30
Age-Related Macular Degeneration
Jie Jin Wang  Ronald Klein
Ronald Klein
Age-related macular degeneration (AMD), also termed age-related maculopathy (ARM), is the leading cause of irreversible blindness and visual impairment in older persons, and will remain a major threat to vision in coming decades (1). Research on AMD has progressed rapidly in recent decades (2–9). In particular, the identification of genetic variants responsible for AMD susceptibility (6, 7, 10–12) and environmental risk or protective factors for AMD, has pointed to likely pathogenetic mechanisms for this condition (7, 9, 13–15).
PREVALENCE AND INCIDENCE OF AGE-RELATED MACULAR DEGENERATION
In the last two decades there has been a growing number of large population-based studies conducted in different countries, providing estimates of AMD prevalence (16–33) and incidence (34–48).
AGE-RELATED MACULAR DEGENERATION PREVALENCE IN WHITES
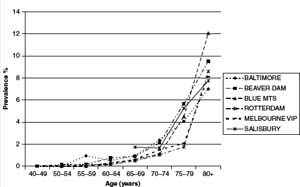
The meta-analysis conducted by the Eye Disease Prevalence Research Group (49), using data collected from multiple populations, including the Baltimore Eye Survey (20), the Beaver Dam Eye Study (BDES) (16) and the Salisbury Eye Evaluation (SEE) project (50) in the USA, the Rotterdam Study (RS) (17) in the Netherlands, and the Blue Mountains Eye Study (BMES) (18) and Visual Impairment Project (VIP) (22) in Australia, showed high consistency in the age-specific prevalence of late AMD (Fig. 30-1) and large soft drusen (≥125 μm in diameter) (Fig. 30-2) in whites. The prevalence of late AMD (geographic atrophy and neovascular AMD) increased exponentially with increasing age, rising from less than 0.5% at age 60 years to around 10% at age 80≶ years (49) (Fig. 30-1). The prevalence of large drusen showed a similar age-related increasing trend but the association with age is more linear than exponential (49) (Fig. 30-2). The natural course of AMD (involving the disappearance of large drusen associated with the progression to a more advanced AMD stage with aging (36) could explain the observed age-related linear (rather than exponential) pattern in the prevalence of large drusen.
AGE-RELATED MACULAR DEGENERATION PREVALENCE IN OTHER RACES AND ETHNICITIES
Ethnic variation in the prevalence of AMD and AMD lesions was observed in studies with multiracial groups such as the Baltimore Eye Survey (20), National Health and Nutrition Examination Survey (NHANES III) (51) and the Multi-Ethnic Study of Atherosclerosis (MESA) (33), and was previously summarized from studies conducted prior to this century (52).
Blacks
Findings from the Baltimore Eye Survey (20), and the Barbados Eye Study (53) which examined a sample of blacks, have suggested that the prevalence of some AMD lesions, particularly late AMD, is lower in blacks than in whites. The same observation has been consistently reported by a number of studies conducted in populations in the USA (21, 23, 33, 50). Possible selection bias may have occurred in some studies due to either low participation rate (21), a high proportion with ungradable retinal photographs (20, 21, 23), or poor survival in the eldest among black participants (20). Other factors may also be responsible for the racial variations in AMD frequency, including choroidal melanin density (23) and gene polymorphisms that may predispose whites to a more severe AMD than blacks (19, 20).
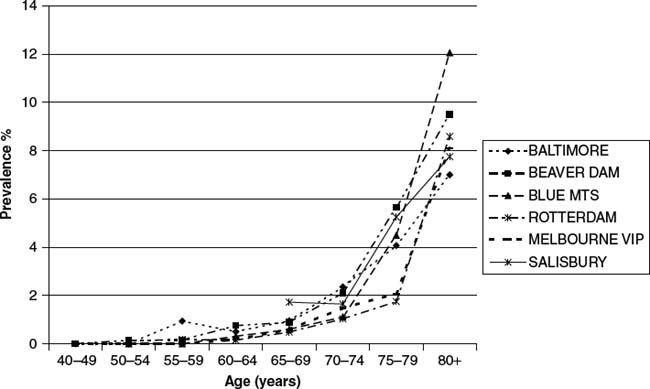
Figure 30-1. Prevalence of late ARMD by age in whites. (Reproduced from the Eye Disease Prevalence Research Group report, Friedman DS, O’Colmain BJ, Munoz B, et al. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol 2004;122:564–572.)
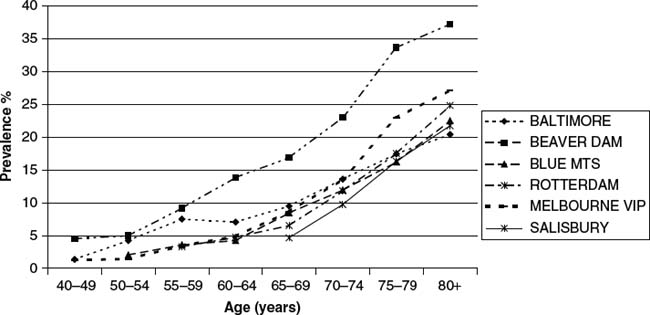
Figure 30-2. Prevalence of large drusen (≥125 µm in diameter) by age in whites. (Reproduced from the Eye Disease Prevalence Research Group report, Friedman DS, O’Colmain BJ, Munoz B, et al. Prevalence of age-related macular degeneration in the United States. Arch Ophthalmol 2004;122:564–572.)
Mexican Americans
Mexican Americans (Hispanic whites) have been found to have a relatively low prevalence of late AMD but a similar prevalence of signs of early AMD compared to non-Hispanic whites (19, 51). This observation was confirmed by data from the Los Angeles Latino Eye Study (LALES) (25) and the Proyecto Vision Evaluation and Research (VER) (32), both with large population-based samples of Hispanic whites, and the MESA Study (33), which used the same study methods, grading protocol and graders to assess AMD lesions in participants of four racial/ethnic groups (blacks, Hispanic, Chinese and whites).
Asians
Relatively well-conducted population-based studies of AMD prevalence in Asian populations have emerged in recent years, including studies conducted in Japan (28) (Funagata Study, unpublished data), India (29, 31), and China (30).
The prevalence of early and late AMD in Japanese and Indian populations does not appear to be substantially different from that in whites of the Western world, according to the two studies that used retinal photographic grading to diagnose AMD and AMD lesions (28, 31). However, the prevalence of soft drusen and retinal pigmentary abnormalities varies across studies (28, 31) and differs from the corresponding prevalence reported in white populations of similar age (soft distinct drusen 10–16%, soft indistinct drusen 5–8%, and pigmentary abnormalities 7–13%)(16, 18). While soft indistinct drusen were relatively infrequent in both Japanese (0.5%) (28) and Indians (2.2%) (31), the predominant early AMD lesion in the Japanese population was soft distinct drusen (8.4%) and not retinal pigmentary abnormalities (3.2%) (28), whereas in the Indian population, both soft distinct drusen (34.0%) and retinal pigmentary abnormalities (10.8%) were frequent (31). In a Chinese population aged 40+ years, the Beijing Eye Study team reported a very low prevalence of both early (1.4%) and late AMD (0.2%) (30).
Comparability of study findings from Asian populations to those of Western countries is still limited, due to different methods used across studies. Although the Wisconsin Age-Related Maculopathy Grading System has been used in these recent studies in Asia, the AMD grading used has not been validated either internally or externally (28, 30, 31). Standardized methodology in retinal photography and AMD grading, together with the use of uniform AMD definitions, are critical for new studies in Asia to confirm whether the differences in AMD frequency between Asian and Western populations are real.
There are other possible reasons that could explain the observed differences in AMD prevalence across studies and racial groups. It is worth noting that two Japanese studies both reported high prevalence rates of neovascular AMD in Japanese men, similar to those observed in whites but sharply contrasting with the much lower prevalence in Japanese women (28) (Funagata Study, unpublished data). Possible explanations for this gender difference may include a high prevalence of smoking among Japanese men and a higher frequency of polypoidal choroidal vasculopathy (PCV) among Japanese men compared to Japanese women (54). The complement factor H (CFH) polymorphism (the Y402H) has consistently been documented as a major AMD genetic marker in white patient samples. However, in Japanese and Chinese with late AMD, the frequency of the variant high risk genotypes (CC) or the risk allele (C) of CFH was much lower than that reported in whites with late AMD (55–57). This may partly explain the low prevalence of late AMD observed in the Japanese and the Chinese. Different AMD-related gene variants may be manifest in Asian with AMD. The lack of an association of CFH Y402H polymorphism with late AMD in two independent case studies of Japanese patients suggest that different gene polymorphisms may play a role in the pathogenesis of AMD in Asians compared to non-Asian cohorts (55, 56).
AGE-RELATED MACULAR DEGENERATION INCIDENCE IN WHITES
After the turn of the century a number of population-based studies, following the BDES (34, 37), have provided AMD incidence in older white populations (36,38–43,46,47).
The cumulative 5-year, person-specific incidence of early AMD has been reported to range from 7.9% to 8.7%, and the corresponding incidence of late AMD ranges from 0.9% to 1.1% in the three predominantly white populations across three continents, the BDES (34), RS (38) and the BMES (36), all of which used similar study protocols in AMD phenotype ascertainment. Similar to AMD prevalence, incidence of this condition is strongly age-related (34, 36, 38, 39), showing an exponential increase with age (see Fig. 30-2 of the report by the RS (38).
The long-term (10 or more years) cumulative incidence and progression of AMD has been reported by the BDES (37, 48), BMES (47), and the Copenhagen City Eye Study (42). Estimates from the two studies with reasonable follow-up rates (37, 47) indicate that the person-specific 10-year incidence of early AMD ranged from 10.8% to 12.1%, and the corresponding incidence of late AMD ranged from 2.1% to 2.8%, after age-standardization of the BMES to the BDES population (47). The 15-year cumulative incidence of late AMD was 3.1% and of early AMD was 14.3% in the BDES (48). In addition to age, incidence of late AMD was also strongly related to the severity of early AMD lesions at baseline (37, 47, 48).
A substantially higher incidence of neovascular AMD has been observed in the second eye of clinic patients presenting unilateral neovascular AMD, observed not only in whites (58–61) but also in Japanese (62). In the BMES population, 29% of second eyes developed end-stage AMD (neovascular AMD or geographic atrophy involving the fovea) in subjects with unilateral end-stage AMD (36).
PROGRESSION
Progression of AMD from soft (distinct or indistinct) drusen, reticular drusen, or retinal pigmentary abnormalities to geographic atrophy or neovascular AMD has been well documented in clinical case series (60, 63, 64). In the BDES and BMES, early ARM lesion characteristics have been studied in detail in terms of distribution, location, size, lesion type, and area involved in relation to the risk of subsequent development of late AMD (37, 65, 66). Large soft drusen (≥125 µm in diameter), soft drusen with indistinct margins (indistinct soft or reticular drusen), or pigmentary changes involving large macular areas plus close proximity to the fovea indicate a much higher risk of subsequent late AMD development (37, 65).
The Age-Related Eye Disease Study (AREDS) developed an ordinal AMD severity for risk prediction from pre-existing early AMD lesions defined from baseline retinal photographs (67, 68). The BMES 10-year AMD incidence data validated this AREDS AMD Simplified Severity Scale and provided further evidence supporting that incidence of late AMD strongly relates to the severity of early AMD lesions at baseline (47).
AGE-RELATED MACULAR DEGENERATION INCIDENCE IN OTHER ETHNICITIES
Blacks
The Barbados Eye Study reported 4-year (40) and 9-year incidence (46) of AMD in a black population aged 40–84 years at baseline. At the 4-year visit (40), incident neovascular AMD was observed in one of the 2362 persons at risk (0.04%) and incident geographic atrophy in none of the 2419 at risk (0%). The incidence of early AMD lesions, including intermediate-sized drusen, was also low (5.2%, 60/1160). However, at the 9-year visit, the long-term incidence of early AMD was 12.6% and of late AMD 0.7% (46). This 9-year incidence of early AMD is similar to that reported from the BDES and BMES (37, 47), but the 9-year incidence of late AMD is lower than that observed in whites (37, 47). In the AREDS participants who had early or intermediate AMD at baseline, the risk of progression to neovascular AMD over a median follow-up period of 6.3 years was nearly 7-fold in whites than in blacks (odds ratio 6.8, 95% confidence interval 1.2-36.9) (69).
Other Ethnicities
To date, there are no Hispanic white population-based data available on AMD incidence, and only one report from a Japanese population on the 5-year incidence of AMD (44). Early AMD incidence was 8.5% and late AMD incidence was 0.8% in Japanese aged 50+ years at baseline, with 1.9% in men but only 0.2% in women. The nearly 10-fold difference in incidence rates between Japanese men and women is consistent with findings of AMD prevalence among Japanese, possibly due to high frequency of smoking and high incident PCV cases in Japanese men (54).
EMERGING AMD RISK AND PROTECTIVE FACTORS
Smoking
Smoking is a major modifiable risk factor for AMD, consistently found not only in cross-sectional population-based studies (70–73) (Fig. 30-3A), but also in longitudinal studies (69, 74–80) (Fig. 30-3B). Pooled data estimated that risk for 5-year incidence of late AMD was more than double (odds ratio [OR] 2.35, 95% confidence interval [CI] 1.30–4.27) in current smokers compared to persons who never smoked (77) (Fig. 30-3B). Overall, the magnitude of risk for late AMD in current versus noncurrent smokers, or in past versus nonsmokers, ranges between 2- and 5-fold (80). In the BMES population (76), current smokers developed late AMD at a mean age of 67 years, while past smokers developed late AMD at a mean age of 73 years and nonsmokers at a mean age of 77 years. This 10-year average difference in the mean age of developing late AMD in smokers versus nonsmokers implies a substantial increase in the burden on affected individuals, their families, and aged disability care. Evidence supporting a causal role for smoking in AMD includes its dose-response relationship with pack-years of smoking (81, 82), reduced risk after smoking cessation (the earlier smoking cessation occurs, the lower the risk of developing AMD later in life (71, 81–84), and evidence from animal models (85). Passive smoking exposure has also been documented to be associated with AMD in a case control study (81), but not in a population-based study (86). Smoking as a major AMD risk factor has also been documented in Mexican American (87), Indian (88), and Japanese (44) populations.
Figure 30-3. A: Smoking and prevalence of late age-related macular degeneration. B: Smoking and incidence of late age-related macular degeneration.
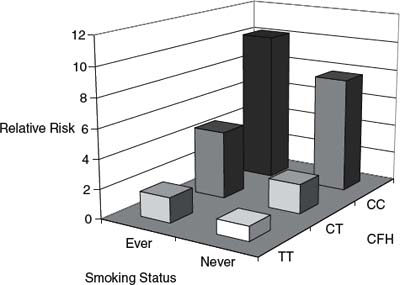
Figure 30-4. Joint effect of CFH-Y402H gene and smoking on risk of
age-related macular degeneration (93). CFH, complement factor H; CC; CT; TT.
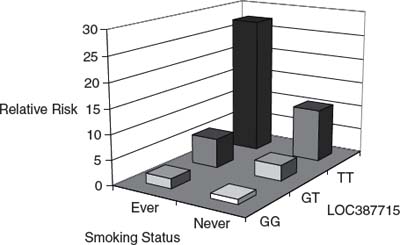
Figure 30-5. Joint effect of the Loc387715-A69S gene and smoking on risk of age-related macular degeneration (95). GG; GT; TT.
Evidence of synergistic effects of history of smoking with other factors contributing to high AMD risk has been emerging recently (82, 89–94). Carriers of the APOE 2 allele had a much higher risk of neovascular AMD if they smoked, compared to APOE 4 or APOE 3 carriers who also smoked (89). For the two confirmed AMD-related gene loci (CFH and LOC387715), smoking exerts a much greater effect on AMD risk in persons homozygous for the risk alleles of either of these two gene polymorphisms (Y402H in CFH and rs10490924 in LOC387715), compared to subjects homozygous for the nonrisk alleles (90–95) (Figs. 30-4 and Figs. 30-5). The odds ratio (OR) for AMD among individuals homozygous for the risk alleles who also smoked was two- or three-fold compared to subjects with either factor alone (nonsmoking, or absence of the risk alleles) (91, 92, 94, 96). In the BMES 10-year follow-up data, biological synergism of smoking with the lowest level of serum high-density lipoprotein (HDL) cholesterol, the highest total to HDL cholesterol ratio, or history of low fish consumption with AMD risk was suggested (82).
Based on currently available evidence, cigarette smoking is considered an important trigger or promoter in the course of the development of late AMD (80, 85). Emerging evidence indicates that combined effects of smoking with other AMD-related factors most likely contribute to the high risk of AMD among smokers (82, 94, 96). No statistically significant interaction on multiplicative scales has been established (96–98), but biological interaction on an additive scale (82, 92, 94, 96) is not uncommon (99).
ANTIOXIDANT NUTRIENTS
The hypothesis that oxidative damage may be involved in the pathogenesis of AMD (100) is supported by a number of factors: (a) the high concentration of polyunsaturated fatty acids present in the outer segments of photoreceptors of the retina; (b) high photo-oxidative stress and relatively high oxygen tension in this region, and; (c) the well-known susceptibility of polyunsaturated fatty acids to undergo oxidation in the presence of oxygen or oxygen-derived radical species (100). However, evidence of a protective effect of antioxidant nutrients against AMD has been inconsistent (101–109), as has the association between AMD and serum carotenoids (110–113).
Currently, evidence as to the effectiveness of intervention with antioxidant vitamin and mineral supplementation on slowing AMD progression is dominated by findings from one large randomized clinical trial, the AREDS (114, 115). In this study, a modest beneficial effect (25% reduction) from antioxidant and zinc supplementation on progression to late AMD was observed in persons with moderate to relatively advanced early AMD (114). While the majority of intervention trials conducted so far were underpowered to detect small differences (115), there is limited evidence at present suggesting that people with less advanced early AMD lesions should take supplements (115, 116), and the AREDS findings should only be applied to appropriate at-risk patients with caution (117). The UK Drug and Therapeutics Bulletin (118) published a very thorough evaluation of the use of nutritional supplements for AMD: subgroup analysis of AREDS data suggested that in patients with unilateral advanced AMD, the AREDS formula (a specific combination of high doses of zinc and antioxidant vitamins) may assist in preventing advanced disease and deterioration of visual acuity in the fellow eye, though there is no convincing evidence to support the use of nutritional supplements in other groups (118). The Food and Drug Administration (FDA) of the USA also concluded that no credible evidence exists for a health claim about the intake of lutein or zeaxanthin (or both) and the risk of AMD (119). The AREDS-2 is currently investigating this relationship.
DIETARY FATTY ACIDS, FISH CONSUMPTION, AND LIPIDS
The underlying hypothesis for associations between serum cholesterol and dietary fat intake and AMD arose from the speculation that AMD and cardiovascular disease may share common risk factors (120, 121) or similar pathogenesis (such as atherosclerosis and arterioscleroses) (121, 122). Another consistently documented factor associated with low AMD risk is regular fish consumption (72, 121–124) or dietary omega 3 fatty acid intake (125) (Fig. 30-6A, 30-6B). In the BMES cohort, joint exposure to low frequency of a history of fish consumption and current smoking was found to be associated with a much higher long-term risk of late AMD than the effect of either exposure alone (82). In comparison with nonsmoking individuals who consumed fish at least once per month, the relative risk of late AMD from current smoking increased from 2.7 (95% confidence interval, [CI], 0.9-7.7) in persons who regularly consumed fish at least once per month to 7.3 (95% CI 2.4-22.4) in those who consumed fish less than once a month, with an estimated synergy index of 4.2 (82) for biological interaction (99). In addition, BMES 10-year AMD incidence data showed that the protective effect from weekly fish consumption is only evident among subjects homozygous for the CHF Y402H C allele, with a statistically significant interaction (unpublished).
In three separate studies of largely different study samples, the Eye Disease Case-Control Study (125), the Age-related Macular Degeneration Study (121) and the US Twin Study of Age-related Macular Degeneration (72), Seddon et al. reported a possible joint effect of linoleic acid (a major component of omega-6 fatty acid) and omega-3 fatty acids or fish consumption on the risk of AMD. A trend of reduced AMD risk associated with increasing intake of omega-3 fatty acids (72, 125), or a reduced risk of AMD progression associated with fish consumption at least twice a week (121), was only evident in persons who consumed a diet low in linoleic acid. Similarly, in the BMES population, weekly consumption of fish was protective against early AMD incidence over 10 years only in subjects with low intake (below median) of linoleic acid (unpublished data).
No consistent evidence has been found for associations of AMD with other dietary fats (23, 121–129) or serum lipids (120, 129, 130–133). Use of cholesterol-lowering medications (statins) has also shown inconsistent findings of a protective effect on AMD prevalence (134–136) and incidence (137–141). Conflicting findings on these associations between intake of other mono- and poly-unsaturated fats, or serum lipids, and AMD suggest that these associations, if they exist, are unlikely to be major AMD risk factors.
Interpretation of findings regarding dietary data should be made with caution because these findings may be due, in part, to uncontrolled confounding. It is possible that participants with a previous diagnosis of early AMD subsequently changed to a healthier diet, or that persons with a better diet were more likely to have a better overall lifestyle and receive better medical care, accounting for the lower frequency of AMD. Such biases have been used to explain why data from longitudinal observational studies showed a benefit of hormone replacement therapy while a large randomized control trial, the Women’s Health Initiative, did not (142).
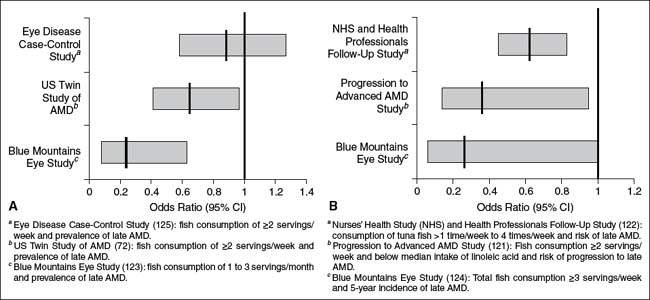
Figure 30-6. A: Regular fish intake and prevalence of late age-related macular degeneration. B: Regular fish consumption and incidence of late age-related macular degeneration.
INFLAMMATORY MARKERS
Inflammation may play a role in the pathogenesis of AMD. Supporting this hypothesis is the fact that leucocytes have been observed in choroidal neovascularization (CNV) tissues from post-mortem eyes with neovascular AMD (14, 143). In laser-induced CNV mice models, macrophages have been shown to have a role in the extent of CNV (144). This hypothesis has received further support from findings on some AMD-related genetic markers located on complement-related genes: CFH (complement regulatory gene) (11), C2/BF (complement pathway-associated genes) (13, 14, 145, 146) and C3 (the most abundant complement component) (147). CFH is known to modulate the complement cascade by inactivating components of the cascade and by binding initiation factors such as C-reactive protein (CRP) (14, 146, 148, 149). Age has been shown to be associated with increasing, and smoking associated with reducing, plasma levels of CFH (150). However, the CFH Y402H polymorphism was not found to be associated with CRP level (151, 152), nor did the genetic variation in CRP appear to be associated with risk of AMD (153).
A recent finding that the CFH Y402H polymorphism affects binding affinity to CRP has led to the hypothesis that reduced binding of CFH Y402H to CRP leads to impaired targeting of CFH to cellular debris, accumulation of which increases inflammation at the retinal pigment epithelium–choroid interface in subjects with AMD (154). This hypothesis is in keeping with one proposed by Anderson et al. (13) and Hageman et al. (155), namely, that local, immune-mediated, inflammation plays a role in drusen biogenesis (9, 13, 155), possibly analogous to processes observed in other age-related conditions such as Alzheimer’s disease and atherosclerosis (14, 156).
Some inflammatory markers, such as high leukocyte count, have been documented to be associated with long-term AMD incidence in two well-conducted population-based studies (157, 158). Other large studies have provided inconsistent evidence on the association between CRP and AMD incidence (159–163). A joint effect of AMD genetic susceptibility, indicated by the CFH Y402H CC genotype, with high CRP level or leukocyte count on AMD progression has been suggested in a population-based sample (92). Associations between AMD and factors related to hemostasis or endothelial dysfunction have also been reported inconsistently (164, 165).
It is has been speculated that certain microbial infections could be environmental triggers for AMD pathogenesis. Chlamydia pneumoniae infection has been thought to be a trigger, but its association with AMD has not been consistently documented (166–170). Use of systemic anti-inflammatory medications has not been found to have an effect on AMD prevalence or incidence (137, 171–173).
Despite the plausible hypothesis that AMD pathogenesis involves inflammatory processes, the associations of systemic inflammatory markers with AMD have been inconsistent. This could be explained by possible discordance between local and systemic inflammation, and that AMD pathogenesis involves other joint factors in addition to local inflammation or low-level systemic inflammation (92).
SUNLIGHT EXPOSURE
Although biologically plausible, the hypothesis of an association between sunlight or short wavelength blue light (174) exposure and AMD has proven difficult to investigate, due to lack of precise, quantitative measures on life-time exposure and confounding by sun-avoidance behavior in subjects with very fair skin susceptible to sun-related skin damage (175). Surrogate factors (questionnaires, sun-related skin damage or presence of pterygium) have been used in epidemiological studies (175–181), with inconsistent associations found to date (180).
In the BDES population some consistency is revealed across baseline cross-sectional data (178), 5-year (182) and 10-year (183) longitudinal data. Time spent outdoors in summer, particularly earlier in life (teens to thirties), was associated with an increased risk of early AMD later in life (182, 183), while the use of hats or sunglasses appeared to provide some protection against development of early AMD lesions later in life (182, 183).
In the BMES (181) persons presenting with pterygium or reporting a past history of pterygium surgery at baseline had an increased risk of 5-year incident late (adjusted OR 3.3, 95% CI 1.1-10.3) and early AMD (adjusted OR 1.8, 95% CI 1.1-2.9). A recent report from a UK case-control study found no association between late AMD and sunlight exposure-related factors, except for the suggestion of an association between skin type prone to sunburn and geographic atrophy (184), a finding consistent with observations from a previous population-based case-control study (175). Although accumulated data suggest the possibility of a sunlight exposure–AMD link, inconsistent evidence does not support the association to be strong (5).
POST CATARACT SURGERY
Light exposure to eyes may increase after cataract surgery (including eyes with intraocular lens implantation). Whether the risk of late AMD is increased in eyes following cataract surgery is a longstanding but unresolved clinical question. Conflicting findings exist between clinical and population-based studies (174). A higher risk of developing late-stage AMD in eyes following cataract surgery has previously been documented in both clinic (185, 186) and population-based cross-sectional (50, 88), case-control (187) and longitudinal studies (188–190) (Fig. 30-7A, 30-7B). A report from postmortem eyes also suggested that neovascular AMD was more frequent in pseudophakic than phakic eyes (191). In contrast, the AREDS (192) and some clinical studies could not confirm a definite link (193, 194).
Potential confounding factors could be operative in this observed association. Cataract surgery could be recommended for some patients with early AMD signs, to enable a better view of the fundus to facilitate diagnosis and therapy. Cataract in the fellow eye of persons with unilateral late AMD may cause substantial disability and a greater need for surgical intervention. As AMD tends to be bilateral, the risk of AMD developing in the second eye of such cases would be much higher than the risk of AMD occurring in the first eye (58–61), irrespective of cataract surgery. Analogous to recently documented synergisms between smoking and genetic variants (90–95), cataract surgery or the nonphakic ocular status alone may not accelerate AMD progression but could act as a trigger to modify the risk of late AMD development and accelerate AMD progression if in combination with other genetic and systemic AMD risk factors. Longitudinal cohort studies on cataract surgical patients are needed to answer this important clinical question. It is important for patients who already have AMD risk signs or AMD genetic susceptibility to be informed about findings of cataract surgery and higher risk in some studies and to discuss this with their doctors before undergoing cataract surgery.
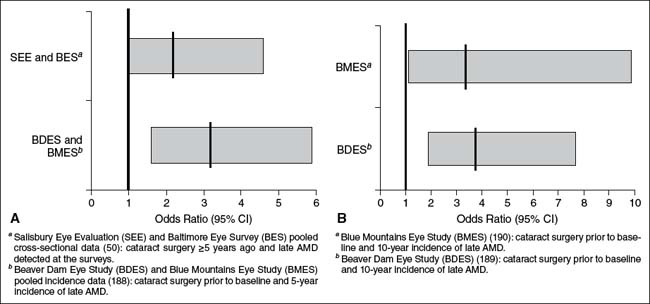
Figure 30-1. A: Prior cataract surgery and 5-year risk of late age-related macular degeneration B: Cataract surgery prior to baseline and 10-year incidence of late age-related macular degeneration in the Blue Mountains and Beaver Dam Eye Studies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


