Chapter 2 Applied Embryology of the Thyroid and Parathyroid Glands
![]() This chapter contains additional online-only content, available on expertconsult.com.
This chapter contains additional online-only content, available on expertconsult.com.
The Thyroid Gland
Normal Development of Thyroid
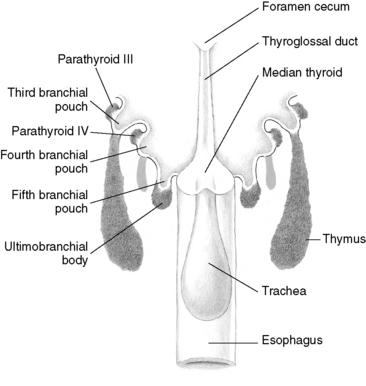
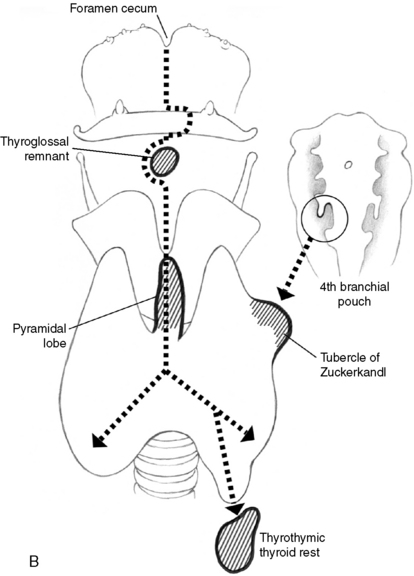
The thyroid gland has a double origin: the primitive pharynx and the neural crest (Figure 2-1). The primitive pharynx is responsible for the origin of medial thyroid anlage, whereas the lateral thyroid anlage originates from neural crest, the source of parafollicular cells or C cells that secrete calcitonin. These cells derive from the ultimobranchial bodies.1 Support for the ultimobranchial origin of C cells has come from the studies of patients with DiGeorge syndrome, a complete or partial absence of the caudal pharyngeal complex. Less than one third of these patients have C cells within their thyroid.2
The primitive pharynx is the origin of the main central portion of thyroid tissue, which appears during the second and third week of fetal life (Figure 2-2). This medial thyroid anlage arises on the ventral pharyngeal wall (the tuberculum impar) at the level of second branchial arch, appearing as a single or paired diverticulum. The median anlage forms the bulk of the thyroid gland. Division of the gland into lateral lobes, if not present from the beginning, occurs so early that it is impossible to determine whether thyroid arises singly or as a paired organ. The median stalk usually has a lumen (the thyroglossal duct) that does not extend into lateral lobes. This diverticulum follows the primitive heart as it descends caudally. It becomes a solid cord of cells that will form the follicular elements. Then, it breaks in two: the proximal part retracts and disappears, leaving only the foramen cecum at the back of the tongue to mark its origin. Early during the fifth week, the attenuated duct loses its lumen and shortly afterward breaks into fragments. The caudal end develops as bilobed encapsulated thyroid gland proper and reaches its final adult orthotopic position by the seventh week and undergoes histologic differentiation into the typical follicles during weeks 10 and 11.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
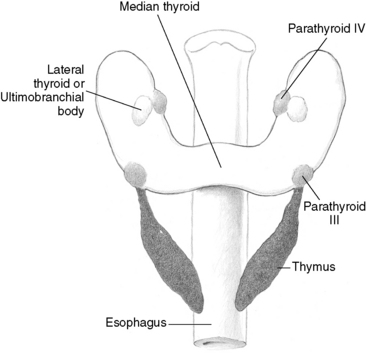
The lateral thyroid anlage develops from proliferation of pharyngeal endoderm. The ventral portion of the fourth pharyngeal pouch becomes attached to the posterior surface of the thyroid during the fifth week and contributes up to 30% of the thyroid weight. The right and left lobes of the thyroid grow caudally with growth of the fetus, taking up their final position at either side of the second to fourth tracheal rings. The line of normal embryologic thyroid descent is called a thyroglossal tract. The causes of the fusion of the median and lateral anlages are unknown. The site of the fusion of these two structures is stated to occur at the tubercle of Zuckerkandl.3,4 Sugiyama speculated that the migration of ultimobranchial body controls the growth of median anlage.5 The fusion of the ultimobranchial bodies and the median thyroid anlage explains why C cells are not scattered throughout the entire thyroid but are restricted to a zone deep within the middle to upper thirds of the lateral lobes along a hypothetical central lobar axis.6 The extreme upper and lower poles as well as the isthmic regions are generally devoid of C cells.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
1. Subtotal or even near total resections, leaving a small posterior remnant of thyroid tissue, should never be done.
2. Because lymphatic drainage of the superior poles of the lobes may flow directly into the lateral neck area, lateral neck nodes should be systematically explored, even if the central neck nodes are not involved.
The thyroglossal duct is an epithelial tube that connects the gland and the foramen cecum (see Chapter 6, Thyroglossal Duct Cysts and Ectopic Thyroid Tissue). Early during the fifth week, the attenuated duct loses its lumen and shortly afterward breaks into fragments. During the fifth through the seventh weeks of gestation, the hyoid bone is formed by condensation of mesoderm with subsequent chondrification from the second and third branchial arches; this grows from behind forward, dividing the thyroglossal tract into suprahyoid and infrahyoid portions.7 The attenuated thyroglossal duct tract usually atrophies and disappears by the end of the eighth week. The tract may persist as a fibrous cord or a minute epithelial tube.
Genetic Control
A number of transcription factors involved in thyroid descent and development have been identified. TTF-1 appears at the earliest stages of thyroid development and regulates expression of thyroperoxidase and thyroglobulin. Disruption of this gene in mice results in thyroid agenesis.8 Pax-8, which has similar actions to TTF-1, is expressed in embryonic thyroid during descent, and heterogeneous mutations are associated with thyroid hemiagenesis.9 TTF-2 regulates the above two genes, and disruption is associated with thyroid dysgenesis.10 HoxA3 regulates diverse embryonic processes. Disruption of murine HoxA3 results in thyroid hypoplasia, whereas combined disruption with HoxB3 or HoxD3 results in failure of fusion of the ultimobranchial body with the thyroid. All of these genetic abnormalities appear to result in impaired thyroid descent or development.
Anomalous Development of the Thyroid
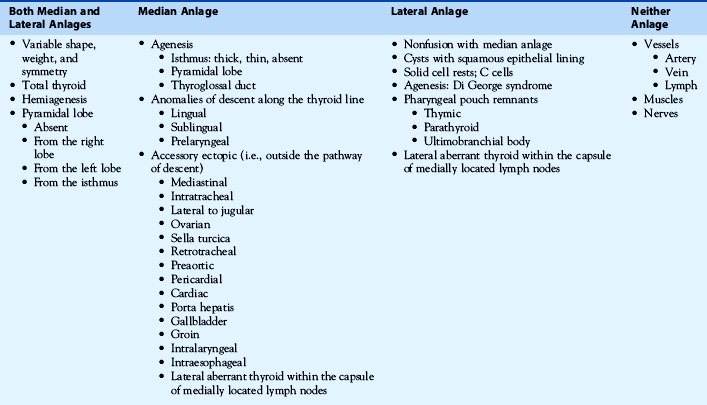
Various anomalies of the development of the thyroid gland involving the median or the lateral anlage (or both) have been described (Table 2-1) (see Chapters 6, Thyroglossal Duct Cysts and Ectopic Thyroid Tissue, and 10, Reoperation for Benign Disease). Developmental variations involving the thyroid can be categorized under the following groups:
Thyroid Ectopias
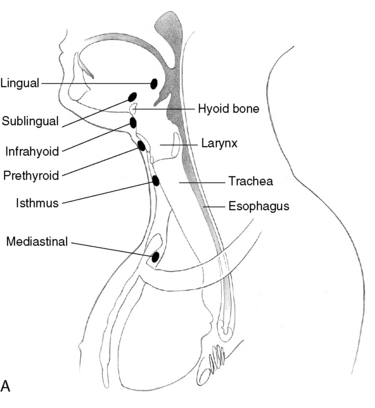
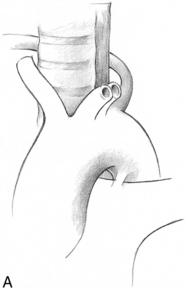
Though ectopic thyroid tissue can be found between the foramen cecum and the normal position of the thyroid gland, the two most common sites of undescended thyroid glands are the lingual thyroid (90%) and anterior neck (10%) (Figure 2-3, A and B). Most of them are detected in childhood and are often associated with hypothyroidism. Under the influence of continued thyroid-stimulating hormone (TSH) stimulation, they may enlarge and produce local symptoms. The ectopic thyroid tissue in the anterior neck may present as a midline mass and may be misdiagnosed as a thyroglossal cyst.11 It is important to differentiate it from the thyroglossal duct cyst, in that it frequently represents the only source of thyroid tissue.
Thyroid Rests
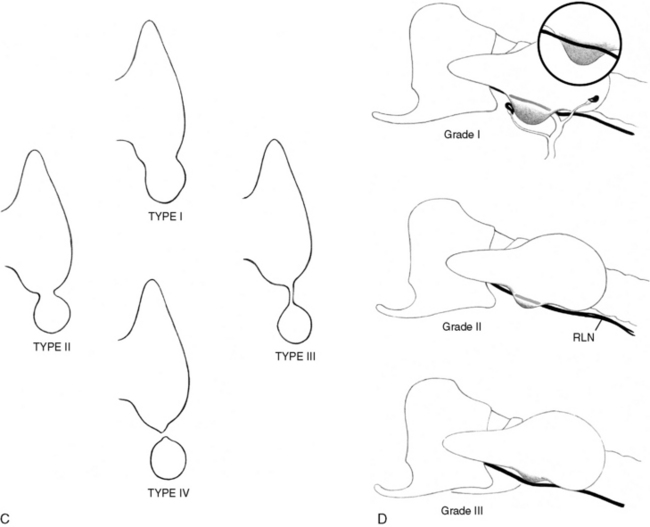
Thyroid rests are isolated rests of normal thyroid tissue lying below the lower pole of the thyroid within the line of the thyrothymic tract, or even within the upper anterior mediastinum (see Chapters 7, Surgery of Cervical and Substernal Goiter, and 10, Reoperation for Benign Disease). They may also have an extension or prolongation of the thyroid tissue attached to the lower pole of the thyroid by a narrow pedicle or even just a fibrovascular band. These rests are presumably an extension of the normal embryologic descent of the thyroid after separation into right and left lobes. Thyroid rests are present in over 50% of patients (see Figure 2-3, C). They are located within the anterior mediastinum. They may be mistaken sometimes for small lymph nodes or even parathyroid glands, and mostly they cause no problems. The development of nodular change within such a rest or prolongation of thyroid tissue might be recognized as a large thyroid nodule quite separate from and caudal to the lower pole of the thyroid gland. If such a nodule lies even further caudal, within anterior mediastinum, following the descent of the heart and the great vessels, it might well give rise to the “isolated” mediastinal or “primary” intrathoracic goiter. The blood supply for these intrathoracic rests is usually from intrathoracic vessels. This explains why primary intrathoracic goiters may require a thoracic surgical approach (i.e., sternotomy) to achieve vascular control.
Sackett et al.12 have suggested a classification for thyroid rests in relation to the thyroid gland (see Figure 2-3, C).
Grade I. Thyroid rests consists of a protrusion of thyroid tissue arising from the inferior aspect of the thyroid gland in the region of the thyrothymic ligament, recognizably distinct from the line of the lower border of the thyroid lobe.
Grade II. Thyroid rests include thyroid tissue lying within the thyrothymic tract and attached to the thyroid proper only by a narrow pedicle of thyroid tissue.
Grade III. Thyroid rests are similar to grade II but are attached to the thyroid gland only by a fibrovascular core.
Grade IV. Thyroid rests have no connection to the thyroid gland.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
Snook et al.,13 in their retrospective analysis of 3044 total or secondary total thyroidectomies performed for benign multinodular goiter in the previous 25 years, reported 11 recurrences and found 5 recurrences in the thyrothymic tract. They concluded that failure to remove embryologic remnants such as thyrothymic residue during total thyroidectomy is a cause of recurrence.
Lingual Thyroid
Failure of the descent of the thyroid gland anlage early in the course of embryogenesis results in a lingual thyroid near the foramen cecum (see Chapter 6, Thyroglossal Duct Cysts and Ectopic Thyroid Tissue). Its applied importance is as follows:
1. In the majority of cases, the lingual thyroid may be the only functioning thyroid tissue.
2. An enlarging lingual thyroid located at the base of the tongue may present with symptoms of dysphagia, upper airway obstruction, or even hemorrhage.
3. Though rare (only 43 cases have been reported so far),14 malignant transformation of the lingual thyroid tissue may occur.
Thyroglossal Duct Cyst
Early during the fifth week, the attenuated duct loses its lumen and shortly afterward breaks into fragments (see Chapter 6, Thyroglossal Duct Cysts and Ectopic Thyroid Tissue). During the fifth through the seventh weeks of gestation, the hyoid bone is formed by condensation of mesoderm with subsequent chondrification from the second and third branchial arches, which grow from behind forward, dividing the thyroglossal duct tract into suprahyoid and infrahyoid portions.15,16 The attenuated thyroglossal duct tract usually atrophies and disappears by the end of the eighth week. This tract may persist as a fibrous cord or a minute epithelial tube, and this persisting tube/duct/cord is called a thyroglossal duct, which connects the gland and the foramen cecum. The thyroid gland may reach its normal position, leaving rests of cells anywhere along this embryonic path, and give rise to postnatal development of cysts; or it may leave rests at any level along the midline developmental pathway (sublingual, prelaryngeal, rarely suprasternal). A thyroglossal duct cyst (TDC) does not have a primary external opening, which are characteristic of some branchial cleft cysts, as the embryologic course of the tract never reaches the surface of the neck.
TDCs are the most common congenital cervical abnormalities, three times more common than branchial cleft remnants. The cyst usually presents as a painless, asymptomatic midline swelling below the hyoid bone and may be observed at any age. TDCs are present at birth in approximately 25% of cases, most are noted during childhood, and the final third become apparent after age 30. The gender incidence is equal. They can be found anywhere in the midline, from the submental region to the suprasternal notch, but are most commonly located halfway between these extremes, near the hyoid bone. Ward et al.17 noted that 80% were juxtaposed to the hyoid bone (25% located in the submental region), 2% lingual, and 7% in a suprasternal location. Only 1% of TDCs were lateral to the midline.17 On examination, cysts are round with a smooth surface and are well defined. With swallowing or protrusion of the tongue, it classically rises in the neck as a result of the cyst being anchored to the hyoid bone and muscles of the tongue. It is usually 1 to 2 cm in diameter, slightly mobile, and nontender unless there is superimposed infection. Oral bacteria may be transmitted through the foramen cecum. Thyroglossal duct sinuses are secondary to infection of the cyst as a result of spontaneous or surgical drainage and are associated with some degree of low-grade inflammation of the surrounding skin. The cutaneous opening is usually 1 to 3 mm in diameter and may intermittently express small droplets of thin mucoid fluid usually clear or yellowish.
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
The operations to cure thyroglossal cysts include removal of cyst with a central portion of hyoid bone and the epithelium-lined tract, running from the cyst to the foramen cecum18 and called as Sistrunk operation. The Sistrunk operation consists of en bloc cystectomy and central hyoidectomy, with tract excision up to the foramen cecum. In Sistrunk’s original report, 31 TDCs were encountered among 86,000 consecutive patients examined at the Mayo Clinic. Sistrunk emphasized the need to make no attempt at isolating the suprahyoid portion of the duct. “At this point the tract usually passes through the hyoid bone, although it is sometimes found passing above or below it.”18 The index finger of the surgeon’s hand can be placed in the patient’s mouth, on the foramen cecum to elevate the tongue and to guide excision of the suprahyoid tract. Sistrunk observed that the excision invariably proceeds at a 45-degree angle. Although Sistrunk recommended apposition of the cut edges of the hyoid bone, it is more recently thought to be neither necessary nor wise to attempt to repair the cut ends of the hyoid, especially in a child. Drainage of the wound is warranted in the presence of acute infection or operative disruption of the cysts.
Histologically, a TDC is lined by pseudostratified ciliated columnar epithelium, squamous epithelium, or both. The supporting wall of the cyst consists of fibrous tissue and frequently contains heterotopic thyroid tissue (20%) and accumulations of other chronic inflammatory cells. Approximately 1% of TDCs may undergo neoplastic change, 85% of which are papillary adenocarcinoma. Cases of squamous cell, anaplastic, and Hürthle cell carcinoma in TDCs have been reported.19 Usually these malignancies are discovered following a Sistrunk procedure. Widstrom’s criteria for the diagnosis of primary papillary carcinoma arising in a TDC include the following20:
Pyramidal Lobe
The pyramidal lobe is the embryologic remnant of the thyroglossal tract. The frequency of presence of pyramidal lobe varies from 55% to 76%.21 When present it is more commonly associated with left side of the isthmus. The pyramidal lobe contains thyroid follicular cells and must be adequately identified and excised along with any fibrous remnant. If overlooked during surgery, it may cause recurrent benign nodular goiter or recurrent hyperthyroidism or malignant disease developing as either a midline or a left-sided neck swelling.
Tubercle of Zuckerkandl
The tubercle of Zuckerkandl (TZ) is a posterolateral projection from the thyroid lobe resulting at the point where lateral and the medial components fuse (see Figure 2-3, D)4,22
Applied importance
1. A grade III tubercle can be associated with significant pressure symptoms and may be the cause of persistent symptoms after subtotal thyroidectomy.
2. TZ is intimately associated with RLN and the superior parathyroid. Enlargement of the tubercle usually occurs lateral to the recurrent laryngeal nerve—the nerve appears to pass into a cleft medial to the enlarged tubercle. An uncommon but high-risk arrangement is where the recurrent laryngeal nerve runs ventral to an enlarged tubercle (see Figure 2-3, D).
3. Elevation of the TZ allows safe dissection of recurrent nerve as it passes medially through a tunnel.
4. The widened prevertebral space, as seen on plain lateral x-ray of the neck, could provide an idea of the presence of an enlarged (grade II/III) TZ.23
The Recurrent Laryngeal Nerve
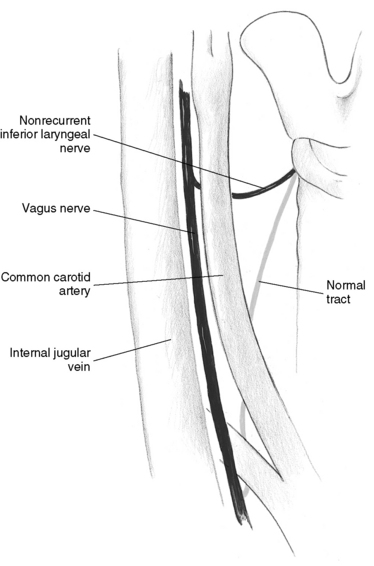
The anatomic course of the recurrent laryngeal nerve is widely variable. In most cases, variability is related to the relationship between thyroid nodules and the inferior thyroid artery, as well as to precocious and variable branching. These variations will be the topic of Chapter 33, Surgical Anatomy and Monitoring of the Recurrent Laryngeal Nerve. However, embryology can solely explain the congenital anomaly of the RLN: the nonrecurrence. It is important for thyroid surgeons to be aware of the possibility of the presence of nonrecurrent inferior laryngeal nerve (NRILN), as it may become damaged inadvertently during a thyroidectomy, causing permanent vocal cord palsy. Several published reports have described the incidence of NRILN of 0.21% to 1.6% on the right side and 0.4% on the left side.24,25,33,34
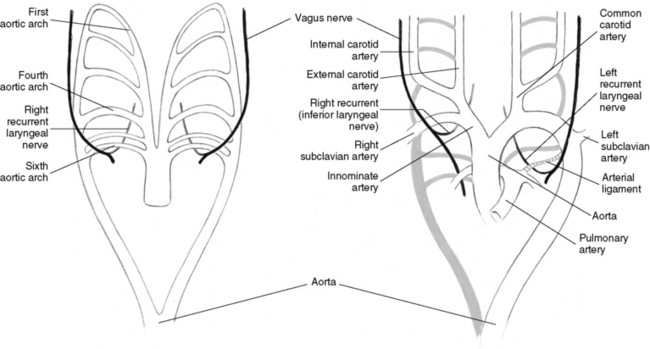
Normal Embryology of RLN
The inferior laryngeal nerves are derived from the VI branchial arch. These originate from the vagus nerves under the VI aortic arch. Subsequently, the V and the distal portion of the VI aortic arch regress, on both the right and left side, and the two laryngeal nerves remains anchored to the structures that develop from the IV arch (i.e., the right subclavian artery and the aortic arch on the left side). When the heart descends into the thorax, these arteries take with them the nerves, which then assume their normal recurrent course (Figure 2-4).
Anomalous Development of the RLN
When the segment of the fourth right aortic arch between the origin of the right common carotid artery and the right subclavian artery disappears, the resulting break in the primitive arterial ring leads to a left-sided aortic arch, with the right subclavian artery being the last collateral (Figure 2-5). In this case, the right subclavian is formed at the expense of the dorsal aorta and the seventh intersegmental artery and runs in an oblique direction (lusoria course) to the right axillary region. This atresia has two other consequences on the vascular system: the absence of the innominate artery and of the arterial segment under which the right RLN normally forms a loop. As a result, during the embryonic lengthening of the neck, the nerve branch is not attached at the thorax level and the right RLN arises from the vagus nerve at the cervical level (Figure 2-6). Therefore, nonrecurrence of the RLN always results from this vascular anomaly during embryonic development of the aortic arches.24,26
Implications of Anomalous Development
![]() Please see the Expert Consult website for more discussion of this topic.
Please see the Expert Consult website for more discussion of this topic.
Implications of Anomalous Development
The following observations can be made from available literature:
1. Until recently, the chance of predicting the presence of an NRILN is very low. However, some clues may be provided by the presence of impairment of swallowing,24 the presence of abnormal right subclavian artery (arteria lusoria) on a computed tomography (CT) or the demonstration of distortion of esophagus (bayonet image) caused by the retroesophageal esophagus on a barium swallow,24,27 or endoscopy showing presence of pulsations behind the cervical esophagus.24,27 Recently, it has been demonstrated that preoperative neck ultrasonography may suggest the presence of an NRILN.27 Indeed, normal vascular anatomy implies a so-called Y sign on the side represented by the division of the innominate artery in the common carotid artery and subclavian artery. In the absence of this Y sign, an aberrant right subclavian artery (arteria lusoria) is suspected. As a consequence, in the absence of the Y sign, an NRILN should be expected.27
2. Because of its anatomic position, an NRILN is at great risk of being damaged during surgery. In a large series, Toniato et al.28,29 reported a 12.9% injury rate among 31 patients with an NRILN, which is much higher than the rates of RLN described by most authors in published reports.
3. Three anatomic variants have been recognized29:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree