Purpose
To evaluate the axis difference between corneal and internal astigmatism in patients with cataract, because if the axis of corneal astigmatism is opposite to the axis of internal astigmatism, the amount of refractive astigmatism will increase after cataract surgery owing to disappearance of the neutralizing effect of the crystalline lens on corneal astigmatism.
Design
Retrospective cross-sectional study.
Methods
One hundred eighty patients (180 eyes) who underwent cataract surgery were enrolled. Preoperative refractive, corneal, and internal astigmatism were measured using a wavefront analyzer and retrospectively analyzed. On-axis was defined as an axis difference between corneal and internal astigmatism of 180 ± 10 degrees. Opposite-axis was defined as an axis difference between corneal and internal astigmatism of 90 ± 10 degrees. The remaining cases were defined as oblique-axis.
Results
Corneal and internal astigmatic vectors showed a tendency to have the opposite direction. An on-axis difference was seen in 10.0% of patients (18 eyes), oblique-axis in 69.4% of patients (125 eyes), and opposite-axis in 20.6% of patients (37 eyes). Of all eyes, 10.0% had an opposite-axis difference with more than 1.00 diopter (D) of both corneal and internal astigmatism. The percentage of eyes with an opposite-axis difference between corneal and internal astigmatism had a tendency to increase as corneal and internal astigmatism increased ( P = .030 and P = .003, respectively).
Conclusions
A total of 10.0% of all eyes with cataract had an opposite-axis difference with more than 1.00 D of both corneal and internal astigmatism. In these cases, surgical techniques to reduce corneal astigmatism, such as a toric intraocular lens, should be recommended to increase patient satisfaction.
As the accuracy of the intraocular lens (IOL) power calculation is getting better, cataract surgery is now being called a refractive surgery. IOL power calculation is important for attaining optimal refractive outcomes in cataract surgery. However, an optimal refractive outcome cannot be achieved by a spherical IOL in cases of eyes with corneal astigmatism greater than or equal to 0.75 diopter (D). Thus, there are several surgical techniques to reduce corneal astigmatism at the time of cataract surgery: on-axis corneal incision, manual peripheral corneal relaxing incisions, and toric IOLs.
Refractive astigmatism consists of corneal and internal astigmatism. Although total corneal astigmatism can arise from anterior and posterior corneal astigmatism, corneal astigmatism is generally measured from the anterior corneal surface and defined as anterior corneal astigmatism. Internal astigmatism is defined as astigmatism arising from the internal ocular surfaces (posterior cornea, anterior and posterior crystalline lens).
When the axis of corneal astigmatism is similar to that of the internal astigmatism, the amount of postoperative refractive astigmatism usually decreases after cataract surgery. On the other hand, if the axis of corneal astigmatism is opposite to the axis of the internal astigmatism, the amount of refractive astigmatism will increase after surgery because the neutralizing effect of the crystalline lens on the corneal astigmatism disappears. Some patients might experience new astigmatism that did not exist before surgery. Thus, surgical techniques for reducing corneal astigmatism, such as a toric IOL, should be emphasized more in eyes with opposite axes of corneal and internal astigmatism.
Several previous studies have evaluated the prevalence of corneal astigmatism in patients with cataract. However, they did not pay attention to the axis difference between corneal and internal astigmatism. The goal of this study is to evaluate the prevalence of corneal and internal astigmatism according to the axis difference for the choice of a toric IOL in eyes with cataract.
Subjects and Methods
Study Population
This retrospective cross-sectional study included 180 eyes from 180 consecutive patients who underwent cataract surgery with implantation of an IOL at our institute between May 24, 2011 and May 30, 2012. Patients whose corneal and internal astigmatism could be measured using a wavefront analyzer (KR-1W; Topcon, Tokyo, Japan) were included. Patients with best-corrected visual acuities (BCVA) less than 20/40 in the operated eye after cataract surgery, prior ocular surgery (such as pars plana vitrectomy or penetrating keratoplasty), corneal pathology (such as Avellino dystrophy or corneal opacity), severe thyroid eye disease, severe zonulysis, and traumatic cataract were excluded. Institutional Review Board approval for this study was obtained from the Korea University Guro Hospital. All research and data collection adhered to the tenets of the Declaration of Helsinki.
Patient Examination
Preoperative refractive, corneal, and internal astigmatism were measured using the KR-1W. One month after surgery, all patients underwent a complete ophthalmic examination, including slit-lamp biomicroscopy and postoperative BCVA.
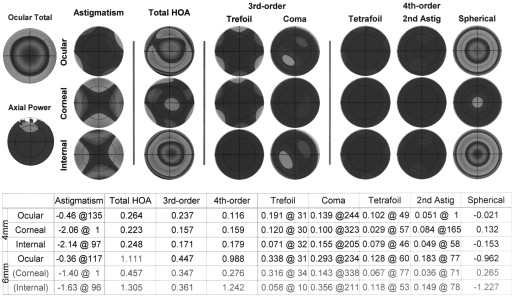
The measurement of refractive, corneal, and internal astigmatism was conducted under high mesopic conditions (8 lux) in the 4-mm optical zone without pharmacologic pupil dilation using the KR-1W. The KR-1W includes 3 technologies: Hartmann-Shack wavefront system, Placido disk topographic system, and standard autorefraction. This device has the advantage that measurements of the refractive and corneal astigmatisms are performed on the same axis and using the same reference for centration. Thus, internal astigmatism can be more accurately calculated ( Figure 1 ).
Main Outcome Measures
Corneal astigmatism was defined as the astigmatism of the corneal anterior surface. Internal astigmatism was defined as the vectorial difference between the corneal plane refractive astigmatism and the corneal astigmatism. Internal astigmatism is composed of posterior corneal and lenticular astigmatism (anterior and posterior).
The refractive, corneal, and internal astigmatism were converted from the “negative-cylinder form” convention to the rectangular forms of Fourier notation for the power vector analysis using the following equations :
where C is negative-cylinder power and angle α is cylinder axis. J 0 is Jackson cross cylinder power at axis 0 and 90 degrees and J 45 is Jackson cross cylinder power at axis 45 and 135 degrees.
For the analysis of the axis difference between the corneal and internal astigmatism, eyes were classified into 3 categories: on-axis, opposite-axis, and oblique-axis. On-axis was defined as an axis difference between the corneal and internal astigmatism of 180 ± 10 degrees, opposite-axis as 90 ± 10 degrees, and the rest were defined as oblique-axis. With-the-rule (WTR) astigmatism was defined as an axis of corneal or internal astigmatism of 180 ± 10 degrees, against-the-rule (ATR) astigmatism as 90 ± 10 degrees, and the rest were defined as oblique astigmatism.
Statistical Analysis
Descriptive statistics for all patient data were obtained using the Statistical Package for the Social Sciences, version 12.0 (SPSS Inc, Chicago, Illinois, USA). Spearman rank-order correlation analyses were done to evaluate the correlation among age, corneal astigmatism, and internal astigmatism. The analysis of variance (ANOVA) test was done to compare the mean age among WTR, oblique, and ATR astigmatism of the corneal and internal astigmatism. Subjects were divided according to whether both corneal and internal astigmatism have more than 1.00 D or not. Frequency distribution of each group according to axis differences between corneal and internal astigmatism were evaluated using χ 2 test. χ 2 linear trend tests were performed to compare the percentage of eyes with opposite-axis difference in 0.50 D steps in corneal and internal astigmatism. Multivariate binary logistic regression analysis was performed to calculate the odds ratio of an opposite-axis difference between corneal and internal astigmatism through several parameters, which showed the significant result from univariate analysis. Results were considered statistically significant if the P value was < .05.
Results
A total of 180 eyes from 180 patients who underwent uncomplicated cataract extraction with implantation of an IOL in the bag were included in this study. Of the 180 patients, 61 were men and 119 were women. The mean (± SD) age was 66.1 (± 10.6) years (range, 39-93 years). The laterality, mean preoperative corneal power, anterior chamber depth, axial length, and predicted refraction are given in Table 1 .
| Parameter | Mean (SD) | Range |
|---|---|---|
| Age (y) | 66.1 (10.6) | 39-93 |
| Sex, n (%) | ||
| Male | 61 (33.9) | – |
| Female | 119 (66.1) | – |
| Laterality, n (%) | ||
| Right eye | 87 (48.3) | – |
| Left eye | 93 (51.7) | – |
| Corneal power (D) | 44.46 (1.55) | 40.46-48.43 |
| Anterior chamber depth (mm) | 3.19 (0.39) | 2.25-4.25 |
| Axial length (mm) | 23.61 (1.56) | 21.08-32.29 |
| Predicted refraction (D) | −0.29 (0.55) | −4.52-0.20 |
The mean cylinder power and J 0 , and J 45 components for the preoperative refractive, corneal, and internal astigmatism measured with the KR-1W are shown in Table 2 . The mean cylinder power of corneal astigmatism was 1.11 (± 0.89) D and the mean cylinder power of internal astigmatism was 1.09 (± 0.77) D.
| D (SD) a | J 0 , D (SD) | J 45 , D (SD) | |
|---|---|---|---|
| Refractive astigmatism | 1.38 (0.89) | −0.35 (0.61) | 0.02 (0.42) |
| Corneal astigmatism | 1.11 (0.89) | −0.03 (0.64) | 0.01 (0.32) |
| Internal astigmatism | 1.09 (0.77) | −0.33 (0.45) | 0.01 (0.37) |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


