Chapter 8 Approach to the Mediastinum
Transcervical, Transsternal, and Video-Assisted
Indications
The most common indication for mediastinal exposure is the presence of a substernal goiter or true posterior descending goiter (see Chapter 7, Surgery of Cervical and Substernal Goiter). Although substernal goiter is a relatively common finding, the need for mediastinal exposure is infrequent but often cannot be determined until the time of surgery. Thyroid cancer that involves mediastinal structures or is associated with enlarged mediastinal nodes is another indication. Certain thyroid malignancies may involve the trachea, larynx, and esophagus, necessitating a cervical exenteration with mediastinal tracheostomy requiring extensive mediastinal exposure. Tumors may involve vascular structures requiring proximal and distal control only achieved by mediastinal exposure. Occasionally, parathyroid adenomas descend into the mediastinum and require access to the mediastinum.
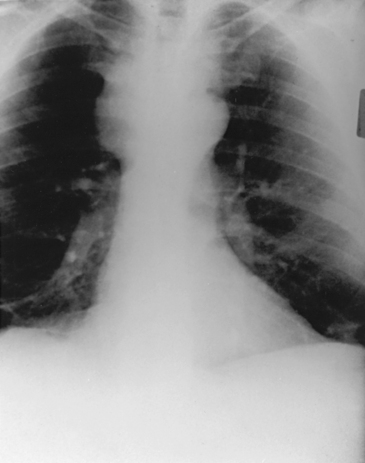
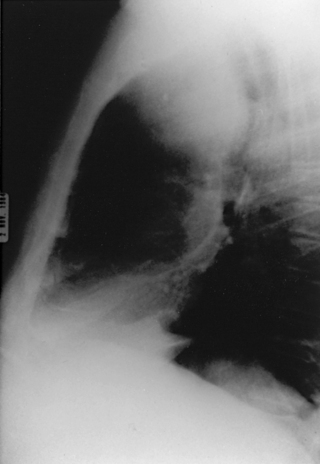
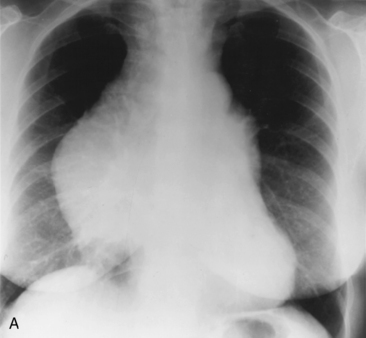
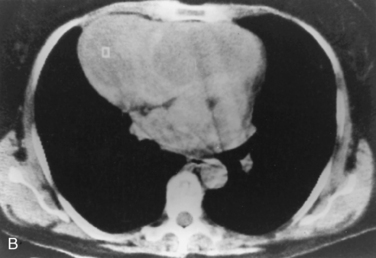
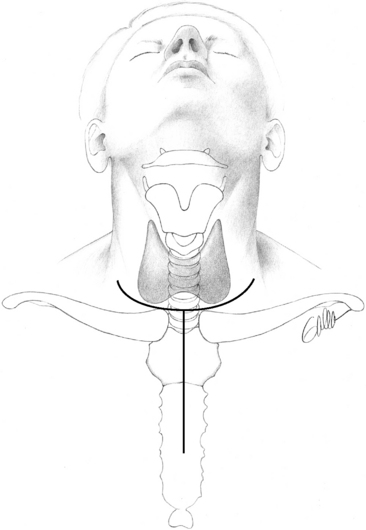
Substernal goiter is the most common clinical problem requiring mediastinal exposure. The typical patient with a substernal goiter is shown in Figure 8-1. This type of patient can almost always have the goiter removed through a low collar incision. Substernal goiters represent between 3% and 47%1–6 of all goiters removed, depending on the definition of what constitutes a substernal goiter (see Chapter 7, Surgery of Cervical and Substernal Goiter). The indications for removal of substernal goiter include actual or impending airway obstruction or threat of malignancy (about 2% to 3%). The majority of substernal goiters can be removed through a cervical incision. In our experience about 3% have required an upper or full sternotomy.2,3 The only case requiring a full sternotomy in our series was a patient who had previous goiter surgery through a posterior thoracotomy (Figure 8-2). A full sternotomy was required to safely remove a recurrent goiter because of massive size, location, and prior thoracotomy (see Figure 8-2).
Mediastinal exposure for substernal goiter is required infrequently in part because extension of the neck acts to migrate the gland into the neck. Conventional techniques of capsular dissection allow gradual delivery into the neck. Thyroid surgeons should be aware of additional techniques described by others for delivery of difficult substernal goiters. These techniques include the use of a spoon,6 a Foley balloon catheter,7 and, rarely, morcellation.8
The true posterior descending goiter is an uncommon entity. The largest experience was reported by DeAndrade.8 DeAndrade reported a total of 9100 patients with goiters, 1300 (14.2%) of whom were intrathoracic (substernal); only 128 were posterior mediastinal in location. Interestingly, all of these were removed through a cervical exposure. The ability to remove posterior goiters through a cervical approach is undoubtedly related to the preservation of some connection to the cervical gland and cervical blood supply, making delivery possible. The use of sternotomy, thoracotomy, or trapdoor incision advocated by some9,10 is rarely indicated currently.
True ectopic thyroid masses (i.e., thyroid tissue separate from the thyroid gland) are extremely uncommon.11 Such lesions may derive their blood supply from the mediastinum. Sternotomy or thoracotomy may be used in these cases because the preoperative diagnosis may be in doubt or concern exists about control of mediastinal vessels (see Chapter 7, Surgery of Cervical and Substernal Goiter).
Surgical Options for Exposure
Partial Sternotomy
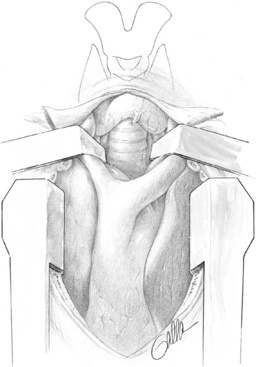
Positioning patients with an inflated thyroid bag under the shoulders to extend the neck brings the carina to the level of the angle of Louis. Division of the manubrium to just beyond the angle of Louis exposes the upper mediastinum and is all that is required for most circumstances. This is accomplished by making a longitudinal skin incision from the midpoint of the collar incision, carrying it down just below the angle of Louis (Figure 8-3). It is important to dissect the suprasternal notch free of surrounding attachments. This allows the surgeon to insert a finger behind the manubrium and clear the areolar attachments. This maneuver is important to sweep the innominate vein and the pleura free from the back of the manubrium. Division of the innominate vein is the greatest risk to division of the upper sternum. Once the back of the manubrium has been cleared, the midline should be identified and scored with the cautery. The manubrium can be divided in a variety of ways. Some prefer the sternal saw. We rely on the Lebsche knife (Figure 8-4). The Lebsche knife has a sharp edge to divide the bone, a broad surface to allow striking with a mallet, and a footplate to allow some control over the depth of division of the sternum. To use the Lebsche knife, the footplate is inserted under the sternal notch and the tip angled upward toward the back of the sternum. The Lebsche knife is vigorously pulled up, lifting the sternum as the mallet strikes it. It is important to divide the manubrium in the midline to allow for reapproximation when the operation is completed. When the manubrium is divided, it is gently spread with a right-angled retractor to allow placement of a small pediatric sternal spreader (Figure 8-5). The spreader is gradually opened to prevent fracture; however, if fracture does occur, it can be reapproximated with expected good results if it is fractured on one side only. This exposure is sufficient for most problems confronting the thyroid surgeon. With the sternal spreader in place, the exposure to the mediastinum is greatly improved. This gives access to the trachea, esophagus, innominate vein, and artery. Dissection can be achieved in the tracheoesophageal groove and into the angle formed by the arch of the aorta and the innominate artery. Mediastinal exposure can be further enhanced with the addition of partial sternotomy (Figure 8-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree