This article aims to help physicians and allergy care providers understand: the role of environmental control in the treatment of allergic disease; the concept of “the inflammatory load”; current published studies on environmental control; factors that influence levels of indoor and outdoor allergens; different methods to decrease patients’ exposure to indoor and outdoor allergens; problems related to nonallergic symptom triggers; special considerations for school and workplace avoidance; role of environmental control in the prevention of allergic disease; various products available on the market to assist in avoidance; and how to plan with the patient to implement environmental control strategies.
- •
Environmental control strategies prove a strong foundation for further allergy management
- •
There are many sources, besides true allergens, that may contribute to the “inflammatory load”
- •
Decreasing a patient’s exposure to outdoor allergens is a realistic goal
- •
The impact of indoor allergens on the patient’s symptoms should be considered, both at home and in the school or workplace
- •
The Focus of avoidance strategies is on “reducing” levels of allergens, rather than “eliminating” them
- •
Patients should be provided with a written copy of all recommendations, which should be reviewed often and kept simple.
This information is designed to help physicians and allergy care providers understand:
- •
The role of environmental control in the treatment of allergic disease
- •
The concept of “the inflammatory load”
- •
The current studies that have been published on environmental control
- •
The factors that influence levels of indoor and outdoor allergens
- •
Different methods to decrease a patient’s exposure to indoor and outdoor allergens
- •
The problems related to nonallergic symptom triggers
- •
Special considerations for school and workplace avoidance
- •
The role of environmental control in the prevention of allergic disease
- •
The various products available on the market to assist in avoidance
- •
How to make a plan with the patient to implement environmental control strategies.
Once the diagnosis of allergy has been made, the next step is to discuss environmental control strategies, also referred to as avoidance, with the patient. It is best to have this conversation after reviewing the results of specific allergy testing, either through skin or blood testing, but it is also reasonable to discuss these strategies based on the history alone. Most of them carry very little risk.
Nevertheless, there is often a great deal of resistance to initiating these strategies, on the part of both the physician and the patient. Discussing avoidance takes a great deal of time out of the physician’s busy schedule. The physician may also not be very familiar with these strategies or has read studies that fail to demonstrate a significant benefit. Many patients are already under the erroneous impression that there is nothing that can be done for allergies, and this is compounded by the commonly held belief that avoidance does not work. For those patients searching for a quick and easy method to relieve their allergy symptoms, a discussion about these strategies is the last thing they want to hear.
It is universally accepted that allergen exposure is a precursor to sensitization, and there are many situations in which the benefits of environmental control are undeniable. If the allergic reaction is immediate and dramatic, the patient will intuitively link the exposure with the symptom and begin practicing environmental control strategies, such as avoiding a home where a cat is present or by staying indoors on a hot, windy day. But in other situations the reactions may be delayed, related to multiple exposures, or more difficult to recognize when symptoms are chronic.
Most of the current studies designed at quantifying the benefits of environmental control for allergic rhinitis have been low-power studies with inconsistent follow-up periods, variability in patient populations, and a lack of blinding. The 2010 review by the Cochrane Collaboration on dust mite avoidance measures concluded that they “may be of some benefit in reducing rhinitis symptoms,” but the evidence was not strong. In addition, most of these studies have looked at only one isolated intervention, whereas the genetic and environmental complexities of allergic rhinitis and asthma most likely require a multifaceted treatment approach.
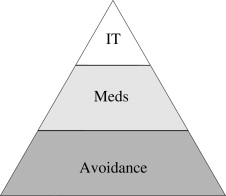
Conceptually, the management of allergies can be thought of as a pyramid with 3 levels ( Fig. 1 ). The classic triad of allergy management includes environmental control, pharmacotherapy, and immunotherapy. Environmental control forms the foundation of this pyramid, but it is actually not a treatment for allergic inflammation. Rather, it is a strategy to prevent further inflammation. Allergic symptoms may continue to gain momentum beyond the period of exposure, a phenomenon known as the “priming” effect, and for this reason avoidance alone may not seem to help at first. Every structure needs a strong foundation, but a person cannot live in the foundation alone. Environmental control sets the stage for effective treatment with pharmacotherapy and possibly immunotherapy, and for this reason, “there is no avoiding avoidance!”
Concept of the “inflammatory load”
To understand how allergen avoidance can help the allergic patient, one must first understand the concept of the “inflammatory load.” The inflammatory load represents the sum of all allergens, irritants, and other immune stimulators that a patient is exposed to at any given time. When the inflammatory load is high, so are the levels of circulating allergic and inflammatory mediators. In this situation, small challenges with other stimulators may result in worsening symptoms. Direct contributors to the inflammatory load may enter the body through the respiratory tract, digestive tract, or skin. Indirect contributors to the inflammatory load include illness, stress, or problems with mucosal barriers such as high gastrointestinal permeability and IgA deficiency.
Everything that contributes to the allergic load raises the level of inflammation toward a critical threshold, much like water being added to a bucket. When the level rises above the rim, water begins to spill out and the patient becomes symptomatic. The role of avoidance is to slow down the flow of water from that source, keeping the level below the threshold. This analogy helps explain why avoiding one or two antigens can increase a patient’s tolerance to other antigens that the patient is not actively avoiding. If needed, pharmacotherapy and immunotherapy may be used to increase the patient’s overall threshold which, in effect, gives that patient a larger bucket.
Outdoor allergens
Patients are often dismayed upon learning that they are allergic to outdoor allergens because they believe that for such allergies nothing can be done. Although the outdoor environment cannot be changed, the focus for these patients is on recognizing when to enter that environment and preventing those allergens from entering the indoor environment. In order for pollen to be allergenic, it must satisfy the criteria set forth in 1931 by A.A. Thommen ( Box 1 ).
In order for pollen to produce allergic symptoms, it must:
- •
Come from a seed-bearing plant
- •
Be produced in large amounts
- •
Be buoyant enough to allow for airborne spread
- •
Be widely distributed, particularly near areas of human habitation
- •
Have sensitizing potential
- •
Pollen
Pollen represents the male reproductive cells of most plants. Pollens are lightweight proteins, which may travel for many miles on the wind; they are relatively large in size, ranging from 15 to 50 μm, which does not allow them to easily penetrate the lower airway. In the Northern parts of the United States, trees pollinate from February through May, grasses pollinate from June through July, and weeds pollinate from August until the first frost of the year. Three consecutive days with temperatures above 65°F (18.5°C) allow for pollination. The pollination season is longer in warmer climates, and the phenomenon of global warming may also extend the time pollen is normally in the air.
Patients will use many names to describe their pollen allergies.
“Rose fever” is a term commonly applied to springtime allergies, but the pollen from brightly colored flowers is spread by insects and, therefore, does not enter the respiratory tract. This process is known as entemophilous spread, as opposed to airborne, or anemophilous, spread. Keep in mind that patients may still develop nasal symptoms from the odor of blooming flowers.
“Hayfever” is a term often applied to fall allergies, when hay is being harvested, but the true offender is ragweed. In the springtime, many patients notice a yellow coating of pine tree pollen on their cars and become convinced that this is what they are allergic to. This heavy pollen is actually not very allergenic because it does not remain airborne for long enough to cause symptoms. It is a clear sign, however, that pollination is actively occurring.
Patients who are allergic to pollen suffer most on hot, dry, windy days. Pollen counts tend to be highest from 5 to 10 am. If possible, patients should shift activities, such as running or gardening, from the morning to the evening during their active season; they should limit yard work and wear a mask when working outside. Patients should also be instructed to close their windows before going to bed and open the doors and windows only for limited times during the day when necessary. Even basic air-conditioning filters are able to filter out large pollen particles, and this appliance should be used as much as possible, either on the “cool” or “vent” settings. For those patients commuting to work in the morning, they should close the car windows and use the recirculation feature of the air-ventilation system, if present.
Patients should be advised to remove their clothes and shower immediately when they return home at night, particularly after being in the park or hiking in the woods. Pollen may stick to the clothing, skin, and hair, and may be particularly problematic in patients with long hair. The clothing should be placed in a hamper or a closet that is not in the bedroom, but never placed on the bed. The bedroom needs to be the patient’s “safe haven,” the one place in the house where there is a low level of allergens. Washing bed sheets and pillowcases in hot water frequently during the season will help accomplish this. Outdoor pets should also be kept out of the bedroom and should be washed after spending extended time outdoors. After showering, patients should change into clothing that is not worn outdoors.
Many patients who are allergic to pollens discover that when they travel to other regions their allergies improve, and they may be tempted to relocate to that region. In the past this was one recommendation for the treatment of pollen allergies, but is generally not practical nowadays. If the patient does intend to relocate, they must be informed that the genetic ability to form allergies to pollen in the environment will surely move with them. Patients may experience relief for the first few years depending on their new environment, but this “holiday” from allergies may begin to fade as they develop new sensitivities.
Mold
Mold is a ubiquitous organism on the Earth, which is found in both the indoor and outdoor environments. Mold spores are present in the air throughout the year, unless the ground is covered by snow, and outdoor spore counts are about twice as high as indoor levels. Spores are able to survive freezing and boiling, and may range in size from 5 to 50 μm. In general, particles less than 10 μm are able to gain access to the lower airway, and this explains why mold is a potent trigger for asthma. Both the spores and the fragments of mycelia are allergenic.
Mold requires warmth, moisture, and organic debris to grow. It is attracted to damp, shady areas where decaying vegetation is present. Spore counts peak after the sun sets, and therefore cause more symptoms during the evening as opposed to the morning for pollen-allergic patients. Many patients believe that they are allergic to grass because they are symptomatic after cutting the lawn. Although the grass in the lawn is typically too short to pollinate, the clippings that stick to the blade on the underside of the lawnmower are a perfect medium for mold growth. When the lawnmower is started again, the mold particles are propelled into the air.
Although mold is a perennial allergen, there are seasonal spikes that might fool the patient and clinician into thinking that pollen is the offending allergen. In colder climates, when snow begins to thaw in the early spring, many of the mold spores that have been dormant for the entire winter suddenly become airborne. Because of the rain seen in the late spring, early summer is also a time when airborne mold spores are elevated. During the fall, the leaves decaying on the ground also serve as a perfect medium for mold growth. Mold counts are generally higher in areas near stagnant bodies of water, such as lakes or marshes.
It is not possible to eliminate mold from the outdoor environment, but performing regular surveys around the exterior home and surrounding property is a good way to recognize trouble spots. Steps should be taken to thin out dense vegetation that is close to the house or lying on the roof. Any trees and bushes that are dead or decaying near the house should be removed and leaves raked away from the foundation. Firewood should be moved away from the house. The roof must be inspected for any holes or signs of excessive wear, and any leaky gutters or improperly installed flashing repaired. Water should be diverted away from the foundation and any low-lying areas filled in. Professional masons and landscapers may be needed to get the job done properly.
Outdoor allergens
Patients are often dismayed upon learning that they are allergic to outdoor allergens because they believe that for such allergies nothing can be done. Although the outdoor environment cannot be changed, the focus for these patients is on recognizing when to enter that environment and preventing those allergens from entering the indoor environment. In order for pollen to be allergenic, it must satisfy the criteria set forth in 1931 by A.A. Thommen ( Box 1 ).
In order for pollen to produce allergic symptoms, it must:
- •
Come from a seed-bearing plant
- •
Be produced in large amounts
- •
Be buoyant enough to allow for airborne spread
- •
Be widely distributed, particularly near areas of human habitation
- •
Have sensitizing potential
- •
Pollen
Pollen represents the male reproductive cells of most plants. Pollens are lightweight proteins, which may travel for many miles on the wind; they are relatively large in size, ranging from 15 to 50 μm, which does not allow them to easily penetrate the lower airway. In the Northern parts of the United States, trees pollinate from February through May, grasses pollinate from June through July, and weeds pollinate from August until the first frost of the year. Three consecutive days with temperatures above 65°F (18.5°C) allow for pollination. The pollination season is longer in warmer climates, and the phenomenon of global warming may also extend the time pollen is normally in the air.
Patients will use many names to describe their pollen allergies.
“Rose fever” is a term commonly applied to springtime allergies, but the pollen from brightly colored flowers is spread by insects and, therefore, does not enter the respiratory tract. This process is known as entemophilous spread, as opposed to airborne, or anemophilous, spread. Keep in mind that patients may still develop nasal symptoms from the odor of blooming flowers.
“Hayfever” is a term often applied to fall allergies, when hay is being harvested, but the true offender is ragweed. In the springtime, many patients notice a yellow coating of pine tree pollen on their cars and become convinced that this is what they are allergic to. This heavy pollen is actually not very allergenic because it does not remain airborne for long enough to cause symptoms. It is a clear sign, however, that pollination is actively occurring.
Patients who are allergic to pollen suffer most on hot, dry, windy days. Pollen counts tend to be highest from 5 to 10 am. If possible, patients should shift activities, such as running or gardening, from the morning to the evening during their active season; they should limit yard work and wear a mask when working outside. Patients should also be instructed to close their windows before going to bed and open the doors and windows only for limited times during the day when necessary. Even basic air-conditioning filters are able to filter out large pollen particles, and this appliance should be used as much as possible, either on the “cool” or “vent” settings. For those patients commuting to work in the morning, they should close the car windows and use the recirculation feature of the air-ventilation system, if present.
Patients should be advised to remove their clothes and shower immediately when they return home at night, particularly after being in the park or hiking in the woods. Pollen may stick to the clothing, skin, and hair, and may be particularly problematic in patients with long hair. The clothing should be placed in a hamper or a closet that is not in the bedroom, but never placed on the bed. The bedroom needs to be the patient’s “safe haven,” the one place in the house where there is a low level of allergens. Washing bed sheets and pillowcases in hot water frequently during the season will help accomplish this. Outdoor pets should also be kept out of the bedroom and should be washed after spending extended time outdoors. After showering, patients should change into clothing that is not worn outdoors.
Many patients who are allergic to pollens discover that when they travel to other regions their allergies improve, and they may be tempted to relocate to that region. In the past this was one recommendation for the treatment of pollen allergies, but is generally not practical nowadays. If the patient does intend to relocate, they must be informed that the genetic ability to form allergies to pollen in the environment will surely move with them. Patients may experience relief for the first few years depending on their new environment, but this “holiday” from allergies may begin to fade as they develop new sensitivities.
Mold
Mold is a ubiquitous organism on the Earth, which is found in both the indoor and outdoor environments. Mold spores are present in the air throughout the year, unless the ground is covered by snow, and outdoor spore counts are about twice as high as indoor levels. Spores are able to survive freezing and boiling, and may range in size from 5 to 50 μm. In general, particles less than 10 μm are able to gain access to the lower airway, and this explains why mold is a potent trigger for asthma. Both the spores and the fragments of mycelia are allergenic.
Mold requires warmth, moisture, and organic debris to grow. It is attracted to damp, shady areas where decaying vegetation is present. Spore counts peak after the sun sets, and therefore cause more symptoms during the evening as opposed to the morning for pollen-allergic patients. Many patients believe that they are allergic to grass because they are symptomatic after cutting the lawn. Although the grass in the lawn is typically too short to pollinate, the clippings that stick to the blade on the underside of the lawnmower are a perfect medium for mold growth. When the lawnmower is started again, the mold particles are propelled into the air.
Although mold is a perennial allergen, there are seasonal spikes that might fool the patient and clinician into thinking that pollen is the offending allergen. In colder climates, when snow begins to thaw in the early spring, many of the mold spores that have been dormant for the entire winter suddenly become airborne. Because of the rain seen in the late spring, early summer is also a time when airborne mold spores are elevated. During the fall, the leaves decaying on the ground also serve as a perfect medium for mold growth. Mold counts are generally higher in areas near stagnant bodies of water, such as lakes or marshes.
It is not possible to eliminate mold from the outdoor environment, but performing regular surveys around the exterior home and surrounding property is a good way to recognize trouble spots. Steps should be taken to thin out dense vegetation that is close to the house or lying on the roof. Any trees and bushes that are dead or decaying near the house should be removed and leaves raked away from the foundation. Firewood should be moved away from the house. The roof must be inspected for any holes or signs of excessive wear, and any leaky gutters or improperly installed flashing repaired. Water should be diverted away from the foundation and any low-lying areas filled in. Professional masons and landscapers may be needed to get the job done properly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


