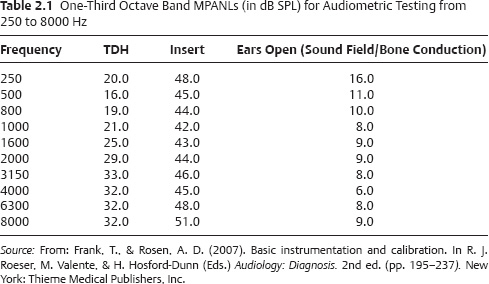
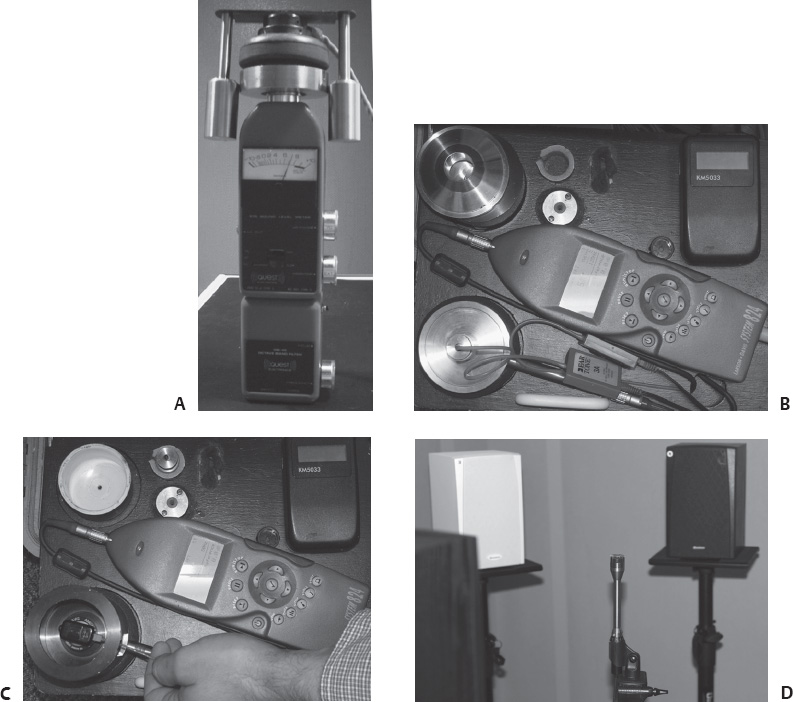
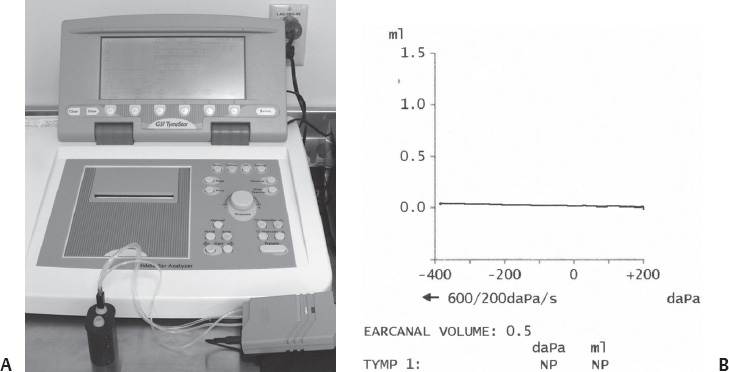
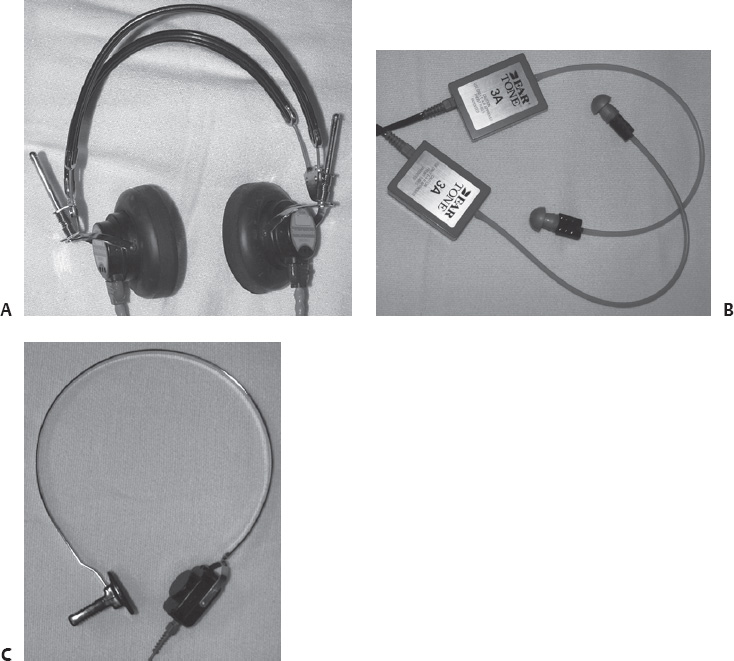
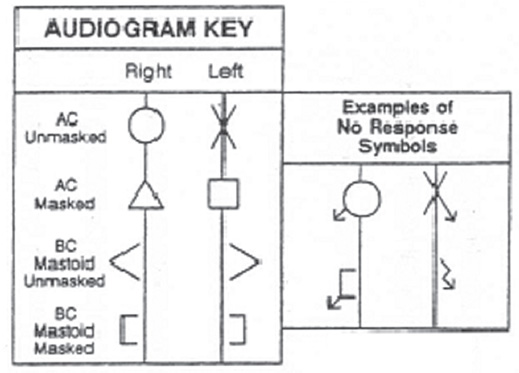
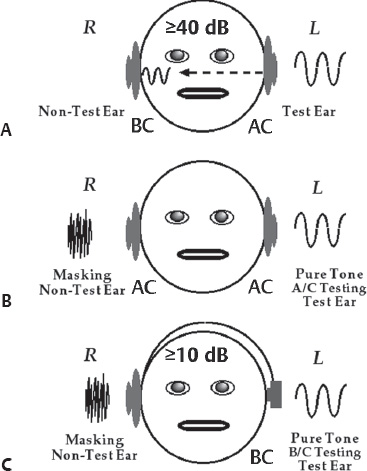
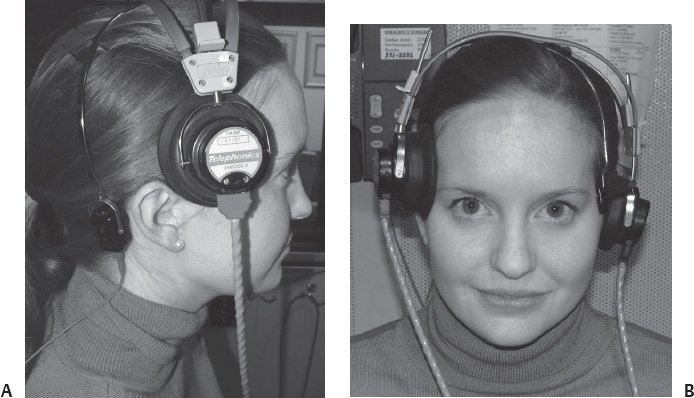
2 Audiometric Testing Audiometric equipment should be calibrated quarterly, with an exhaustive calibration required annually, to ensure that the results obtained via audiometric testing are accurate. In addition, many states require that audiometric calibration be performed annually to acquire and maintain licensure. Audiometric calibration standards are provided by the American National Standards Institute (ANSI) and by the International Electrotechnical Commission (IEC). Calibration of an audiometer involves the use of the following equipment: pistonphone (used to calibrate the sound level meter [SLM]), voltmeter, pressure and free-field condenser microphone, sound level meter with either an octave or one-third octave filter, appropriate couplers (6 cc, 2 cc, artificial mastoid), and a 500 g and 5.4 newton (N) weight. The output of the audiometer is confirmed through the various transducers used in testing (i.e., headphones, insert earphones, bone oscillator, and loudspeaker) whereas the transducer is coupled to an artificial ear, 2 cc coupler, or artificial mastoid. For loudspeaker calibration (Fig. 2.1D), a calibrated free-field microphone is placed in the test room at a distance equal to where the center of a patient’s head would be, but with the patient absent. The output from the calibrated microphone is coupled to a calibrated SLM and one octave or one-third octave filter. Signals (narrowband noise [NBN], frequency-modulated pure tones, or speech) are sent to the loudspeaker from the audiometer, and the output from the loudspeaker is calibrated with the equipment mentioned above to be sure that the measured output adheres to the ANSI S3.6–2004 standard for sound field thresholds. In ANSI S3.6–2004, there are separate standards if the loudspeaker is at 0°, 45°, or 90° azimuth to the patient and if testing is done monaurally or binaurally. Typically, most clinics select the standard for 0° with binaural hearing as their reference for sound field calibration. Reflecting back to Chapter 1 of this guidebook, calibration confirms that an audiometer dial reading of 0 decibels in hearing level (dB HL) is equivalent to the expected decibels in sound pressure level (dB SPL) at each frequency for all transducers. In addition, calibration verifies that no harmonic distortion exists (i.e., 1000 Hz on the audiometer is representative of a pure tone with a frequency of 1000 Hz), that noise interference does not exist, and that the attenuator dial is linear (i.e., an increase of 5 dB HL (on the audiometer dial) results in an increase of 5 dB SPL [in the coupler]). Figure 2.1 illustrates the configuration for calibration of the audiometer using the THD-49/50 headphone coupled to the 6 cc coupler (A), the ER-3A insert earphone coupled to the 2 cc coupler (B), the bone oscillator coupled to the artificial mastoid (C), and the loudspeakers being calibrated by a free-field microphone (D). In addition, regular calibration should be performed on immittance audiometers to confirm that the results obtained in tympanometry, acoustic reflex threshold (ART) testing, and acoustic reflex decay testing are accurate. Figure 2.2 illustrates the calibration of an immittance audiometer with the use of a 0.5 cc cavity. When measuring hearing thresholds, it is important that the noise level in the test environment does not result in erroneously elevated thresholds. According to the ANSI (ANSI S3.1–1999 [Revised 2003]), when testing pure tone thresholds using conventional (TDH-49/50) headphones the maximum permissible ambient noise levels (MPANLs) range from 16 to 33 dB SPL (Table 2.1 , Column 2) depending on test frequency. In addition, the MPANLs for testing with loudspeakers in the sound field or via bone conduction are even lower (6–16 dB SPL; Table 2.1, Column 4), whereas those for testing using insert earphones are higher (42–51 dB SPL; (Table 2.1, Column 3). The ambient noise levels in a “quiet” office will almost always exceed the MPANLs; therefore, special care should be taken when interpreting hearing tests obtained in rooms that do not meet ANSI S3.1–1999 (Revised 2003). Further, if acceptable noise levels cannot be achieved, then the use of a single- or double-walled soundbooth is required. Conventional pure tone audiometry consists of air-conduction (AC) and bone-conduction (BC) testing. AC testing involves the use of a headphone (Fig. 2.3A) or insert earphone (Fig. 2.3B) that delivers the stimulus (250, 500, 1000, 2000, 3000, 4000, 6000, and 8000 Hz) to the external auditory canal. The thresholds obtained via air-conduction testing reflect the status of the outer ear, middle ear, and inner ear. BC testing involves the use of a bone oscillator (Fig. 2.3C) to deliver the stimulus (250, 500, 1000, 2000, 3000, and 4000 Hz) to the mastoid process. The thresholds obtained via BC testing reflect the status of only the inner ear. Thresholds are typically obtained using a bracketing technique in which the audiologist increases and decreases the attenuator dial on the audiometer (dB HL) until threshold is determined. Threshold is defined as the lowest intensity level (dB HL) at which the patient hears the stimulus 50% of the time. (Note: Pure tone testing at inter-octaves of 750 and 1500 Hz are required if a difference of ≥ 20 dB HL exists between 500 and 1000 Hz or 1000 and 2000 Hz, respectively.) Fig. 2.3 Various transducers used in pure tone testing. (A) TDH 49/50 headphones. (B) ER-3A insert earphones. (C) B71 bone oscillator. Pure tone thresholds are plotted on an audiogram, with frequency on the x-axis and dB HL on the y-axis, using the audiometric symbols illustrated in Fig. 2.4. The audiogram must maintain an aspect ratio of 20 dB per octave, meaning that if the distance between 0 and 20 dB HL is 1 inch, then the distance between each octave (e.g., 250 to 500 Hz) must also be 1 inch. Pure tone thresholds for the right ear are commonly recorded using red symbols and are represented by a circle (unmasked) or triangle (masked) for air-conduction and a bracket (with the opening facing rightward) for bone-conduction testing. Pure tone thresholds for the left ear are commonly recorded using black or blue symbols and are represented by an “x” (unmasked) or square (masked) for AC and a bracket (with the opening facing leftward) for BC testing. In some cases, a patient may have no response to pure tones at the limits of the audiometer. Such responses are recorded using the appropriate symbol (unmasked or masked AC or BC) with the addition of an arrow that points diagonally to the bottom left corner of the audiogram for right ear responses and diagonally to the bottom right corner of the audiogram for left ear responses. Fig. 2.4 Audiometric symbols. Masking is the use of a noise source placed into the non-test ear (NTE) to prevent the participation of the NTE in the determination of a patient’s audiometric threshold in the test ear (TE). The noise source used in masking for pure tone testing is narrow-band noise (NBN) centered at the test frequency (e.g., 1000 Hz NBN to NTE when establishing a threshold for 1000 Hz in the TE). Masking for speech audiometry is conducted using a speech noise, which is a broadband noise (centered around 500 to 2000 Hz) filtered to mirror the long-term average speech spectrum. Masking for AC testing is required if the AC threshold at a test frequency in the TE exceeds the BC threshold of the NTE by 40 dB HL or greater at the same test frequency. Thus, this rule requires a contralateral comparison between the AC threshold of the TE to the BC threshold at the same frequency in the opposite or NTE. The criterion of 40 dB HL was chosen as a conservative estimate of the minimum interaural attenuation for AC testing. Interaural attenuation is the amount by which a signal introduced to the TE is decreased during transmission through the skull to the NTE (Roeser & Clark, 2007). Figure 2.5A illustrates the crossover that occurs to the NTE when a signal of greater than or equal to 40 dB HL is introduced to the TE. The masking stimulus for all pure tone testing consists of NBN centered around the test frequency to the NTE (Fig. 2.5B). Fig. 2.5 Illustrations of the average interaural attenuation for air-conduction testing (A), and masking configurations for air-conduction (B) and bone-conduction (C) testing. (Adapted from: Roeser, R. J., & Clark, J. L. (2007). Clinical masking. In R. J. Roeser, M. Valente, & H. Hosford-Dunn (Eds.). Audiology: Diagnosis. 2nd ed. (pp. 261–287). New York: Thieme Medical Publishers, Inc.) Masking for BC testing is required if the AC threshold of the TE exceeds the BC threshold of the TE by 10 dB HL or more, which is referred to as an air–bone gap. The minimum interaural attenuation for BC testing is 0 dB and therefore, the criterion for masking is reduced compared with that of masking for AC testing (Fig. 2.5C). Thus, this rule requires an ipsilateral comparison between the AC and BC threshold of the same ear at the test frequency; however, masking for BC testing is performed via an NBN centered around the test frequency to the NTE using AC. As can be seen in Fig. 2.6, when masking for right BC thresholds, the right ear remains unoccluded while the left ear is covered with the headphone for presentation of the masking noise. In this case, the right earphone is simply placed on the right side of the head so as not to occlude the right ear and to support the earphone placed over the left ear. During speech audiometry, patients are asked to repeat a standardized list of spondee words (e.g., mushroom, baseball) until a speech recognition threshold (SRT) is established. In this case, the words are decreased in 10 dB steps and increased in 5 dB steps until the audiologist finds the softest level in dB HL at which the patient can correctly repeat the word 50% of the time (hence the term speech recognition threshold). The spondee words used to establish the SRT are presented via a recorded list or the audiologist may use a microphone to present the words via monitored live voice (MLV). Although recorded presentation is preferred so that results may be more reliably compared between audiologists and clinics, MLV is often used. In such cases in which MLV is used, it is important that the audiologist present each syllable of the spondee word at 0 dB on the volume units (VU) meter of the audiometer for greater accuracy. The SRT should be in good agreement (± 10 dB) with the patient’s pure tone average (PTA), or the average of pure tone thresholds at 500, 1000, and 2000 Hz, in a reliable test session. Fig. 2.6 (A,B) Transducer configuration for masked bone-conduction testing on the right ear, with masking noise presented to the left ear via the left earphone. In this case, the right earphone is simply resting on the side of the head.
 Why Is It Important to Calibrate Audiometric Equipment?
Why Is It Important to Calibrate Audiometric Equipment?
 What Is the Maximum Allowable Noise Level in the Test Environment?
What Is the Maximum Allowable Noise Level in the Test Environment?
 How Are Air-Conduction and Bone-Conduction Thresholds Determined?
How Are Air-Conduction and Bone-Conduction Thresholds Determined?
 When Is Masking for Air-Conduction Testing Required?
When Is Masking for Air-Conduction Testing Required?
 When Is Masking for Bone-Conduction Testing Required?
When Is Masking for Bone-Conduction Testing Required?
 How Is the Speech Recognition Threshold Determined?
How Is the Speech Recognition Threshold Determined?
| SRT (dB HL) | Interpretation |
| 0–15 | Normal |
| 16–25 | Slight |
| 26–40 | Mild |
| 41–55 | Moderate |
| 56–70 | Moderately severe |
| 71–90 | Severe |
| > 90 | Profound |
Sometimes, an SRT cannot be measured and the audiologist is simply interested in measuring the level (dB HL) at which the patient is aware that speech is present (speech awareness threshold, or SAT). The SAT should be in good agreement with the patient’s best pure tone threshold because the SAT is merely a detection measure and does not require identification of the spondee word. Table 2.2 summarizes the interpretation of the SRT.
 How Is the Word Recognition Score Determined?
How Is the Word Recognition Score Determined?
Another common measure made by audiologists is the word recognition score (WRS). The WRS is a measure in which the patient repeats a list of 50 one-syllable (monosyllabic), phonetically balanced words, and in which a percentage correct score is calculated. For adult patients, the most common word lists are the NU-6 (male or female talker) or the CID-22 (male talker). For children, the most commonly used word list is the PBK-50. The best practice is to use a complete 50-word list unless the patient misses two or less of the first 25 words. If more than two words of the first 25 are missed then best practice is to administer all 50 words. Also, many audiologists unfortunately use MLV presentation of the monosyllabic words. In this practice, the audiologist uses a microphone to present the words live as he/she monitors the vocal effort (input level) of his/her presentation by observing the VU meter on the audiometer. The goal is to peak the words of the carrier phase “say the word” at 0 dB on the VU meter, but let the presentation level of the actual word fall to a more natural presentation. As one can imagine, this is not the preferred best practice as this will create significant inter- and intra-audiologist variability. Best practice demands that the 50 words be presented in a standardized format using ether a compact disc (CD) or tape presentation of the word lists. The words are presented at a dB level at which the listener can hear clearly, which for most normal-hearing listeners is ~40 dB louder than the listener’s SRT (i.e., 40 dB SL, or sensation level). Table 2.3 provides guidelines for interpreting the WRS.
| WRS (%) | Interpretation |
| 90–100 | Normal |
| 76–88 | Slight difficulty |
| 60–74 | Moderate difficulty |
| 50–58 | Poor |
| < 50 | Very poor |
 When Is Masking for Speech Recognition Threshold Required?
When Is Masking for Speech Recognition Threshold Required?
Masking for SRT testing is required if the SRT in the TE exceeds the best BC threshold of the NTE at any of the speech frequencies (500, 1000, or 2000 Hz) by 40 dB or more. Masking for speech audiometry utilizes a speech noise that is presented to the NTE via AC.
 When Is Masking for Word Recognition Testing Required?
When Is Masking for Word Recognition Testing Required?
Masking for WRS testing is required when the presentation level of the words in the TE exceeds the best BC threshold of the NTE by 40 dB or more at any of the speech frequencies (500–2000 Hz). Because word recognition testing is typically conducted at 40 dB SL (in reference to the listener’s SRT in the same ear), it may be assumed that masking for WRS should always be used in patients with relatively symmetrical hearing sensitivity. Again, masking for speech audiometry utilizes a speech noise that is presented to the NTE via AC.
 How Do You Interpret an Audiogram?
How Do You Interpret an Audiogram?
Audiometric interpretation involves determining the type, magnitude, and configuration of hearing loss. As stated previously, the type of hearing loss is determined by comparing AC and BC thresholds, and may be classified as conductive, sensorineural, or mixed. The magnitude of hearing loss is interpreted on a range from normal to profound and is based on the PTA (PTA = average of thresholds at 500, 1000, and 2000 Hz). Table 2.4 reports the magnitude of hearing loss.
The configuration or shape of the hearing loss can be classified as flat, sloping, rising, precipitous, trough, inverted trough, high frequency, fragmentary (corner), or notched. A flat configuration is characterized by little or no change in thresholds across frequencies (±20 dB). A sloping configuration is characterized by hearing thresholds decreasing (poorer) as frequency increases. This sloping configuration can be gradual, sharp, or precipitous. A rising configuration is characterized by hearing thresholds increasing (improving) as frequency increases. This rising configuration can be gradual, sharp, or precipitous. A precipitous configuration is characterized by hearing thresholds decreasing (poorer) very sharply between octave frequencies. A trough configuration is characterized by hearing thresholds being poorer in the mid frequencies and better in the low and high frequencies. This configuration is often associated with genetic hearing loss. An inverted trough configuration is characterized by hearing thresholds being better in the mid frequencies and poorer in the low and high frequencies. A high-frequency configuration is characterized by hearing thresholds being within normal limits at 250 to 2000 Hz and followed by hearing loss at 3000 to 8000 Hz. A fragmentary (corner) configuration is characterized by hearing thresholds being present only in the very low frequencies. A notched configuration is characterized by normal hearing through 3000 Hz with a sharp drop at 4000 and 6000 Hz, and improvement at 8000 Hz. This configuration is typically seen in patients having a history of excessive exposure of loud levels of noise. Another example of a notched configuration is during BC testing when there is poorer hearing at 2000 Hz with better hearing at 1000 and 4000 Hz. This is sometimes called Carhart’s Notch and is sometimes seen in patients with otosclerosis. Figure 2.7 provides illustrations and descriptors for the audiometric configurations discussed above.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree