Purpose
To investigate choroidal topographic changes by swept-source optical coherence tomography (Swept-OCT) in patients undergoing intravitreal injections of anti–vascular endothelial growth factor (VEGF) for exudative age-related macular degeneration (AMD).
Design
Prospective interventional study.
Methods
Consecutive patients with unilateral treatment-naïve exudative AMD were entered into the study over 6 months. Changes in choroidal thickness after intravitreal ranibizumab injections, overall in the macula and in neovascular and non-neovascular areas, from baseline to month 3 (loading phase) and month 6 (pro re nata phase), were investigated by means of Swept-OCT maps.
Results
Forty-one eyes of 41 patients (mean age: 79.4 ± 7.3 years) were analyzed. Choroidal thickness at study entry was significantly thicker in the study eyes as compared to fellow eyes ( P < .05). Analysis of sectorial choroidal thickness over time in study eyes revealed a significant reduction in both neovascular and non-neovascular areas from baseline to month 3 and month 6 ( P < .0001 for all). Central choroidal thickness revealed significant variation between treated and fellow eyes from baseline to month 3 ( P = .017) and month 6 ( P = .045). The visual gain was significantly higher ( P = .02) in patients with a larger choroidal thickness reduction (≥29 μm, n = 11) vs the others (n = 30).
Conclusions
The thinning of the macular choroid (affected or not by choroidal neovascularization), along with the significantly thicker choroid in exudative AMD eyes before treatment initiation compared to fellow eyes, allows the hypothesis that anti-VEGF treatment may favorably influence the choroidal exudation by reducing choroidal vascular hyperpermeability.
Age-related macular degeneration (AMD) is the most common cause of irreversible vision loss in the developed world in people aged over 50 years. The characteristic of the exudative form of AMD is choroidal neovascularization (CNV), which is an abnormal growth of newly formed choroidal blood vessels within the macular area. There are different types of CNV growth pattern based on the Gass classification: sub–retinal pigment epithelial (RPE) (type 1), subretinal (type 2), and combined form.
Optical coherence tomography (OCT) is a noninvasive imaging technique that provides cross-sectional biomedical tissue images. This imaging technique has provided a great advantage in ophthalmology for displaying the retina and RPE, but visualization of the choroid was still limited because of the restricted light penetration owing to presence of melanin in the RPE and in the choroid. In the recently developed swept-source OCT (Swept-OCT), a center wavelength of >1000 nm has been used, while diffuse spectral-domain (SD) OCT uses light with a wavelength of 800 nm. The Swept-OCT, with a longer wavelength, has high penetration, which allows the visualization of the entire choroid. The Swept-OCT, as a high-speed scan rate technique with a relatively low sensitivity roll-off vs depth in comparison with the SD OCT, can produce a 3-dimensional (3D) high-contrast choroidal image, as the software supplied with the instrument allows automatic mapping of the choroidal thickness.
In various studies, OCT has shown the choroidal thinning in exudative AMD. Anti–vascular endothelial growth factor (VEGF) is currently the first-line treatment of CNV in exudative AMD, which has a stabilizing effect and, often, visual acuity improvement. Recent studies have shown that under the effect of anti-VEGF treatment, the thickness of the choroid seems to be reduced, which leads to questions about the clinical consequences of these treatments. On the other hand, other recent studies did not show the effect of choroidal thinning after treatment. A study of the choroidal maps generated by Swept-OCT in patients treated with intravitreal injections of anti-VEGF could allow more accurate measurements, and could provide additional data to this debate.
In this study, using Swept-OCT we investigated the choroidal topographic changes in patients undergoing intravitreal injections of anti-VEGF (ranibizumab) for exudative AMD.
Methods
Study Participants
In this single-center prospective interventional study, consecutive patients presenting with unilateral treatment-naïve exudative AMD were entered over a 6-month period at the Transparency Eye Clinic of Tours. Informed consent was obtained from all patients, in agreement with the Declaration of Helsinki for research involving human subjects. For this prospective interventional study, French Society of Ophthalmology Ethics Committee approval was obtained.
Criteria for inclusion were: (1) both male and female patients >50 years old; (2) diagnosis of treatment-naïve exudative AMD due to presence of type 1 or type 2 CNV; and (3) best-corrected visual acuity (BCVA) between 20/25 and 20/250 (Snellen equivalents) in the treated eye. The exclusion / study exiting criteria were: (1) CNV secondary to causes other than AMD; (2) idiopathic polypoidal choroidal vasculopathy (PCV); (3) previous treatment for CNV prior to initiation of treatment with ranibizumab (such as laser photocoagulation, photodynamic therapy, intravitreal injections of other anti-VEGF); (4) administration of anti-VEGF treatments in the fellow eye during the study period; (5) signs of any other retinal disease in the study eye, such as vitreoretinal disease (eg, epiretinal membrane and vitreomacular traction syndrome) or retinal vascular disease (eg, diabetic retinopathy, and retinal vein occlusion); (6) any ocular surgery in the past 3 months; (7) any thromboembolic event in the past 3 months.
Study Protocol
Before treatment (Baseline), all patients underwent a complete ophthalmologic examination including BCVA measurement using standard Early Treatment of Diabetic Retinopathy Study (ETDRS) charts, slit-lamp biomicroscopy, intraocular pressure (IOP), fundus biomicroscopy, and fluorescein angiography (FA) (TRC-50IX; Topcon, Inc, Tokyo, Japan).
All patients also underwent Swept-OCT (Topcon, Inc), with a wavelength-sweeping laser centered at 1050 nm (tuning range of 100 nm), scanning speed of 100 000 A-scans per second, and a scan window depth of 2.6 mm. The transverse and axial resolutions are, respectively, 20 mm and 8 mm in tissue. The Swept-OCT examinations were performed after pupil dilation by trained examiners. A 3D imaging data set was obtained for both eyes in each subject with a radial scan protocol of 12 lines (12 mm B-scans composed of 1024 A-scans) through the fovea. In order to reduce speckle noise, 16 B-scan images were averaged. The scan then was centered using an internal fixation target and confirmed by a built-in camera of the swept-source OCT system.
The initial treatment consisted of 3 intravitreal injections of 0.5 mg (0.05 mL) ranibizumab (loading phase), followed by a pro re nata (PRN) retreatment approach. Then, monthly, a detailed medical and ocular history of each patient, as well as assessment of BCVA using ETDRS charts and ophthalmic examination including slit-lamp biomicroscopy, IOP, fundus biomicroscopy, and OCT (± FA in doubtful cases), were performed. Intravitreal ranibizumab injection was stopped in eyes with a dry macula (absence of intraretinal and/or subretinal fluid) on OCT. On the other hand, eyes with a persistent or recurrent fluid in the macula on OCT (and/or leakage from the CNV on FA), and/or new macular hemorrhage on fundus biomicroscopy, received an additional injection. At 3 and 6 months from baseline, all patients underwent 3D Swept-OCT evaluation of the study eye (treated).
Morphologic Change Analysis by Swept-Source Optical Coherence Tomography
The 3D Swept-OCT imaging covered a 12 mm circle area, which was centered on the fovea. In each 3D image, the macular thickness was calculated as the distance between the inner limiting membrane (ILM) and the inner border of the RPE–Bruch membrane complex. Also, the choroidal thickness was measured as the distance between the outer border of the RPE–Bruch membrane complex and the chorioscleral border. Each automatically determined line was then manually corrected for any errors by one of the authors (S.R.).
The automated built-in calibration software (software version 9.00.003.17; Topcon, Inc) was used to measure the distance between the lines and create circular macular and choroidal thickness maps of 12 mm diameter. False colors (starting from cool colors progressing to warm colors, 0–500 μm) and ETDRS sectors (6 × 6 mm) were applied to the choroidal thickness map. The mean thickness of each sector was automatically determined in the “center” sector within 1 mm from the center of the fovea, in 4 “inner ring” sectors (superior, inferior, nasal, and temporal) within 1–2 mm from the center of the fovea, and in 4 “outer ring” sectors (superior, inferior, temporal, and nasal) within 2–3 mm from the center of the fovea.
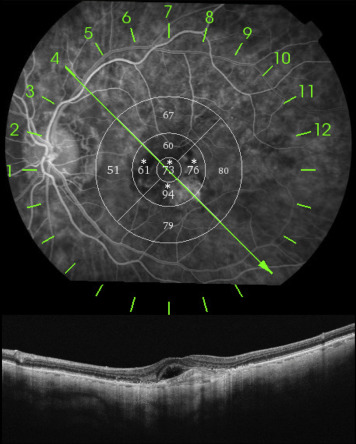
Using the “import image” tool of Swept-OCT (software version 9.12; Topcon, Inc), each FA image acquired with the TRC-50IX was matched with the corresponding infrared image acquired with the swept-source OCT system. As a result, it was possible to match sectorial macular choroidal thickness maps with sectorial FA characteristics. For each ETDRS sector, 2 expert retinal physicians (E.H.S., G.Q.) analyzed the FA images and categorized as “neovascular” areas those sectors characterized by >50% angiographic abnormalities; sectors characterized by ≤50% angiographic abnormalities were categorized as “non-neovascular” areas ( Figure 1 ). Disagreement between readers was resolved by open adjudication.
Statistical Analysis
Statistical calculations were performed using SAS (Version 9.3; SAS Institute Inc, Cary, North Carolina, USA). Based on a 20 μm subfoveal choroidal thickness under the effect of the treatment and a standard deviation (SD) of 25 with an alpha risk = 0.05 and a power of 90% (beta risk = 0.1), the effective size needed to highlight this difference is 34. This number was then increased to 40 in order to account for the lost patient data. All data are presented as mean ± SD. The last-observation-carried-forward (LOCF) method was used to replace the missing data. Student t test and analysis of variance (a repeated-measures ANOVA) were used to evaluate changes of mean BCVA (ETDRS score, letters), mean central macular thickness (CMT), and mean central choroidal thickness (“center” sector) from baseline to month 3 and month 6. ANOVA and Student t test were used for comparison of mean choroidal thickness overall in the macula and in neovascular and non-neovascular areas over time at the “center” sector and at 8 internal and external sectors (superior, inferior, nasal, and temporal) in study eyes. A nonparametric assessment of a relationship between choroidal thickness and BCVA was performed using the Spearman correlation test. A distributional test (Shapiro-Wilk) was done for evaluating normality and data distribution. Multivariate analysis of variance (F-test) was used to evaluate any significant effect of factors like age and axial length on choroidal thickness. The chosen level of statistical significance was P < .05.
Results
Patient Demographics and Main Clinical Findings
Forty-one eyes of 41 consecutive patients (23 female, 18 male; mean age 79.4 ± 7.3 years [range, 62–92 years], mean axial length of 23.3 ± 0.9 mm [range, 20.7–24.8 mm]) diagnosed with exudative AMD fulfilled the inclusion/exclusion criteria and entered the study.
There were no significant effect of age on choroidal thickness in treated and untreated eyes ( P = .15, F = 2.17, and P = .09, F = 1.24, respectively). Also, axial length had no remarkable effect on choroidal thickness in study eyes ( P = .02, F = 0.23) and fellow eyes ( P = .03, F = 0.35).
Mean central choroidal thickness at study entry was significantly thicker in the study eyes compared to fellow eyes (187.2 ± 102.2 μm vs 168.2 ± 89.0 μm, respectively; P = .002). Similarly, mean overall macular choroidal thickness at study entry was significantly thicker in the study eyes (175.4 ± 93.1 μm) vs fellow eyes (155.5 ± 79.9 μm), with P < .0001.
After the loading phase, 14 patients received a mean of 2 ± 0.6 further intravitreal ranibizumab injections between month 3 and month 6.
Changes in Functional and Morphologic Findings During the Study Period
In comparison with baseline (59.4 ± 17.4 letters), the mean BCVA significantly improved to 65.5 ± 17.2 letters ( P < .0001) after 3 months and to 65.0 ± 17.2 letters, P = .0004 after 6 months in study eyes; no further improvement was recorded from month 3 to month 6 ( P = .29) (test for normality of BCVA: P = .0003, baseline; P = .0007, month 3; and P < .0001, month 6).
CMT significantly decreased in the study eyes at both 3 months (from 356.0 ± 104.3 μm to 233.1 ± 43.0 μm; P < .0001) and 6 months (from 356.0 ± 104.3 μm to 246.2 ± 54.2 μm; P < .0001) (test for normality of CMT: P = .0255, baseline; P = 0.0021, month 3; and P < .0001, month 6).
Mean central choroidal thickness between study eyes and fellow eyes was similar at month 3 (171.8 ± 92.1 μm and 164.9 ± 87.6 μm, respectively, P = .16) and at month 6 (172.1 ± 93.3 μm and 165.2 ± 94.9 μm, respectively, P = .98) (test for normality of central choroidal thickness in study eyes: P = .0085, baseline; P = .0112, month 3; and P = .0047, month 6).
Mean central choroidal thickness significantly decreased in the 41 study eyes at both 3 months (from 187.2 ± 102.2 μm to 171.8 ± 92.1 μm; P = .0006) and 6 months (from 187.2 ± 102.2 μm to 172.1 ± 93.3 μm; P = .0025) (test for normality of central choroidal thickness in fellow eyes: P = .0028, baseline; P = .0028, month 3; and P = .0004, month 6) ( Figures 2 and 3 ).
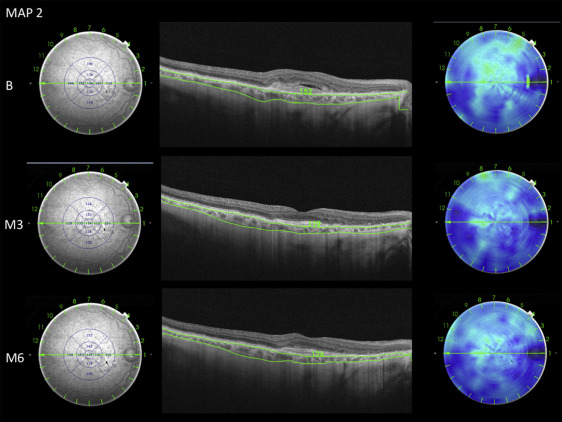
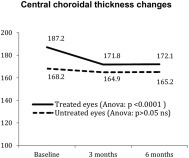
The mean central choroidal thickness in untreated eyes (37 fellow eyes had interpretable choroidal maps) showed a nonsignificant change from 168.2 ± 89.0 μm at baseline to 164.9 ± 87.6 μm at 3 months ( P = .27) and to 165.2 ± 94.9 μm at 6 months ( P = 0.37) ( Figure 3 ).
Analysis of sectorial choroidal thickness over time at the “center” sector and at 8 internal and external sectors (superior, inferior, nasal, and temporal) in study eyes revealed a significant reduction for corresponding sectors in both neovascular and non-neovascular areas from baseline to month 3 and to month 6 ( Table 1 ). No significant differences in choroidal thickness were observed between neovascular and non-neovascular areas at baseline ( P = .91), month 3 ( P = .83), and month 6 ( P = .84) ( Table 1 ).
| Area | Baseline | Month 3 | Month 6 | Variation and Student t Test (Paired): Month 3 vs Baseline | Variation and Student t Test (Paired): Month 6 vs Baseline | Variation and Student t Test (Paired): Month 6 vs Month 3 | ANOVA a |
|---|---|---|---|---|---|---|---|
| Neovascular | 182.3 ± 60.3 μm | 167.4 ± 47.8 μm | 166.3 ± 50.1 μm | −14.9 ± 18.8 μm ( P = .001) | −16 ± 17.2 μm ( P = .0002) | −1.1 ± 8.9 μm ( P = .55) | P < .0001 |
| Non-neovascular | 184.6 ± 77.6 μm | 171.2 ± 74.2 μm | 170.1 ± 75.2 μm | −13.3 ± 15.9 μm ( P = .0006) | −14.5 ± 16 μm ( P = .0003) | −1.2 ± 7.7 μm ( P = .48) | P < .0001 |
| ANOVA | P = .91 | P = .83 | P = .84 | P = .76 | P = .76 | P = .99 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


