinetic profile of bevacizumab administered intravenously in patients with tumors was collected in phase I to phase III trials (8). Pharmacokinetics were assessed after analyzing 491 patients (a total of 4,629 bevacizumab concentrations) who received 1 to 20 mg/kg of bevacizumab weekly, every 2 weeks, or every 3 weeks (9). The estimated half-life of bevacizumab was approximately 20 days (range 11 to 50 days). The predicted time to reach a steady state was 100 days. The accumulation ratio following a dose of 10 mg/kg of bevacizumab every 2 weeks was 2.8. The clearance of bevacizumab varied by body weight, by gender, and by tumor burden. After correcting for body weight, males had a higher bevacizumab clearance (0.262 L/day vs. 0.207 L/day) and a larger Vc (3.25 L vs. 2.66 L) than females. Clearance was 26% faster in men than in women. Patients with higher tumor burden had a higher clearance (0.249 L/day vs. 0.199 L/day) than patients with tumor burdens below the median.
Intravitreal Pharmacokinetics: Animal Models
Bakri et al. (10) published the first intravitreal pharmacokinetic study. They used a rabbit model to analyze the pharmacokinetics of 1.25 mg of intravitreal bevacizumab. They found that vitreous concentrations of bevacizumab reach a peak concentration of 400μg/mL 1 day after intravitreal injection and declined in a monoexponential fashion with a half-life of 4.32 days. Concentrations of >10μg/mL bevacizumab were maintained in the vitreous humor for 30 days. Bevacizumab concentrations in the aqueous humor of the injected eye reached a peak concentration of 37.7μg/mL 3 days after drug administration. Serum concentrations were low; a maximum serum concentration of 3.3μg/mL was achieved 8 days after intravitreal injection and the concentration fell 29 days after injection. Elimination of bevacizumab from aqueous humor and serum paralleled elimination found in vitreous humor, with half-life values of 4.88 days and 6.86 days, respectively.
Bakri also detected very low concentrations of bevacizumab in the fellow uninjected eye (0.35 ng/mL at 1 day to 11.17 ng/mL at 4 weeks). Concentrations of bevacizumab in aqueous humor of the fellow eye reached their peak at 1 week and declined to 4.56 ng/ml at 4 weeks.
Ranibizumab pharmacokinetics were analyzed using the same rabbit model (11). After injecting 0.5 mg of intravitreal ranibizumab into rabbit eye, the half-life in vitreous was 2.88 days (compared 4.32 days of bevacizumab). No ranibizumab concentration was detected in the serum or in the fellow eye.
Intravitreal Pharmacokinetics: Human Eyes
Csaky and associates (12) report a half-life of 10 days in vitreous samples of 18 patients after injection of 1.25 mg of bevacizumab. In accordance with these results Krohne et al. (13) found a half-life of 9.82 days after analyzing aqueous humor sample of 30 eyes that received 1.5 mg bevacizumab. In the Csaky study, bevacizumab concentrations in vitreous are reported to reach peak values of 80 to 170μg/mL. Krohne showed that concentration of the drug in aqueous humor peaked on the first day after injection with a mean concentration of 33.3μg/mL and declined in monoexponential fashion. The higher concentrations in vitreous compared with aqueous humor measurements are to be expected considering the intravitreal delivery of the drug.
Zhu et al. (14) found a relatively lower half-life (6.7 days) after analyzing vitreous samples of 11 patients with choroidal neovascularization injected with 1.25 mg of bevacizumab. The investigators showed a peak concentration of the drug 2 days after injection, and a minimum concentration to completely block the VEGF-A-induced endothelial cell proliferation (>500 ng/mL) for 48 days. They also investigated the relationship between intravitreal bevacizumab and vitreous VEGF-A. Free VEGF-A levels in the vitreous ranged from 0.2 to 33.9 pg/mL and showed a negative correlation with the bevacizumab concentration, confirming in vivo binding affinity of bevacizumab to VEGF-A.
PENETRATION THOUGH THE RETINAL LAYERS
Assays in cynomolgus monkeys (15) and albino rabbits (16) showed that bevacizumab penetrated inner layers of the retina on the first day of injection and reached the choroid during the following days. An active transport mechanism is probably involved in the process.
Retina Toxicity
Safety of intravitreal bevacizumab was evaluated in several animal assays and in vitro studies. Electroretinograms performed after various doses of bevacizumab injections in rabbits show no retinal toxicity, with no alterations in scotopic and photopic a-wave and b-wave amplitude. No histopathology changes or toxicity to the cells were noted (16–20).
Mechanism of Action
Bevacizumab binds to the receptor-binding site of active forms of VEGF-A, including the biologically active (cleaved form of this molecule) VEGF110. With the binding of bevacizumab to VEGF-A, the interaction of this molecule with its receptors (Flt-1 [VEGFR-1] and KDR [VEGFR-2]) on the surface of endothelial cells reduces endothelial cell proliferation, vascular leakage, and new blood vessel formation (21).
VEGF inhibition generates ultrastructural changes in blood vessels. Some of these alterations explain the efficacy of bevacizumab in the treatment of macular edema and choroidal neovascularization.
Structural changes, like reduction in number of open fenestrations in blood vessels, and close-tight junctions between adjacent endothelial cells, lead to a reduction in vascular leakage and new vessel formation (22). Electron microscopic quantification demonstrated a highly significant reduction of endothelial cell fenestrations at choriocapillaris level after intravitreal injection of bevacizumab. In an animal model, blockage of the VEGF causes secondary atrophy of the choriocapillaris and results in a loss of endothelial cell fenestrations. The loss of fenestrations starts within 24 hours of bevacizumab injection into the vitreous, and regeneration of fenestrated capillaries is detected within two weeks after VEGF inhibition. Electron microscopic evaluation after intravitreal bevacizumab also demonstrated some degree of capillary blockage. Regionally altered arrangement of leukocytes, thrombocytes, and erythrocytes were found closing the capillaries lumen (22).
Moreover, in vitro studies with human umbilical vein endothelial cells incubated with bevacizumab demonstrated reduction of the number of proliferating cells, prevention of cell growth, induction of apoptosis, and, significantly, reduction of migration capacity of the cells (23). These results demonstrate that clinical doses of bevacizumab are able to prevent several steps of the angiogenic process.
CLINICAL INDICATIONS OF BEVACIZUMAB
Following FDA approval of Bevacizumab for treatment of metastatic colorectal cancer, ophthalmologists from around the world extended treatment indications. Currently, bevacizumab is being used for a variety of eye diseases that involve new vessel formation and macular edema.
The first outcomes of bevacizumab in ophthalmology were published in 2006. The encouraging results observed with intravitreal ranibizumab in the earlier phase I/II studies gave the initial impulse to investigate the systemic effect of bevacizumab in neovascular age-related macular degeneration (ARMD) patients.
SANA (Systemic Avastin for Neovascular AMD) was designed to look at the safety, efficacy, and durability of systemic bevacizumab for the treatment of neovascular ARMD. Two cohorts of 9 patients were followed for 24 consecutive weeks following intravenous administration of Bevacizumab at doses of 5 mg/Kg. Improved visual acuity with resolution of leakage from neovascular lesions was observed after 2 or 3 doses of bevacizumab (24). Mild elevation in blood pressure was the only adverse event identified. In spite of the lack of severe adverse events in this first trial, some investigators were concerned with the potential risk for uncontrolled hypertension and thromboembolic events, as had been observed in cancer patients (25, 26). With that concern in mind, and because of the pharmacologic similarity with the ranibizumab, intravitreal delivery was tested. It was assumed that, theoretically, a 400-fold lower dose of bevacizumab injected into the eye was safer for the patient than a higher dose given systemically.
Since that first publication in 2006, several studies have been done using bevacizumab for multiple retinal pathologies. New vessel formation, macular edema, choroidal neovascularization, and as an adjuvant in vitreous and glaucoma surgery have been some of the indications for bevacizumab in ophthalmology.
BEVACIZUMAB IN MACULAR EDEMA
The pathogenesis of macular edema is multifactorial and not completely understood. Disruption in the blood-retinal barrier secondary to inflammatory mediators like VEGF, prostaglandins, cytokines, and other vasopermeability factors, have been involved in the increased permeability of the perifoveal capillaries and the resulting macular edema.
Recent studies show the efficacy of an intravitreal injection of bevacizumab in reduction of pseudophakic cystoid macular edema (27), macular edema secondary to retinal venous occlusions, diabetes (28, 29), and other eye diseases like retinitis pigmentosa (30).
DIABETIC MACULAR EDEMA
The Early Treatment Diabetic Retinopathy Study (ETDRS) (31) established that focal laser photocoagulation for diabetic macular edema (DME) reduced moderate visual loss by 50%. Based on these results, laser treatment for DME has been the only well demonstrated treatment that reduces the risk of vision loss in these patients. However, in the ETDRS, 12% of treated eyes lost ≥15 ETDRS letters at a 3-year follow-up interval. Furthermore, only 3% of the laser-treated eyes gained ≥3 lines of vision. Given that most of the eyes laser-treated for DME do not experience an improvement in visual acuity, alternative management strategies like intravitreal steroids and anti-VEGF are being considered.
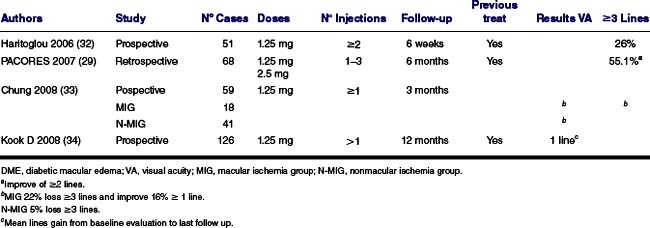
Bevacizumab has been used as a treatment for DME since 2006. Several studies have been published showing good results with this new approach (Table 36-1). It has been proposed that the use of intravitreal bevacizumab may reduce the risk of vision loss in eyes with DME by 96% (29). This risk reduction is lower when the investigators include eyes with advanced stages of DME and macular ischemia (32–34). The benefit appears evident during the first month of treatment and may continue improving for the next 6 months. Re-injections are often necessary, however, to reach maximum improvement. The optimal treatment schedule is yet to be determined but probably variable, depending on multiple factors. There is evidence that a single injection of bevacizumab lasts for 4 to 6 weeks. Deterioration of visual acuity and recurrence of macular edema are often seen again after 8 to 12 weeks (35).
Visual function recovery after bevacizumab treatment in the presence of macular ischemia is not as good as in the absence of ischemia. The foveal thickness may decrease after the injection, but this reduction does not correlate with an improvement in visual acuity (33).
A phase 2 randomized, multi-center clinical trial was conducted by the Diabetic Retinopathy Clinical Research Network (DRCR.net) at 36 clinical sites in the U.S. (36). The study was designed to provide data on the short-term effect of intravitreal bevacizumab for DME. The patients were assigned randomly to one of five groups: focal photocoagulation at baseline (N ∇ 19, Group A), intravitreal injection of 1.25 mg bevacizumab at baseline and 6 weeks (N ∇ 22, Group B), intravitreal injection of 2.5 mg bevacizumab at baseline and 6 weeks (N ∇ 24, Group C), intravitreal injection of 1.25 mg bevacizumab at baseline and sham injection at 6 weeks (N ∇ 22, Group D), or intravitreal injection of 1.25 mg bevacizumab at baseline and 6 weeks with photocoagulation at 3 weeks (N ∇ 22, Group E). Although about half of eyes demonstrated an initial positive response to intravitreal bevacizumab (exceeding an 11% reduction in retinal thickness compared with baseline at either the 3-week or 6-week visit), this response was similar to that observed in the laser group after more than 3 weeks. In addition, the magnitude of the response was not large for most subjects. Two doses of bevacizumab are being used: 1.25 mg and 2.5 mg. Both concentrations work in a similar way reducing macular edema and restoring visual acuity in DME. A combination of bevacizumab and laser photocoagulation was tested and no apparent short-term benefit or adverse outcomes were found (36). A large phase 3 randomized clinical trial is important to determine the value of bevacizumab in DME.
TABLE 36-1 BEVACIZUMAB FOR DME
MACULAR EDEMA IN VASCULAR OCCLUSIONS
Venous occlusions are the second most common retinal vascular disease after diabetic retinopathy. Vision loss in these cases is associated with macular edema and macular ischemia. Laser photocoagulation has been the only evidence-based treatment for patients with macular edema secondary to branch vein occlusions (BRVO) since 1984 when the BRVO Study (37) was published. The BRVO study showed that 63% of laser treated patients had improved ≥2 lines of vision compare with 36% of the control eyes with a mean gain in visual acuity of 1.3 lines in the treated group.
Laser photocoagulation proved not to be useful in macular edema secondary to central retina vein occlusion. The Central Vein Occlusion Study (38) found that initial visual acuity is the best prognostic factor for patients; patients with initial visual acuity of 20/40 or better often retain good vision, patients with initial visual acuity of 20/50 to 20/200 have a variable prognosis (20% may get better), and patients with initial visual acuity worse than 20/200 have a poor prognosis (80% remain 20/200 or worse).
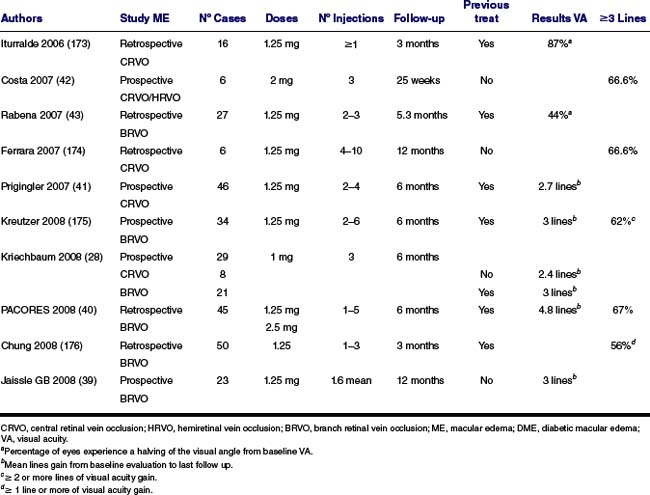
Bevacizumab is being used for macular edema in branch and central occlusions with promising outcomes (Table 36-2) (Figs. 36-1 and Figs. 36-2). Investigators reported gain of 2 to 4.8 lines of vision after bevacizumab treatment in patients with macular edema secondary to vein occlusions (39–41). Around 67% of the patients gain 3 or more lines of visual acuity after treatment (40, 42). The optimum dosing and sequence for treatment is still undetermined. The literature available seems to indicate that multiple injections are required to achieve better visual acuity and to maintain improvement. Two to three injections over the first 6 months appear to be the most common management strategy. (43). Visual improvement and reduction in macular thickness is reported as early as 1 week after treatment and remains stable or improves for up to 2 months after the injection (43, 44). Three to four months after treatment visual acuity declined and macular thickness increased in some patients (44). To date no investigators have reported worsening of nonperfusion after treatment with bevacizumab, and some of them reported collateral vessel formation.
Irvine-Gass Syndrome
Cataract surgery with intraocular lens implantation can be complicated by postoperative cystoid macular edema (Irvine-Gass Syndrome). The incidence of clinically significant cystoid macular edema (CME), defined as a snellen visual acuity of 20/40 or worse with petaloid perifoveal macular edema, was reported in between 0% and 13% (45, 46). Postsurgical macular edema resolves spontaneously in nearly 75% of cases within 6 months. In other cases, where spontaneous resolution is not achieved, CME can be difficult to treat. Treatments used for Irvine-Gass syndrome include systemic, periocular, intravitreal, and topical corticosteroids; oral and topical nonsteroidal anti-inflammatory drugs (NSAIDs); oral and topical carbonic anhydrase inhibitors; and pars plana vitrectomy. Cases that are refractory to medical treatment with steroid and non-steroid medication, and patients with contraindication for steroid use can be treated with anti-VEGF drugs.
TABLE 36-2 BEVACIZUMAB FOR MACULAR EDEMA SECONDARY TO VASCULAR OCCLUSIONS
Intravitreal bevacizumab has been used in several cases of pseudophakic CME with positive results (27, 47, 48). The Pan-American collaborative Study Group (27) reported the largest series of patients with Irvine-Gass syndrome treated with bevacizumab. The report includes 28 eyes from 5 different institutions with CME after cataract surgery treated with primary intravitreal bevacizumab. The mean time from cataract surgery to treatment was 13 months (range 1–60). None of the eyes receive intravitreal treatments or had vitreous surgery previously. Seventy-one percent of patients gained 2 lines or more of visual acuity after bevacizumab treatment, with a mean significant reduction in central macular thickness.
A German group reported (49) 16 eyes with refractory macular edema after cataract surgery that received intravitreal bevacizumab. Interesting, none of the eyes experienced improved visual function despite multiple injections. Although central retinal thickness improved significantly in 81% of patients, the anatomical change was mild and did not translate into visual improvement in most of the cases. Patients in this study were heterogeneous with chronic and recalcitrant CME. Eyes included in the study did not respond to previous treatment with NSAIDs, corticosteroids, or acetazolamide.
The difference in the characteristics of patients in both studies may explain the divergence in results. Treatment of postoperative CME remains controversial, especially in cases of chronic CME, which is often unresponsive to different therapies.
IDIOPATHIC MACULAR TELANGIECTASIS
Idiopathic macular telangiectasias (IMT) are dilated capillaries that develop in the macula and perifoveolar areas without a known cause. In 1993, Gass and Blodi (50) established a classification of these entities with subgroups and stages. In type 2 (perifoveal telangiectasia) the telangiectatic blood vessel is limited to the perifoveolar area and is associated with leakage and cystic appearance of the fovea. Typical findings in fluorescein angiography are parafoveal ectatic capillaries and late diffuse leakage, mainly temporal to fovea. Yannuzzi et al. (51) have recently updated the classification scheme for IMT in which type 2 A is referred as perifoveal telangiectasia. This entity has been divided into two stages: nonproliferative, characterized by perifoveal telangiectasis, crystalline deposits, subretinal pigment plaques, right angle vessels, and inner lamellar cysts; and proliferative, which is defined by the presence of choroidal neovascularization.
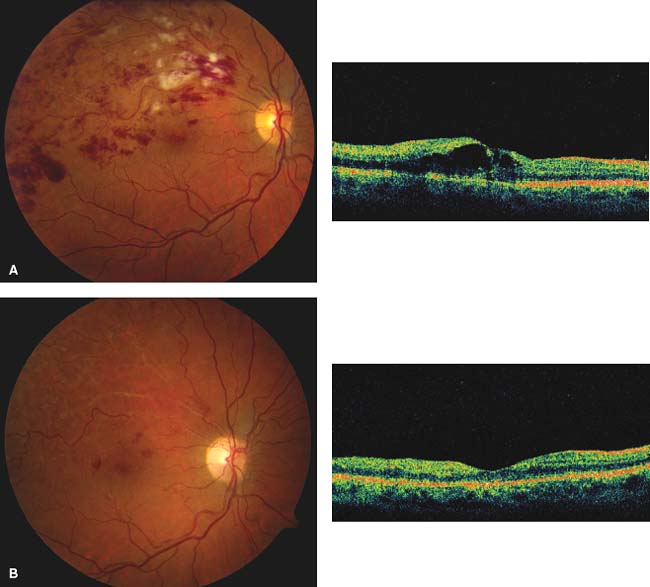
Figure 36-1. A: Fundus photo and OCT of right eye demonstrating Branch retinal vein occlusion and macular edema, AV 20/100. B: Fundus photo and OCT 6 months later after one Avastin treatment. Visual acuity (VA) 20/20 at 1-year follow-up.
Bevacizumab has been used in nonproliferative and proliferative type 2 telangiectasias with diverse results (52–58). Issa et al. (53) report a mean increase in visual acuity of 8 letters after intravitreal bevacizumab administration in 6 eyes with nonproliferative type 2 IMT; the 16 and 21-month follow up showed that VEGF inhibition resulted in an increase in mean visual acuity and decrease in parafoveal leakage and central retinal thickness in all treated eyes. The authors conclude that the effect was temporary, with a rebound effect on parafoveal leakage and central retinal thickness about 3 to 4 months after treatment. The use of bevacizumab appears to be more advantageous in cases of proliferative disease (59).
Uveitis
CME and choroidal neovascularization (CNV) are the two complications associated with uveitis that have been treated with intravitreal bevacizumab.
CME is one of the most common causes of significant visual loss in patients with intraocular inflammation. It is more often associated with intermediate uveitis, posterior uveitis, and panuveitis. Studies showed increased aqueous humor levels of VEGF in patients with uveitic macular edema (60). The classic approach to treat uveitic CME includes corticosteroids (topical, intravitreal or systemic), NSAIDs (topical and systemic), and systemic carbonic anhydrase inhibitors. Bevacizumab has been used for uveitic CME in an attempt to block VEGF and address CME from a different causative mechanism. Coma et al. (61) published the results of 13 eyes with recalcitrant CME secondary to uveitis treated with intravitreal bevacizumab; more than a third of patients experienced improved visual acuity, and 46% had decrease foveal thickness after treatment. These results were similar to the results of Mackensen et al. (62) where 40% of eyes improved visual acuity after treatment.
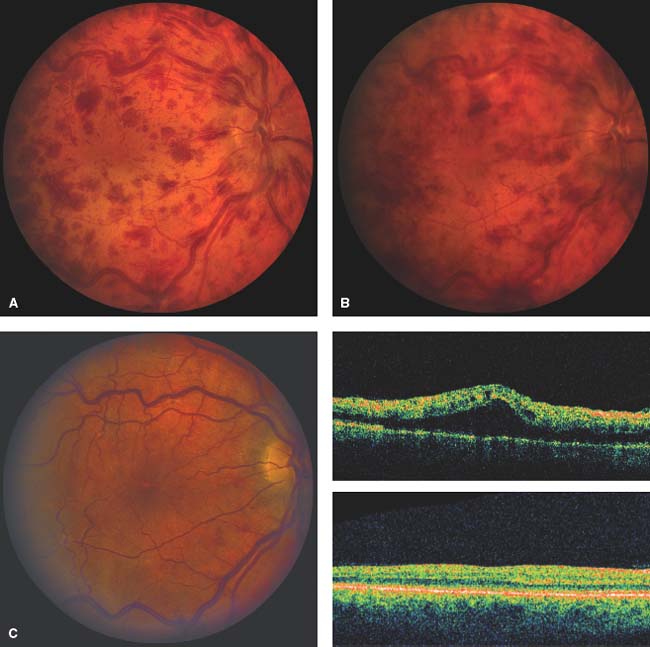
Figure 36-2. A: Fundus photo of right eye with central retinal vein occlusion, VA 20/25. B: Fundus photo of same eye 2 months later demonstrating increase in hemorrhage. OCT shows macular edema, VA 20/200. C: Fundus photo of same eye after four intravitreal bevacizumab treatments. OCT shows resolution of macular edema VA 20/25.
CNV may occur in uveitic patients secondary to inflammation and/or ischemia. It is a rare complication and sometimes responds to systemic and local corticosteroids, photodynamic therapy (PDT), and more recently anti-VEGF treatment. Bevacizumab has been used to treat CNV (subfoveal, juxtafoveal, and peripapillary) secondary to uveitis with positive results (63–66). It is also being used in CNV secondary to multifocal choroiditis and chorioretinitis (67, 68), toxoplasmosis (69, 70), presumed ocular histoplasmosis (71, 72), and punctate inner choroidopathy (73), with promising results.
BEVACIZUMAB IN CHOROIDAL NEOVASCULARIZATION
CNV is an important cause of visual loss. The visual loss is mainly associated with intraretinal or subretinal fluid, hemorrhage, or fibrosis. CNV most commonly occurs in the setting of ARMD, but it may result from any retinal pigment epithelium and Bruch’s membrane-complex perturbation. CNV may arise from more than 25 different ocular diseases including angioid streaks, multifocal choroiditis, myopia, and trauma.
The development of CNV has been shown to be associated with an alteration in the delicate balance of various growth factors involved in angiogenesis (74–76). VEGF is a powerful angiogenic factor and is essential for the development of CNV. On the other hand, pigment epithelium derived factor (PEDF) is known to be a strong inhibitor of neovascularization. In presence of bevacizumab, the VEGF level is reduced and PEDF level is increased; these changes are favorable for inhibition of CNV angiogenesis (77).
Bevacizumab has been used for CNV with good results after intravitreal treatment in age related macular degeneration, pathologic myopia, idiopathic CNV (78, 79), CNV secondary to central serous retinopathy (78), to adult-onset vitelliform dystrophy and Best’ disease (80, 81), to angioid streaks (82–84), to pseudoxanthoma elasticum (85, 86), and choroidal osteoma (87, 88).
AGE-RELATED MACULAR DEGENERATION
CNV is responsible for 80% to 90% of severe cases of vision loss in ARMD patients (89–92). Rosenfeld et al. were the first to report the use of bevacizumab in ARMD patients. Since then, clinical experience with bevacizumab has been published in retrospective and prospective studies, case series, and multiple personal experiences with unpublished data.
Bevacizumab has been tried in patients with subfoveal classic and occult membranes, in naïve and previously treated patients, in lesions with subretinal hemorrhage and with pigment epithelium detachment (Table 36-3) (Fig. 36-3) (93–103).
Patients considered treatment failures after intravitreal pegaptanib (Macugen) and PDT, and patients with chronic lesions with poor visual acuity show some visual gain from bevacizumab treatment (98, 99, 104, 105).
The most commonly used dose is 1.25 mg in 0.05 cc; some reports compared 2.5 mg with the 1.25mg and did not observe statistically significant differences in changes of visual acuity, ocular coherence tomography (OCT) macular thickness, or number of reinjections needed (106). The optimal treatment schedule is unknown. Arias et al. (107) compared the scheme of loading dose (bevacizumab administered once a month for three months then prn versus Avastin × 1 with subsequent prn dosing) and found that patients did better when bevacizumab is administered in 3 doses once a month and then as needed. Retreatment is necessary to achieve and maintain visual gain; some investigators have reported a mean of 3 to 4 injections over 12 months (95, 106, 108, 109). The need for chronic therapy is indicated by the recurrence of leakage from the CNV, defined as a decrease of visual acuity associated with an increase of subretinal fluid, macular edema on OCT and/or fluorescein angiography, that was observed after the initial treatment in almost all the patients in different reports.
TABLE 36-3 BEVACIZUMAB FOR AMD
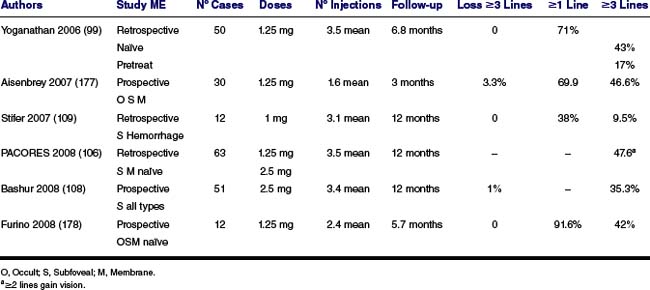

Figure 36-3. A: Fundus photo and IVFA of subfoveal CNVM with AMD. B: IVFA of the same eye demonstrating resolution of the leakage after 3 treatments with bevacizumab.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


