Neurotology and skull base surgery slowly emerged out of a confluence of interrelated disciplines and technologies over the past century to become the field that we know today. Its formation required the marriage of neurosurgery and otology, the introduction of the operating microscope, and advances in surgical technique, anesthesia, and radiology. Along the way, the field also began involving specialists within ophthalmology and craniofacial and plastic and reconstructive surgery. Lastly, and perhaps most importantly, the formation of neurotology and skull base surgery required pioneering surgeons who were willing to push the boundaries of their training, sometimes under the ridicule or scorn of the medical establishment. This historical overview focuses upon the origins of the specialty, from the birth of otology and neurosurgery up through the last quarter century.
The nineteenth century
Adam Politzer: the father of otology
The origins of otology are instrumental in understanding contemporary neurotology, and no discussion of otology can ensue without appreciating the contributions of Politzer. If one can rightly be called the “father” of otology, he must be Adam Politzer (1835–1920). Without diminishing the work of other great men during that time, such as Schwartze, Gruber, and von Tröltsch, Politzer was the most charismatic leader of this newly emerging specialty. Politzer’s mission—to establish a correlation between the findings of his dissections and true clinical findings—had been realized in part by Toynbee in London, Wilde in Dublin, and von Tröltsch in Wurzburg. None of these ear specialists had access to the tremendous wealth of pathology offered by the Vienna General Hospital, however, which cared for 3000 to 4000 patients at any given time . In this setting, Politzer completely characterized a whole series of diseases previously grouped under the vague heading “dry middle ear catarrh.” He was the first to define panotitis, leukemia of the ear, and labyrinthine suppuration and established that a cholesteatoma was related to an ingrowth of squamous epithelium. His textbook, Lehrbuch der Ohrenheilkunde (Textbook of the Diseases of the Ear and Adjacent Organs), originally published in 1878, was in its fifth edition by 1908, had been translated into multiple languages, and was used the world over as the standard of otologic practice. Politzer, along with his colleague Joseph Gruber, had made Vienna the premier destination for otologic training in the world at that time and had established otology as a respectable specialty in its own right.
Resurrection of the mastoidectomy
The “mastoidectomy” was abandoned in the late 1700s and continued to be shunned by the medical community until at least 1870 because of disastrous early attempts . Herman Schwartze (1837–1900) ( Fig. 1 ), in the late 1800s, is most credited with resurrecting the modern mastoid operation as we know it today. Schwartze was born in 1837 in Neuhof, Germany, and later studied in Berlin and Wurzburg, Germany. He was assistant at the Anatomopathological Institute in Wurzburg and—like many otologists of his generation—was a pupil of von Tröltsch. In 1859, he obtained his medical degree and subsequently took a post as professor in Halle, Germany, where he directed the Otological clinic at Halle University until his retirement. Schwartze also was involved with helping to start the first journal dedicated solely to the ear, Archiv fur Ohrenheilkund e, in 1863 along with von Tröltsch and Politzer. Schwartze eventually succumbed to a nervous condition of restlessness, vertigo, and delusions, dying of heart failure at the age of 73.
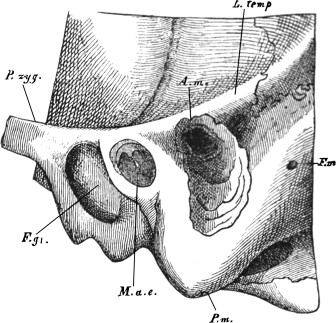
It was Schwartze’s mentor, von Tröltsch, who was responsible for urging Schwartze to fully develop a method of treatment for suppurative processes of the temporal bone. In 1863, Schwartze and Eysell published his “epoch-making” work on the indications for the mastoid operation and his success with the use of specifically designed chisels and gouges ( Fig. 2 ). According to Whiting , an American otologist, in 1911, through this publication Schwartze had “…clearly enunciated the technical and symptomatic principles upon which are based the steps of the modern mastoid operation as performed to-day (sic), and however much we may modify our practice the innovations result in a little more or a little less than Schwartze’s operation…”. Later, in 1889, Stacke, and subsequently, Zaufal in 1890, described the radical mastoid operation .
Sir William Macewen: the first skull base surgeon
If one man can be named the first true skull base surgeon, then surely he must be Sir William Macewen ( Fig. 3 ). Once called the founder of neurosurgery by Cushing and Eisenhardt, and “the unfair surgeon” by others for his exhaustive work ethic, leaving little behind for “…aftercomers to improve or amend” , Macewen left behind a legacy that is still felt today. Macewen was born in 1848 on the Scottish Island of Bute, the youngest of 12 children. As the son of a master mariner, the young Macewen learned to use tools and his hands at an early age. He joined the Glasgow Medical Faculty in 1865 and began his surgical work at the same time that Joseph Lister performed his epoch-making antiseptic research. Lister was Macewen’s premier influence as a young faculty member and was instrumental in Macewen’s pioneering work in surgical antisepsis.
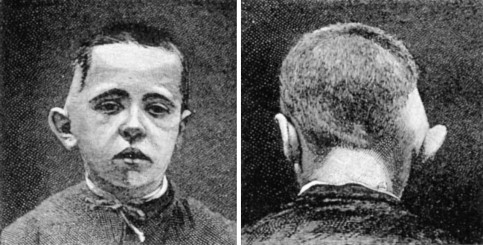
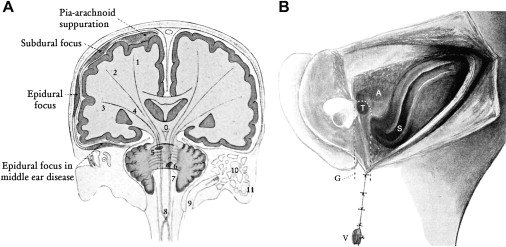
In his now classic, Pyogenic Infective Diseases of the Brain and Spinal Cord , Macewen outlined his technique of treating otogenic intracranial complications. His results were so extraordinary for the era—they were unequaled until the era of computed tomography—and have been deemed “…nothing short of extraordinary” and “…one of the most remarkable books ever written on a neurosurgical subject” . Certainly, one can claim that it also is one of the most remarkable books ever written on a neurotologic subject. In the monumental work, he described 94 cases of intracranial infections and reported such extraordinary results as successful evacuation of a brain abscess in 21 out of 22 cases ( Fig. 4 ). As later pointed out by Jefferson , Macewen may deserve the honor of having written the first clear description of mastoiditis. Macewen reported on 54 mastoidectomies for infections confined to the middle ear and mastoid and a separate listing of mastoidectomies in which there was extension into the cranium. As a surgeon who was “…as familiar and at home operating on the head and brain, as a clinician educated by past experience to recognize the signs of brain disease, and as an anatomist who had made a special study of the ear, he was triply armed immediately to follow the clues given him by the state of the patient or local extensions of the disease” . For these reasons, Macewen must be considered the first true skull base surgeon, equally versed in operations of the ear and brain and the pathologic processes affecting both. It is, perhaps, because of Macewen’s residence in Glasgow, some distance from the epicenter of British medicine in London, that he felt that his accomplishments were unrecognized during his lifetime .
In his later years, Macewen became an elder statesman of surgery. He was president of the British Medical Association, president of the International Society of Surgeons, and was the surgeon to HM the King in Scotland. He was invited to become the chair of Surgery at the newly established Johns Hopkins Medical School in 1889, but an agreement was not reached and Halstead ultimately was appointed instead. Macewen died after a severe case of pneumonia in 1924 at the age of 76 .
Victor Horsley and the birth of neurosurgery
It was not just otology that had defined itself as a unique subspecialty in the latter half of the nineteenth century. Neurosurgery, the second pillar of neurotology and skull base surgery, also saw its nascent beginnings during this time. The National Hospital for Nervous and Mental Diseases, located on Queen’s Square in London, is considered by most to be the birthplace of neurological surgery. Although Macewen was clearly one of the stars of this emerging field, his practice in distant Glasgow limited his influence among his contemporaries. The National Hospital hosted such luminaries as Charles-Édouard Brown-Séquard, John Hughlings Jackson, and Sir William Gowers, making it the center for neurologic studies in the world at that time; however, the most famous surgeon to grace the hospital staff also was credited with the founding of modern neurologic surgery: Sir Victor Horsley (1857–1916). A contemporary of Macewen’s, and also credited with some of neurosurgery’s earliest successes, it was Horsley’s “…indefatigable physiological experimentation in addition to his clinical and pathological experiments” that has led to his inclusion in neurosurgery’s pantheon . Horsley also was the first surgeon to devote most of his efforts to neurosurgery. His contributions to neurosurgery included the first laminectomy for a spinal neoplasm, the first carotid ligation for aneurysm, the first transcranial approach to the pituitary, pioneering intracranial trigeminal nerve sectioning for neuralgia, and the use of bone wax to stem bleeding from bone, to name but a few of his many accomplishments . According to Cushing , after Horsley was appointed surgeon to the “…National Hospital for the Paralyzed and Epileptic, Queen Square, the birth of modern neurologic surgery may properly be assumed to have taken place.”
Victor Horsley was present at what is widely considered the first modern brain tumor surgery. In 1884, Godlee, at the Hospital for Epilepsy and Paralysis in London, operated on a tumor that had been diagnosed and localized to the right motor cortex by the neurologist Bennett . Although brain tumors had been removed previously, Bennett’s localization of the tumor and Godlee’s first use of the antiseptic technique during tumor surgery made the case extraordinary. Using Bennett’s knowledge of neuroanatomy and pathophysiology, Godlee was able to plan his craniotomy directly over the tumor and easily removed the tumor, which turned out to be a glioma. The patient survived the immediate operation, but succumbed to purulent cerebritis a month later. The case is noteworthy for overcoming the third most challenging obstacle—following anesthesia and asepsis—that faced the development of neurosurgery: tumor localization. With this obstacle overcome, using the help of neurologists, such as Bennett, neurosurgical advances accelerated. Godlee’s case also is noteworthy from the standpoint of who attended the operation: the neurologist Hughlings Jackson and the neurosurgeons Victor Horsley and David Ferrier; Joseph Lister (Godlee’s uncle) was reported to be there as well .
Sir Charles Ballance: pioneering skull base surgeon
Along with Victor Horsley, Sir Charles Ballance ( Fig. 5 ) was another of the pioneering British neurologic surgeons. Neurotology and skull base surgery also can claim Ballance as one of its instrumental founders, based upon his landmark surgical advances within the temporal bone. Born in 1856 in Middlesex, England, Ballance entered medical school in 1875 at St. Thomas’ Hospital in London. As one of the stars of his medical school class, Ballance was taught by such eminent figures as Joseph Lister. Following his graduation, he traveled to Germany where he was taught by the leaders in medicine at that time, including Virchow, von Bergmann, Schwartze, and Trendelenburg. Ultimately, and perhaps reluctantly, specializing in ear surgery, Ballance returned to England where he was appointed Aural Surgeon at St. Thomas’ Hospital in London. In 1891 he was appointed as Surgeon to the National Hospital for the Paralyzed and Insane, Queen’s Square, where he became a colleague of Horsley. Ballance ultimately ended up as Surgeon-in-Charge of the Ear Department of St. Thomas’ Hospital .

Ballance’s accomplishments within the field of neurosurgery would become legendary. He helped to advance the science of cerebral localization along with the neurologists David Ferrier, Charles Beevor, and Charles Sherrington. He assisted Horsley in the first successful removal of an extramedullary spinal cord tumor; it is said that Ballance’s direction within the operation probably led to its success . In addition to these impressive advances are numerous groundbreaking contributions to neurotology and skull base surgery. Ballance was one of the first to popularize the radical mastoidectomy for advanced middle ear infections and was one of the first in England to advocate transmastoid drainage and ligation of the jugular vein for an infected, thrombosed lateral sinus ( Fig. 6 ). He improved the mastoidectomy by advocating lining the cavity with an epithelial graft, lowering the prevalence of postoperative infection . Although successful drainage of cerebellar otogenic abscesses were reported first by Schwartze in 1887 and later by Macewen in 1890, it was Ballance who first drained such an abscess by cerebellar localization, rather than following the infection from the mastoid . Ballance also devised a new method of gaining access to the cavernus sinus in cases of otic infection spread . Based upon these numerous accomplishments, Ballance rapidly ascended to become the premier surgeon in London for infectious diseases of the temporal bone.
As if these accomplishments were not enough, Ballance is credited with the first successful complete removal of an acoustic neuroma, performed in 1894 . Ballance also attempted division of the auditory nerve by way of a suboccipital approach for painful tinnitus. The operation also was noted for its use of electrical and mechanical stimulation of the exposed cranial nerves for clear auditory nerve identification. Although the operation was described as a success because “…the painful tinnitus had ceased,” the patient expired 1 year later. Additionally, Ballance performed landmark studies on the facial nerve, Bell’s palsy, and facial nerve grafting.
It is clear that Ballance was one of the greatest neurotologic and skull base surgeons in the history of the field. One of his landmark treatises, Essays on the Surgery of the Temporal Bone , written in 1919 , continues to have relevance, based upon his treatment paradigms, approach to temporal bone disease, and historical review of otology and temporal bone surgery.
Twentieth century
A tumor that helped defined a specialty: acoustic neuroma
It comes as no surprise that one of the most common tumors of the brain has played a pivotal role in the development of neurotology and skull base surgery. It also is not surprising that the surgeons who pioneered acoustic neuroma surgery throughout the twentieth century are considered the most influential surgeons of their era.
Although the first postmortem description of an acoustic neuroma was made in 1777 by Sandifort of Leyden University , it was not until nearly 200 years later that the first attempt was made at its removal. Encouraged by the success of Godlee’s operation using neurologic tumor localization and aseptic technique in 1884 , several attempts were made in the late 1800s to remove brain tumors that, following their removal, were diagnosed as acoustic neuromas. The first reported unsuccessful case (the patient died) of an acoustic tumor removal was by McBurney in 1891 . Clearly, the influence of the London school of neurosurgery, led by Horsley, had permeated New York by this time where McBurney was working, because in the report he described his use of tumor localization and its influence upon diagnosis and surgery. The first successful suboccipital resections of an acoustic neuroma were reported by Balance , and shortly after by Annandale .
Despite these early attempts and limited successes, mortality was high for tumor surgery; dissection was by finger, and hemostasis was achieved by packing. As reviewed by Jackler at an international conference of neurosurgeons, the mortality for these operations was 78%, and most survivors had serious disability; however, these statistics were changed radically by the most influential neurosurgeon of the twentieth century, Harvey Cushing.
Harvey Cushing: the founder of modern neurosurgery
There is perhaps no one in the annals of neurologic surgery about whom more has been written than Cushing, a man whose name is synonymous with the field.
Born the youngest of 10 children in a long line of physicians, Cushing followed his father, grandfather, great-grandfather, and great-great-grandfather’s path into medicine. After an undergraduate education at Yale University, he studied medicine at Harvard Medical School. Subsequently, he went to Johns Hopkins University to train under the pioneering surgeon Halsted, where he was exposed to the other medical icon of that era William Osler. From Johns Hopkins and later at Harvard, Cushing literally revolutionized the field of neurosurgery. He introduced the concept of meticulously documented anesthesia records and the use of continuous intraoperative blood pressure monitoring. He was perhaps the first surgeon to make regular use of the new technology of x-rays, including making the emulsions and developing the films himself. He described the “Cushing response,” the physiologic changes induced by an increase in intracranial pressure. He performed pioneering work in balanced salt solutions that led to modern intravenous therapy. He pioneered transsphenoidal pituitary surgery. He revolutionized surgical training by introducing canine surgery for medical students. He radically improved intracranial hemostasis with the development of surgical clips and electrocautery, and with it, drastically improved surgical morbidity during neurosurgical procedures .
In addition to these “technical” advances, Cushing radically changed the practice of surgery. Cushing insisted that surgeons take responsibility for their own diagnoses and decisions to operate, rather than rely upon medical physicians or neurologists . It was Cushing who made fashionable meticulous, anatomically based surgical technique, rather than reliance upon speed. Of course, this was made possible by his improved technical advances, such as hemostasis and insistence upon superior anesthesia. So pervasive was his instruction, that to this day, nearly all American-trained neurologic surgeons can trace their legacy back to Cushing.
Cushing’s advances within the field of skull base surgery are equally monumental, particularly with regard to the treatment of acoustic neuromas. After realizing that the tumors could not be removed completely by current standards, he advised intracapsular removal of the tumor and subtotal resection ( Fig. 7 ) . Combined with his other technical advances, this approach enabled Cushing to reduce surgical mortality from near 90% to 20%, as noted in his classic monograph, Tumors of the Nervus Acusticus and the Syndrome of the Cerebello-Pontine Angle , published in 1917.
By the time 1920 rolled around, Cushing had redefined the specialty of neurologic surgery, with its emphasis upon a strong foundation of neurologic training. According to Greenblatt and Smith , “…with further demonstration of his successes in training, in therapeutic results, and in research productivity, the Cushing model became the world model.”
Nylén, Holmgren, and the birth of the operating microscope
While Cushing was laying the foundations for modern neurologic surgery in America, two unassuming Swedish surgeons were developing a technology that ultimately revolutionized the fields of otology, neurotology, skull base surgery, and neurosurgery.
The operating microscope evolved out of the optics of the microscope originally pioneered by Robert Hooke and Antony van Leeuwenhoek in the mid-1600s. Yet, it was the inherent constraints of ear surgery that led to the development of a microscope uniquely suited to the operating room. Otology and neurotology were uniquely poised for this transition because of the difficulties imposed by the microscopic anatomy of the inner ear, limiting what ear surgeons could do by unmagnified eyesight alone. Further, with the development of improved anesthesia at the beginning of the twentieth century, the need for more precise surgical technique within otology, as championed by Cushing in neurosurgery, became paramount.
Carl-Olaf Nylén was an assistant in the University Otolaryngology Clinic in Stockholm under the chief Holmgren in the early 1920s. Prompted by Maier and Lion’s report of endolymph movements in the living pigeon using a low-power microscope, Nylén began work on a higher-power microscope that could be used during ear surgery. Such a device would have direct relevance to Nylén’s primary clinical interest of study: labyrinthine fistulas .
Nylén’s first monocular microscope was developed by the Brinnell-Leitz factory. Nylén later recalled his initial use of the microscope, “The idea of using a larger magnification than had previously been employed, occurred to me early in 1921 when I was experimenting with labyrinthine fistula operations on temporal bone preparations from human beings and in living animals…In November 1921 I used the Brinell microscope for observations and operations in two cases of chronic otitis with labyrinthine fistulas, and in one case with bilateral pseudo-fistula symptoms.” Nylén later modified the scope with the help of his friend and engineer Persson so it could mount on the patient more easily. These results were reported in 1922 at the meeting of the Swedish Otolaryngologic Society and in Paris in July of that same year.
Unfortunately, after his initial contribution of the monocular operating microscope, Nylén found himself unable to continue to develop the instrument in the clinic of his chief, Holmgren ( Fig. 8 ) , where tradition and custom dictated that the chief alone carried out the new, and still experimental, otosclerosis surgery, one of the primary applications of the new “otomicroscope.” Holmgren was already known for having introduced the operating loupes to ear surgery, and, thus, already had a substantial appreciation for the need of magnification during these procedures. After seeing his assistant Nylén use the operating microscope, Holmgren immediately recognized the added advantages of the microscope over loupes during these cases. Holmgren did not simply copy Nylén’s idea, he advanced it significantly, and gave ample credit for the idea to his assistant. In one of his publications, he stated, “…following a good idea of my 1. Assistant surgeon Dr. Nylén I tried a microscope and found the Zeiss binocular microscope a very suitable instrument…” To the Zeiss binocular, ophthalmologic scope, Holmgren added a light source and support suitable for the operating theater and began using it that same year, in 1922 (see Fig. 8 ). Compared with Nylén’s monocular scope, Holmgren had developed an entirely new and revolutionary binocular operating microscope.
In his initial description of the uses of the operating microscope in the temporal bone, Holmgren enthusiastically presaged its benefit in ear surgery, stating that the advantages of using the microscope for radical operations on otitis “…are indeed so obvious that no operator, who has had experience of the lens will give it up when doing this operation.” Holmgren’s words are prescient indeed, as any current otologic, neurotologic, skull base surgeon, or neurosurgeon will attest! Additionally, Holmgren used what he termed “…a little circular cutting file, viz., one driven by a little electro-motor of the type which is often used by dentists, armed with the very smallest drills obtainable, which are sufficiently small to make it possible that even very delicate bone operations can be carried out in the utmost safety under the guidance of the eye.” This was perhaps the first application of the drill for aural surgery and has to be regarded as a seminal event in the history of neurotology and skull base surgery.
Walter Dandy
At approximately the same time that Nylén and Holmgren were introducing the operating microscope to aural surgery, one of Cushing’s protégé’s was carrying on the transformation of neurosurgery started by his mentor. Walter Dandy (1886–1946), perhaps Cushing’s most accomplished student, was clearly responsible for ushering in the next great leap in neurotologic, neurosurgical, and skull base surgery.
Passing up a Rhodes Scholarship to enter Johns Hopkins Medical School, Dandy would go on to redefine the specialty of neurosurgery. After graduating medical school, he was appointed by Halsted to surgery, and spent his first year in the Hunterian Labs where Cushing was performing his physiologic experiments. There the two giants developed a contentious relationship almost from the start. At one point, Dandy accused Cushing of not being “…a real scientist” . Therefore, it is no surprise that when Cushing left Johns Hopkins to take over the new neurosurgical department at Brigham Hospital in Boston in 1912, Dandy was not asked to join the team .
If great minds truly do clash, then the squabbles between Cushing and Dandy should come as no surprise. For as much as Cushing transformed the landscape of neurologic surgery, Dandy would nearly rival his teacher’s accomplishments while at Johns Hopkins. Perhaps Dandy’s greatest accomplishment came while he was still in his training years. In 1918, he reported on ventriculography by the injection of air into the cerebral ventricles. The impact upon the field of neurosurgery was enormous, for it allowed the direct localization and size estimation of brain tumors for the first time. According to Horrax , “It brought immediately into the operable field at least one third more brain tumors than could be diagnosed and localized previously by the most refined neurological methods.” One year later, Dandy introduced pneumoencephalography.
Dandy’s influence upon neurotology and skull base surgery was equally profound. In 1917, he reported on the first successful total excision of an acoustic neuroma. Whereas Cushing had advocated leaving the capsule intact to minimize surrounding brain injury, bleeding, and facial paralysis, Dandy recommended total excision ( Fig. 9 ). This departure from his former teacher’s doctrine reportedly left Cushing infuriated . Subsequently, Dandy championed the suboccipital approach for complete acoustic neuroma resection with reports extending into the 1940s.
Dandy’s influence upon neurotology and skull base surgery did not end with his achievements in vestibular schwannoma resection; his impact upon the treatment of Ménière’s disease was equally important. Although Dandy stated that he initially began sectioning the whole VIIIth cranial nerve for patients who had vertigo as early as 1912, he started selectively sectioning the vestibular nerve beginning around 1930. By 1940, he published the results of the operation in more than 400 patients who had Ménière’s disease. Dandy was not the first to treat Ménière’s disease by dividing the VIIIth cranial nerve; this honor probably belongs to Parry , who reported on such a case using a middle fossa approach in 1902. Undoubtedly, the primitive state of neurologic surgery at the time, the outcome of Parry’s reported case (complete facial nerve paralysis), and the report of two other deaths from similar attempts at relieving vertigo dissuaded others from trying this treatment for some time. By the time of Dandy’s report in 1941, however, the procedure was far safer. As Dandy stated, “Ménière’s disease can be permanently cured by division of the auditory nerve. This procedure carries almost no risk to life. Up to the present time, I have performed 401 operations, with 1 death—the 358th case—due to meningitis.”
Terence Cawthorne and the rise of the transmastoid labyrinthectomy
Otologists of the 1930s and 1940s encountered a number of difficulties when attempting to perform Dandy’s surgery, most obvious being the unfamiliarity of neurosurgical anatomy . As a result, a variety of otologic operations were tried during this time to relieve patients of the severe symptoms of Ménière’s disease, including injections of alcohol through the horizontal canal or stapes footplate, electrocoagulation of the horizontal canal, or simply opening the labyrinth and suctioning the contents . It was the method of the British otologist Terence Cawthorne, however, that eventually became the new standard for treating Ménière’s disease in the 1940s and 1950s: the transmastoid labyrinthectomy.
Cawthorne (1902–1970) was universally acknowledged as one of the greatest ear surgeons in the mid-1900s . While serving on the staff of the National Hospital for Nervous Diseases and the Metropolitan Hospital in England, he began studying labyrinthine vertigo intensively. In 1943, Cawthorne introduced a transmastoid labyrinthectomy as a means of destroying the labyrinth and curing the symptoms of Ménière’s disease. The appeal to the otolaryngologic community was immediate. The mastoid operation was one that all otolaryngologists were familiar with already. As amply noted in this historical review, the mastoidectomy had become a widely accepted treatment for suppurative diseases of the ear and chronic otitis media since the 1860s. By the 1940s, all otolaryngology training programs included the mastoidectomy as a basic part of resident training, practiced essentially as it is today. Modifying the mastoid operation to include a labyrinthectomy was a simple step, and the transmastoid labyrinthectomy quickly became the preferred method for treating patients who had Ménière’s disease, surpassing the vestibular nerve section championed by Dandy.
Neurotologic surgery advances in the 1930s and 1940s: Maurice Sourdille, Julius Lempert, and the fenestration operation
Pioneering efforts to restore hearing to patients who had otosclerosis undeniably benefited the development of neurotology and skull base surgery. For the operation to succeed, it required improvements in aural operative technique and surgical microscopy, advances that ultimately were incorporated into neurotologic and skull base surgery. During the 1940s, two figures were prominent in the development of an effective surgical treatment for otosclerosis: Maurice Sourdille and Julius Lempert.
Although the lesser known of the two men, Maurice Sourdille’s impact upon the surgical treatment of otosclerosis was perhaps nearly as equally important. After studying at the University of Paris in 1911, he eventually became a pupil of Lermoyez, one of the most prominent otolaryngologists in France at that time. It was under Lermoyez’s tutelage that Sourdille developed his passion for hearing preservation surgery . Following World War I, Sourdille traveled to Sweden where he studied with Holmgren and Barany. There he witnessed first-hand the spectacular, although often short-lived, labyrinthine fenestration results with the microscope that Holmgren was achieving on patients who had otosclerosis. The high incidence of deafness eventually led Barany and Holmgren to abandon the procedure.
Sourdille recognized that the two principal drawbacks of Holmgren’s operation were closure of the fistula and the risk for infection. After experiments in the cadaver, Sourdille developed a three-stage procedure. He decided that the horizontal canal was the most accessible, and he closed the fistula with a thin cutaneous flap from the external auditory canal, which came to be known as “Sourdille’s flap” . Not only were his hearing results superior, the auditory improvement lasted. After Sourdille presented his results to the French Academy of Medicine in 1929, word quickly spread throughout Europe and the Americas, leading otologists and patients from around the world to seek out Sourdille.
According to Glasscock, Lempert ( Fig. 10 ) must be considered one of the three most pivotal ear surgeons of the twentieth century and the father of modern otologic surgery. According to Cawthorne , Lempert “…led the renaissance of otologic surgery and of otology as a science, at the very moment that antibiotics began to remove acute mastoid infections and their dread complications from the surgeon’s scalpel to the family doctor’s prescription pad.” His charm and charisma were legendary. Based largely upon Sourdille’s technique, Lempert developed the endaural approach to ear surgery , and popularized the drill in otologic surgery, as used by Holmgren before him. According to Glasscock , his exposure of the carotid artery during temporal bone surgery in 1938 was one of the seminal events of skull base surgery development.




