Anatomy & Embryology of the Eye: Introduction
A thorough understanding of the anatomy of the eye, orbit, visual pathways, upper cranial nerves, and central pathways for the control of eye movements is a prerequisite for proper interpretation of diseases having ocular manifestations. Furthermore, such anatomic knowledge is essential to the proper planning and safe execution of ocular and orbital surgery. Whereas most knowledge of these matters is based on anatomic dissections, either postmortem or during surgery, noninvasive techniques—particularly magnetic resonance imaging (MRI), ultrasonography, and optical coherence tomography (OCT)—are increasingly providing additional information. Investigating the embryology of the eye is clearly a more difficult area because of the relative scarcity of suitable human material, and thus there is still great reliance on animal studies, with the inherent difficulties in inferring parallels in human development. Nevertheless, a great deal is known about the embryology of the human eye, and—together with the recent expansion in molecular genetics—this has led to a much deeper understanding of developmental anomalies of the eye.
Normal Anatomy
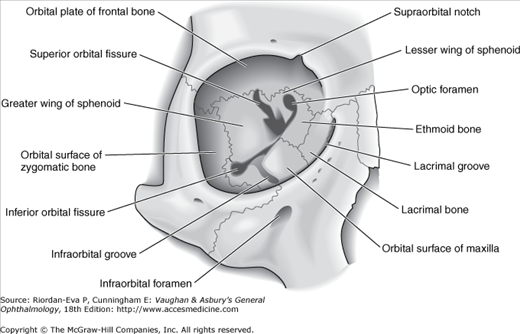
The orbital cavity is schematically represented as a pyramid of four walls that converge posteriorly. The medial walls of the right and left orbit are parallel and are separated by the nose. In each orbit, the lateral and medial walls form an angle of 45°, which results in a right angle between the two lateral walls. The orbit is compared to the shape of a pear, with the optic nerve representing its stem. The anterior circumference is somewhat smaller in diameter than the region just within the rim, which makes a sturdy protective margin.
The volume of the adult orbit is approximately 30 mL, and the eyeball occupies only about one-fifth of the space. Fat and muscle account for the bulk of the remainder.
The anterior limit of the orbital cavity is the orbital septum, which acts as a barrier between the eyelids and orbit (see Eyelids later in this chapter).
The orbits are related to the frontal sinus above, the maxillary sinus below, and the ethmoid and sphenoid sinuses medially. The thin orbital floor is easily damaged by direct trauma to the globe, resulting in a “blowout” fracture with herniation of orbital contents into the maxillary antrum. Infection within the sphenoid and ethmoid sinuses can erode the paper-thin medial wall (lamina papyracea) and involve the contents of the orbit. Defects in the roof (eg, neurofibromatosis) may result in visible pulsations of the globe transmitted from the brain.
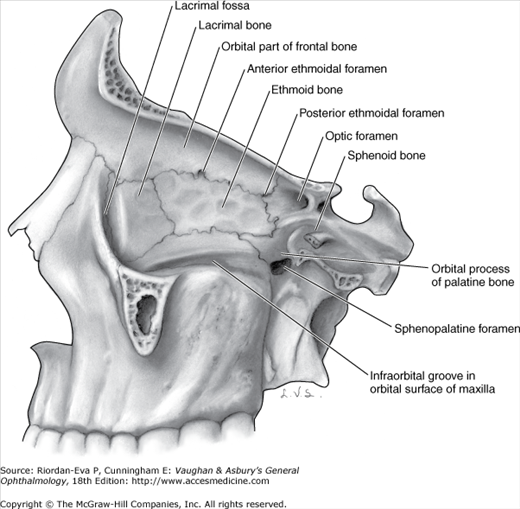
The roof of the orbit is composed principally of the orbital plate of the frontal bone. The lacrimal gland is located in the lacrimal fossa in the anterior lateral aspect of the roof. Posteriorly, the lesser wing of the sphenoid bone containing the optic canal completes the roof.
The lateral wall is separated from the roof by the superior orbital fissure, which divides the lesser from the greater wing of the sphenoid bone. The anterior portion of the lateral wall is formed by the orbital surface of the zygomatic (malar) bone. This is the strongest part of the bony orbit. Suspensory ligaments, the lateral palpebral tendon, and check ligaments have connective tissue attachments to the lateral orbital tubercle.
The orbital floor is separated from the lateral wall by the inferior orbital fissure. The orbital plate of the maxilla forms the large central area of the floor and is the region where blowout fractures most frequently occur. The frontal process of the maxilla medially and the zygomatic bone laterally complete the inferior orbital rim. The orbital process of the palatine bone forms a small triangular area in the posterior floor.
The boundaries of the medial wall are less distinct. The ethmoid bone is paper-thin but thickens anteriorly as it meets the lacrimal bone. The body of the sphenoid forms the most posterior aspect of the medial wall, and the angular process of the frontal bone forms the upper part of the posterior lacrimal crest. The lower portion of the posterior lacrimal crest is made up of the lacrimal bone. The anterior lacrimal crest is easily palpated through the lid and is composed of the frontal process of the maxilla. The lacrimal groove lies between the two crests and contains the lacrimal sac.
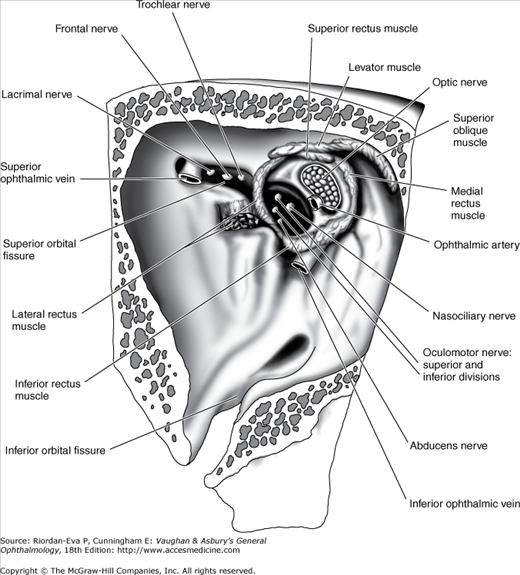
The apex of the orbit is the main portal for all nerves and vessels to the eye and the site of origin of all extraocular muscles except the inferior oblique. The superior orbital fissure lies between the body and the greater and lesser wings of the sphenoid bone. The superior ophthalmic vein and the lacrimal, frontal, and trochlear nerves pass through the lateral portion of the fissure that lies outside the annulus of Zinn. The superior and inferior divisions of the oculomotor nerve and the abducens and nasociliary nerves pass through the medial portion of the fissure within the annulus of Zinn. The optic nerve and ophthalmic artery pass through the optic canal, which also lies within the annulus of Zinn. The inferior ophthalmic vein frequently joins the superior ophthalmic vein before exiting the orbit. Otherwise, it may pass through any part of the superior orbital fissure, including the portion adjacent to the body of the sphenoid that lies inferomedial to the annulus of Zinn, or through the inferior orbital fissure.
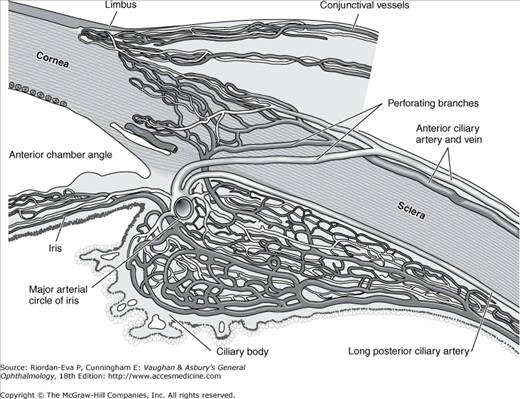
The principal arterial supply of the orbit and its structures derives from the ophthalmic artery, the first major branch of the intracranial portion of the internal carotid artery. This branch passes beneath the optic nerve and accompanies it through the optic canal into the orbit. The first intraorbital branch is the central retinal artery, which enters the optic nerve about 8–15 mm behind the globe. Other branches of the ophthalmic artery include the lacrimal artery, supplying the lacrimal gland and upper eyelid; muscular branches to the various muscles of the orbit; long and short posterior ciliary arteries; medial palpebral arteries to both eyelids; and the supraorbital and supratrochlear arteries. The short posterior ciliary arteries supply the choroid and parts of the optic nerve. The two long posterior ciliary arteries supply the ciliary body and anastomose with each other and with the anterior ciliary arteries to form the major arterial circle of the iris. The anterior ciliary arteries are derived from the muscular branches to the rectus muscles. They supply the anterior sclera, episclera, limbus, and conjunctiva and contribute to the major arterial circle of the iris. The most anterior branches of the ophthalmic artery contribute to the formation of the arterial arcades of the eyelids, which make an anastomosis with the external carotid circulation via the facial artery.
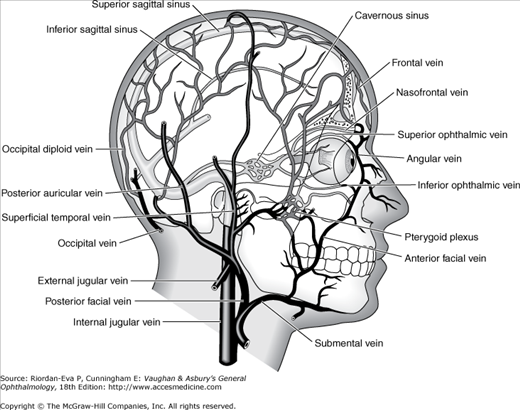
The venous drainage of the orbit is primarily through the superior and inferior ophthalmic veins, into which drain the vortex veins, the anterior ciliary veins, and the central retinal vein. The ophthalmic veins communicate with the cavernous sinus via the superior orbital fissure and the pterygoid venous plexus via the inferior orbital fissure. The superior ophthalmic vein is initially formed from the supraorbital and supratrochlear veins and from a branch of the angular vein, all of which drain the skin of the periorbital region. This provides a direct communication between the skin of the face and the cavernous sinus, thus forming the basis of the potentially lethal cavernous sinus thrombosis, secondary to superficial infection of the periorbital skin.
The normal adult globe is approximately spherical, with an anteroposterior diameter averaging 24 mm.
The conjunctiva is the thin, transparent mucous membrane that covers the posterior surface of the lids (the palpebral conjunctiva) and the anterior surface of the sclera (the bulbar conjunctiva). It is continuous with the skin at the lid margin (a mucocutaneous junction) and with the corneal epithelium at the limbus.
The palpebral conjunctiva lines the posterior surface of the lids and is firmly adherent to the tarsus. At the superior and inferior margins of the tarsus, the conjunctiva is reflected posteriorly (at the superior and inferior fornices) and covers the episcleral tissue to become the bulbar conjunctiva.
The bulbar conjunctiva is loosely attached to the orbital septum in the fornices and is folded many times. This allows the eye to move and enlarges the secretory conjunctival surface. (The ducts of the lacrimal gland open into the superior temporal fornix.) Except at the limbus (where Tenon’s capsule and the conjunctiva are fused for about 3 mm), the bulbar conjunctiva is loosely attached to Tenon’s capsule and the underlying sclera.
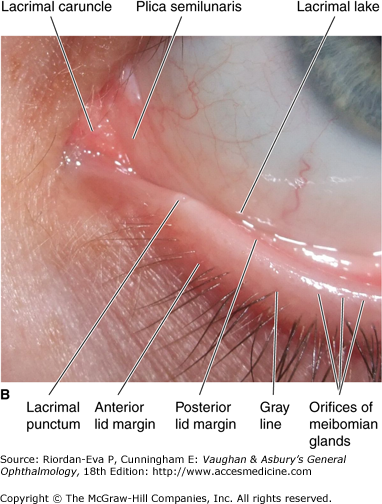
A soft, movable, thickened fold of bulbar conjunctiva (the semilunar fold) is located at the inner canthus and corresponds to the nictitating membrane of some lower animals. A small, fleshy, epidermoid structure (the caruncle) is attached superficially to the inner portion of the semilunar fold and is a transition zone containing both cutaneous and mucous membrane elements.
The conjunctival epithelium consists of two to five layers of stratified columnar epithelial cells—superficial and basal. Conjunctival epithelium near the limbus, over the caruncle, and near the mucocutaneous junctions at the lid margins consists of stratified squamous epithelial cells. The superficial epithelial cells contain round or oval mucus-secreting goblet cells. The mucus, as it forms, pushes aside the goblet cell nucleus and is necessary for proper dispersion of the precorneal tear film. The basal epithelial cells stain more deeply than the superficial cells and may contain pigment near the limbus.
The conjunctival stroma is divided into an adenoid (superficial) layer and a fibrous (deep) layer. The adenoid layer contains lymphoid tissue and in some areas may contain “follicle-like” structures without germinal centers. The adenoid layer does not develop until after the first 2 or 3 months of life. This explains why inclusion conjunctivitis of the newborn is papillary in nature rather than follicular and why it later becomes follicular. The fibrous layer is composed of connective tissue that attaches to the tarsal plate. This explains the appearance of the papillary reaction in inflammations of the conjunctiva. The fibrous layer is loosely arranged over the globe.
The accessory lacrimal glands (glands of Krause and Wolfring), which resemble the lacrimal gland in structure and function, are located in the stroma. Most of the glands of Krause are in the upper fornix, and the remaining few are in the lower fornix. The glands of Wolfring lie at the superior margin of the upper tarsus.
The conjunctival arteries are derived from the anterior ciliary and palpebral arteries. The two arteries anastomose freely and—along with the numerous conjunctival veins that generally follow the arterial pattern—form a considerable conjunctival vascular network. The conjunctival lymphatics are arranged in superficial and deep layers and join with the lymphatics of the eyelids to form a rich lymphatic plexus. The conjunctiva receives its nerve supply from the first (ophthalmic) division of the fifth nerve. It possesses a relatively small number of pain fibers.
Tenon’s capsule is a fibrous membrane that envelops the globe from the limbus to the optic nerve (Figure 1–19). Adjacent to the limbus, the conjunctiva, Tenon’s capsule, and episclera are fused together. More posteriorly, the inner surface of Tenon’s capsule lies against the sclera, and its outer aspect is in contact with orbital fat and other structures within the extraocular muscle cone. At the point where Tenon’s capsule is pierced by tendons of the extraocular muscles in their passage to their attachments to the globe, it sends a tubular reflection around each of these muscles. These fascial reflections become continuous with the fascia of the muscles, the fused fasciae sending expansions to the surrounding structures and to the orbital bones. The fascial expansions are quite tough and limit the action of the extraocular muscles, and are therefore known as check ligaments (Figure 1–20). They regulate the direction of action of the extraocular muscles and may act as their functional mechanical origins, possibly with active neuronal control (active pulley hypothesis). The lower segment of Tenon’s capsule is thick and fuses with the fascia of the inferior rectus and the inferior oblique muscles to form the suspensory ligament of the eyeball (Lockwood’s ligament), upon which the globe rests.
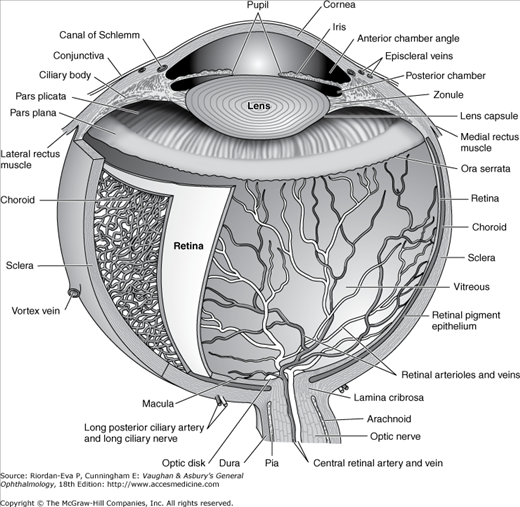
The sclera is the fibrous outer protective coating of the eye, consisting almost entirely of collagen (Figure 1–7). It is dense and white, and continuous with the cornea anteriorly and the dural sheath of the optic nerve posteriorly. Across the posterior scleral foramen are bands of collagen and elastic tissue, forming the lamina cribrosa, between which pass the axon bundles of the optic nerve. The outer surface of the anterior sclera is covered by a thin layer of fine elastic tissue, the episclera, which contains numerous blood vessels that nourish the sclera. The brown pigment layer on the inner surface of the sclera is the lamina fusca, which forms the outer layer of the suprachoroidal space.
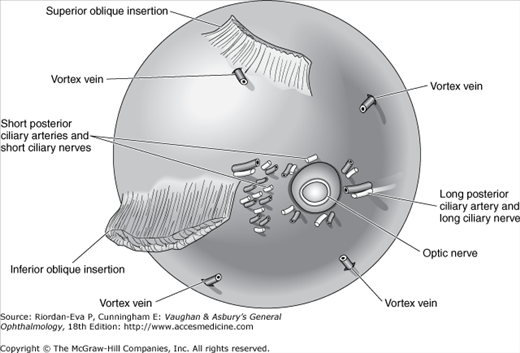
At the insertion of the rectus muscles, the sclera is about 0.3 mm thick; elsewhere it is about 0.6 mm thick. Around the optic nerve, the sclera is penetrated by the long and short posterior ciliary arteries and the long and short ciliary nerves (Figure 1–8). The long posterior ciliary arteries and long ciliary nerves pass from the optic nerve to the ciliary body in a shallow groove on the inner surface of the sclera at the 3 and 9 o’clock meridians. Slightly posterior to the equator, the four vortex veins draining the choroid exit through the sclera, usually one in each quadrant. About 4 mm posterior to the limbus, slightly anterior to the insertion of the respective rectus muscle, the four anterior ciliary arteries and veins penetrate the sclera. The nerve supply to the sclera is from the ciliary nerves.
Histologically, the sclera consists of many dense bands of parallel and interlacing collagen bundles, each of which is 10–16 μm thick and 100–140 μm wide. The histologic structure of the sclera is remarkably similar to that of the corneal stroma (see the next section) but it is opaque rather than transparent because of irregularity of the collagen lamellae, higher water content, and less proteoglycans.
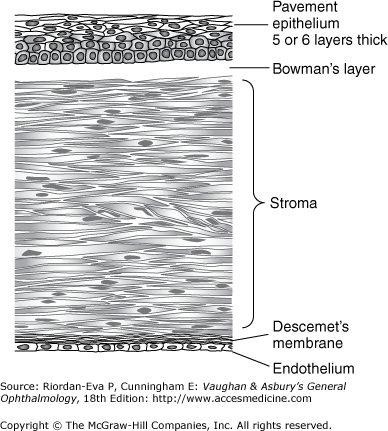
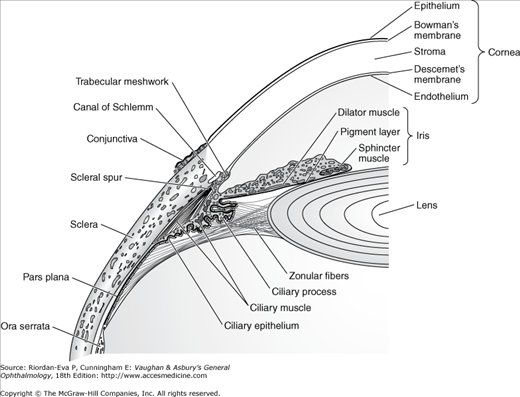
The cornea is a transparent tissue comparable in size and structure to the crystal of a small wristwatch (Figure 1–9). It is inserted into the sclera at the limbus, the circumferential depression at this junction being known as the scleral sulcus. The average adult cornea is 550 μm thick in the center, although there are racial variations, and about 11.7 mm in diameter horizontally and 10.6 mm vertically. From anterior to posterior, it has five distinct layers (Figure 1–10): the epithelium (which is continuous with the epithelium of the bulbar conjunctiva), Bowman’s layer, the stroma, Descemet’s membrane, and the endothelium. The epithelium has five or six layers of cells. Bowman’s layer is a clear acellular layer, a modified portion of the stroma. The corneal stroma accounts for about 90% of the corneal thickness. It is composed of intertwining lamellae of collagen fibrils 10–250 μm in width and 1–2 μm in height that run almost the full diameter of the cornea. They run parallel to the surface of the cornea and by virtue of their regularity, are optically clear. The lamellae lie within a ground substance of hydrated proteoglycans in association with the keratocytes that produce the collagen and ground substance. Descemet’s membrane, constituting the basal lamina of the corneal endothelium, has a homogeneous appearance on light microscopy but a laminated appearance on electron microscopy due to structural differences between its prenasal and postnatal portions. It is about 3 μm thick at birth but increases in thickness throughout life, reaching 10–12 μm in adulthood. The endothelium has only one layer of cells, but this is responsible for maintaining the essential deturgescence of the corneal stroma. The endothelium is quite susceptible to injury as well as undergoing loss of cells with age: the normal density reducing from 23,000 cells/mm2 at birth to 2000 cells/mm2 in old age. Endothelial repair is limited to enlargement and sliding of existing cells, with little capacity for cell division. Failure of endothelial function leads to corneal edema.
Sources of nutrition for the cornea are the vessels of the limbus, the aqueous, and the tears. The superficial cornea also gets most of its oxygen from the atmosphere. The sensory nerves of the cornea are supplied by the first (ophthalmic) division of the fifth (trigeminal) cranial nerve.
The transparency of the cornea is due to its uniform structure, avascularity, and deturgescence.
The uveal tract is composed from anterior to posterior of the iris, the ciliary body, and the choroid (Figure 1–7). It is the middle vascular layer of the eye and is protected by the cornea and sclera. It contributes blood supply to the retina.
The iris is a shallow cone pointing anteriorly with a centrally situated round aperture, the pupil. It is positioned in front of the lens, dividing the anterior chamber from the posterior chamber, each of which contains aqueous humor that passes through the pupil. There are no epithelial cells covering the anterior stroma. The sphincter and dilator muscles develop from the anterior epithelium, which covers the posterior surface of the stroma and represents an anterior extension of the retinal pigment epithelium. The heavily pigmented posterior epithelium represents an anterior extension of the neuroretina.
The arterial blood supply to the iris is from the major circle of the iris (Figure 1–4). Iris capillaries have a nonfenestrated endothelium, and hence do not normally leak intravenously injected fluorescein. Sensory nerve supply to the iris is via fibers in the ciliary nerves.
The iris controls the amount of light entering the eye. Pupillary size is principally determined by a balance between constriction due to parasympathetic activity transmitted via the third cranial nerve and dilation due to sympathetic activity (see Chapter 14).
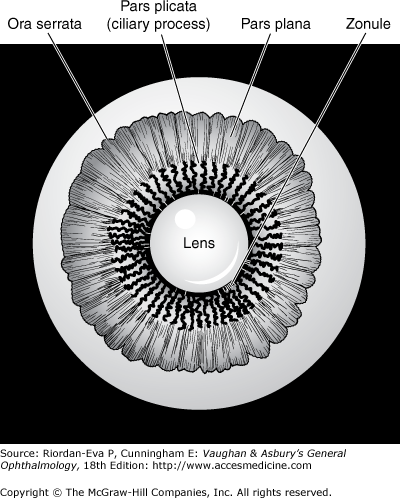
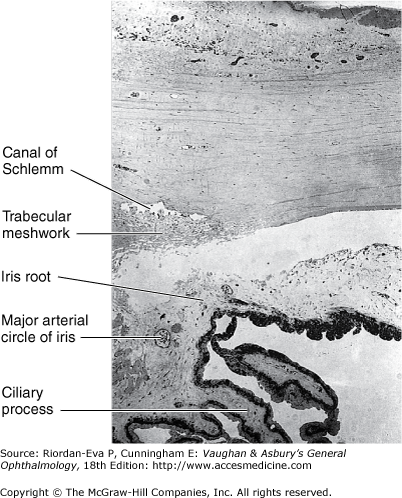
The ciliary body, roughly triangular in cross section, extends forward from the anterior end of the choroid to the root of the iris (about 6 mm). It consists of a corrugated anterior zone, the pars plicata (2 mm), and a flattened posterior zone, the pars plana (4 mm). The ciliary processes arise from the pars plicata (Figure 1–11). They are composed mainly of capillaries and veins that drain through the vortex veins. The capillaries are large and fenestrated, and hence leak intravenously injected fluorescein. There are two layers of ciliary epithelium: an internal nonpigmented layer, representing the anterior extension of the neuroretina, and an external pigmented layer, representing an extension of the retinal pigment epithelium. The ciliary processes and their covering ciliary epithelium are responsible for the formation of aqueous.
The ciliary muscle is composed of a combination of longitudinal, radial, and circular fibers. The function of the circular fibers is to contract and relax the zonular fibers, which originate in the valleys between the ciliary processes (Figure 1–12). This alters the tension on the capsule of the lens, giving the lens a variable focus for both near and distant objects in the visual field. The longitudinal fibers of the ciliary muscle insert into the trabecular meshwork to influence its pore size.
The arterial blood supply to the ciliary body is derived from the major circle of the iris. The nerve supply is via the short ciliary nerves.
The choroid is the posterior segment of the uveal tract, between the retina and the sclera. It is composed of three layers of choroidal blood vessels: large, medium, and small. The deeper the vessels are placed in the choroid, the wider their lumens (Figure 1–13). The internal portion of the choroid vessels is known as the choriocapillaris. Blood from the choroidal vessels drains via the four vortex veins, one in each of the four posterior quadrants. The choroid is bounded internally by Bruch’s membrane and externally by the sclera. The suprachoroidal space lies between the choroid and the sclera. The choroid is firmly attached posteriorly to the margins of the optic nerve. Anteriorly, the choroid joins with the ciliary body.
The aggregate of choroidal blood vessels serves to nourish the outer portion of the retina (Figure 1–4). The nerve supply to the choroid is via the ciliary nerves.
The lens is a biconvex, avascular, colorless, and almost completely transparent structure, about 4 mm thick and 9 mm in diameter. It is suspended behind the iris by the zonule, which connects it with the ciliary body. Anterior to the lens is the aqueous; posterior to it, the vitreous.
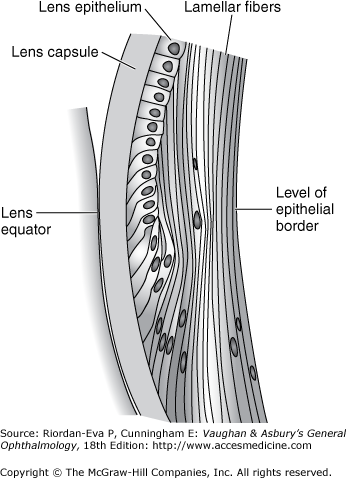
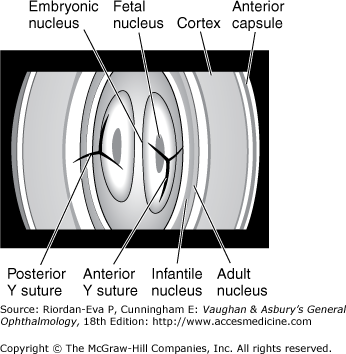
The lens capsule (see The Vitreous later in the chapter) is a semipermeable membrane (slightly more permeable than a capillary wall) that will admit water and electrolytes. A subcapsular epithelium is present anteriorly (Figure 1–14). With age, subepithelial lamellar fibers are continuously produced, so that the lens gradually becomes larger and less elastic throughout life. The nucleus and cortex are made up of long concentric lamellae, the lens nucleus being harder than the cortex. The suture lines formed by the end-to-end joining of these lamellar fibers are Y-shaped when viewed with the slitlamp (Figure 1–15). The Y is upright anteriorly and inverted posteriorly.