6 Age-Related Hearing Loss
 Introduction
Introduction
With advances in health care, life expectancy is increasing. Aging is associated with multiple related medical problems which have been referred to as geriatric syndromes.1 These syndromes typically interact with one another, have more than one cause, and broadly impact functional status of the geriatric patient. Sensory problems, such as impairments of vision, balance, and hearing, are well recognized geriatric syndromes, with hearing loss being the most common sensory problem among older adults.
In 2012, the U.S. Census Bureau projected that the U.S. population aged 65 and older will outnumber the population younger than 18 by 2038.2 It is projected that, in 2015, 15% (47 million) and 2% (6 million) of the population will be 65 and 85 years old and older, respectively; but by 2060, the percent distribution will increase to 22% (92 million) and 4% (18 million), respectively. Studies based on the National Health and Nutrition Examination Survey (NHANES) show that an increasing proportion of the population suffers from hearing loss, reaching more than 80% of those older than 85 years.3 Age-related hearing loss (ARHL) is, by far, the leading cause of hearing loss in developed countries.4
By definition, ARHL is a progressive disorder. Another term commonly used for this disorder is presbycusis. New York otologist St. John Roosa is credited with being the first to describe it as “a physiological… rather than a pathological, change in the ear… analogous to presbyopia, and… termed presbykousis.”5 The term is derived from the Greek presbus (elder) and acouste (to hear). Today, our understanding of this disorder has expanded to include pathological processes in the cochlea and the brain that were not suspected in the late 19th century. Whereas the peripheral pathology is universally accepted, our understanding of changes in the central auditory pathways and the global implications of these changes for management of patients with ARHL is continuing to evolve.
 Presentation
Presentation
Although onset is variable and dependent on several contributing factors, often the earliest symptoms of ARHL appear late in middle age. By this time, cochlear changes have progressed to affect hearing sensitivity in the frequency range that makes up our daily communication sounds. Patients commonly misunderstand similar-sounding words and tend to use context to compensate for this early deficit. In general, consonants are higher pitched than vowels and are spoken more softly than vowels. Age-related high-frequency hearing loss will result in difficulty hearing consonants and makes it easier for background noise to mask. Because consonants convey most of the information in a word, inability to hear them effectively will result in deterioration of speech intelligibility. Furthermore, consonants serve to separate syllables and words from one another. Therefore, with disruption of these breakpoints, words tend to run together and sound “mumbled.” Because voices of children and women tend to have a higher pitch, the initial complaints might be about the low volume and quality of a grandchild’s voice.
Over the years, as disruption of cochlear function extends toward the lower frequency regions, functional consequences become more substantial. With age-related cognitive changes ranging from slowed processing to frank impairment, the ability to use context efficiently to compensate for hearing deficits diminishes. Hearing in noisy or reverberant environments and accented or fast-paced speech become more challenging. A common complaint arising from these disruptions in speech intelligibility is “I can hear the words, but I can’t understand them.” Patients resort to varied strategies to cope. These strategies are influenced by several factors, including personality traits. When individuals have an external locus of control, complaints such as “my grandchildren mumble” are common. On the other hand, those with an internal locus of control display maladaptive strategies such as withdrawal from family conversations.
In general, evaluation and management of hearing loss require insights into the contributing pathophysiological conditions. However, management of age-related disorders is far more complex and challenging because these disorders, including hearing loss, rarely present in isolation. It is estimated that 50 to 75% of adults over age 65 have multiple chronic health conditions. Improving care of these individuals is a priority for the Department of Health and Human Services, and they are a focus of Healthy People 2020.6 Toward this goal, effort is being directed toward integrated care for older individuals with multimorbidity.7 This effort is compelling because persons with combined disabilities are at increased risk of cardiovascular and all-cause mortality.8
The diagnosis of ARHL is based on patient history, physical examination, and a battery of audiological and other testing. Pathophysiology of ARHL is that of a progressive and insidious process, with affected individuals frequently less aware of their communication difficulties than the people around them. In longitudinal studies, deterioration of hearing is reported to be continuous and gradual for the majority of people, ranging from 1 to 6 dB/decade,9–11 although this rate may increase up to 9 dB/decade in older individuals.9 Because of the insidious nature of this disorder, patients often present reluctantly to the clinician, at the insistence of family members.
Besides speech sounds, other important high-frequency warning sounds (alarms, ringing tones, turn signals, etc.) also become more difficult to hear. The common scenario in which a grandparent wearing a digital watch is unaware of the beeping high-pitched alarm is one typical example. Reduced ability to hear alarms raises concern about safety. For example, older individuals with hearing loss have been shown to be at increased risk of motor vehicle accidents while driving.12 There are also social ramifications to this attribute of age-related hearing loss. Difficulties hearing on the telephone, particularly cell phones in which quality of sound may fluctuate with the strength of the network signal, serve as a barrier to their effective use as an alternative to face-to-face communication. The use of high-pitched ring tones by adolescents to communicate via cell phones takes advantage of the inability of the older listeners to detect these sounds in structured settings such as classrooms. Older listeners are also typically unaware of unpleasant high-pitched noise emitted by some electronic devices and chargers, as well as antiloitering devices.
Besides difficulty in hearing communication sounds and alarms, other auditory functions are also impaired. For example, age and hearing loss also impact localization performance. A large body of evidence shows that the accuracy to localize sound sources declines with age, resulting in front–back confusions, especially for spectrally restricted sounds.13–15 Localization accuracy and acuity of acoustic stimuli decline with age and result in a blurred representation of sound sources.16 These deficits are attributed to age-related increase in the neural temporal jitter in the central auditory system that affects the accurate processing of timing information, which is crucial to acuity in representation of sound source position.
As hearing loss severity increases, overall functional status diminishes among older individuals.17,18 It has long been speculated that inability to communicate effectively, and potential decreased overall functional status, will lead to social isolation. For example, hearing impairment has been shown to be associated with poorer scores in social functioning assessments in older Australians.19 Similarly, poorer self-reported hearing scores predicted deterioration in social support among a large cohort of Dutch seniors.20 A recent study by Mick et al, in which cross-sectional data for adults 60 to 84 years old were extracted from the 1999 to 2006 cycles of the U.S. NHANES, revealed that greater hearing loss is associated with increased odds of being socially isolated in women aged 60 to 69 years.21 This association was not affected by use of hearing aids. Based on their results, Mick et al conjectured that females may rely more heavily than males on verbal communication; therefore, hearing loss might impair their ability to receive emotional support to a greater degree than males. Social isolation has significant implications for the well-being of geriatric patients: lonely or isolated older adults are at greater risk for all-cause mortality and development and progression of cardiovascular disease, and lonely older individuals are more than twice as likely to develop Alzheimer disease (AD).22 As noted earlier, hearing loss in older individuals was shown to be associated with increased all-cause mortality in the Australian Blue Mountains Hearing Study.8 Increased all-cause mortality is believed to be mediated by three variables: disability in walking, cognitive impairment, and self-rated health. Thus, besides the insidious nature of the disorder, the isolation associated with hearing loss may be another factor that leads to delayed presentation and diagnosis, primarily because there is little pressure to seek care for communication difficulties.
Inherent difficulties in communication that result in compounding psychosocial effects such as isolation may precipitate psychiatric disorders such as depression. Whether hearing loss can contribute to depression has been a subject of debate. “Limited” and “‘pervasive” degrees of depression were reported in 69% of community-dwelling elders with hearing impairment compared with 31% of non-hearing-impaired individuals.23 Davis and colleagues reported that hearing-impaired elders were 1.79 times more likely than non-hearing-impaired subjects to be depressed.9 Consistent with this view, ARHL tends be associated with late-onset depression but not with early-onset depression.24 In a meta-analysis of published literature, the relationship between chronic diseases and risk for depression in old age was examined by calculating odds risk (OR) and relative risk (RR) for prevalence and incidence rates of depression, respectively.25 Loss of hearing was among a few chronic diseases, including stroke, loss of vision, cardiac disease, or chronic lung disease, that had both a significant OR and a significant RR for increased depression in old age.
On the other hand, the Nord-Trøndelag Hearing Loss Study with data from over 50,000 Norwegians aged 20 to 101 found substantial effects of hearing loss on symptoms of anxiety, depression, self-esteem, and subjective well-being in young and middle-aged persons, but not the older persons.26 Similarly, the Longitudinal Aging Study Amsterdam, in a 4-year follow-up study of older hearing-impaired subjects, found that although hearing loss was associated with loneliness, it was not associated with depression.27
In a cross-sectional study of Americans aged 50 and above, dual sensory loss, vision loss only, and hearing loss only were significantly associated with depression after age, gender, poverty, education, functional impairment, bed days, self-rated health, social support, and social activities were controlled for.28 In contrast, in an English longitudinal study, controlling for health-related variables, including the number of medical conditions and functional disability renders insignificant the association between sensory loss in both vision and hearing with both the onset and the persistence of depression in older persons.29
If depression is indeed a consequence of hearing loss and isolation, that may further reduce the likelihood of patients with ARHL seeking medical attention. Given its psychosocial implications, it has been recommended that clinicians maintain a low threshold for suspecting hearing loss in older patients, particularly when they present with comorbidities like anxiety, depression, or apparent cognitive decline.30
Another symptom that affects the well-being of patients with sensorineural hearing loss is tinnitus. About 85% of patients visiting an otologist have tinnitus.31 The incidence of tinnitus increases with age: tinnitus affects 15% of the general population and 33% of geriatric persons.32 In a longitudinal study of Swedish men and women in their 70s, 15% had continuous tinnitus, and 42% had occasional tinnitus, without any difference in the prevalence of tinnitus between men and women.33 It is not surprising that tinnitus commonly accompanies ARHL.34 This latter entity has been referred to as presbytinnitus.35 Presence of tinnitus by itself is not an independent risk factor for depression,36 but older individuals who perceive their tinnitus to be a problem or who have problems with tinnitus when going to bed often display depression symptoms.37 In patients who also have ARHL, tinnitus can be a source of emotional and sleep disorders, difficulties in concentration, and social problems.34 Tinnitus has been divided broadly into two groups based on age of onset: early- and late-onset.38 The two differ not only with regard to prevalence but also with regard to tinnitus-related distress, with late-onset sufferers being more distressed. Resting state electroencephalography source-localized activity and connectivity comparing the two groups revealed increased activity and functional connectivity in the late-onset group, supporting intrinsic differences in tinnitus-related neural activity, which may have implications for management.39
In geriatric patients, the presence of tinnitus is associated with reduced systolic and diastolic blood pressure, reduced left ventricular ejection fraction, and increased brain natriuretic peptide (BNP) plasma levels.40 These finding suggest that tinnitus is associated with worse control of congestive heart failure in geriatric patients and may have important clinical implications for the early identification of patients who need more aggressive management of heart failure. These findings also lend support to the notion that hemodynamic imbalance can contribute to cochlear impairment in general and tinnitus in particular.
 Risk Factors
Risk Factors
Several factors have been recognized as contributing to the development of ARHL. These might be broadly classified into two categories: intrinsic and extrinsic. Intrinsic factors are host factors and are primarily genetic (including sex and race), but also include health comorbidities (hypertension, diabetes, and stroke). Extrinsic factors in the environment include occupational and leisure noise exposure, smoking, ototoxic medications, socioeconomic status, and other factors. A more practical classification of risk factors is based on whether they can be modified to reduce their impact on ARHL. From this perspective, at the present time, genetic factors are not modifiable. In contrast, disease processes and environmental factors are believed to be modifiable such that their control could delay or minimize hearing loss.
Genetic Factors
Individuals with ARHL often report a family history of hearing loss among parents, siblings, and close relatives. Therefore, it has been presumed that ARHL has a genetic component that influences the age of onset and severity of the loss. Challenges in separation of environmental from genetic factors have made it difficult to assess the contribution of genetics to ARHL. Several lines of evidence, including animal research, large population-based cohort studies, and gene studies using linkage and association analysis have led to estimations of heritability and identified several genetic foci that are thought to be contributory.
Similarities between the auditory systems of mice and humans have allowed researchers to use mice as a model for better understanding of ARHL. Specifically, mutation of the Ahl1 gene (age-related hearing loss gene 1), mapped to chromosome 10, is associated with elevated hearing thresholds at high frequencies in middle- and older-aged inbred mice.41 Cadherin 23 is the gene associated with this locus and has been localized to stereocilia.42 Based on this finding, it is hypothesized that cadherin 23 plays a critical role in signal transduction in the inner ear. More recently, four other genes on the mouse chromosome 10 have been implicated.43–46 Using a genetically heterogeneous population of mice, several polymorphisms affecting ARHL and its modulation by noise have been defined, which included chromosome 10.47 The homologous genes regulating ARHL have yet to be identified in humans.
Large-population-based cohorts have proven useful in detecting the role of inheritance in ARHL. In the Framingham cohort, heritability of ARHL phenotypes was estimated to be 0.35 to 0.55.48 In that study, hearing levels in genetically unrelated and genetically related individuals with sensory and strial presbycusis were compared. The sensory presbycusis phenotype (described later in the chapter) showed a familial aggregation of hearing threshold levels, which was greatest for mother–daughter pairs, sister pairs, and brother pairs. The correlations for the father–child pairs were not significant, which was suggestive of extrinsic factors playing a larger role in the father’s hearing loss patterns. The strial presbycusis phenotype (described later in the chapter) demonstrated a strong familial association in the sister–sister and mother–daughter pairs. Overall, the heritability estimates suggest that 35 to 55% of the variance of the sensory presbycusis phenotype and 25 to 42% of the strial presbycusis phenotype are attributable to genes. The results of this study demonstrated that in a large group of biologically related people, hearing sensitivity is more similar than in a group in the same general environment but who are unrelated. A subsequent study in this population examined the genetic linkage between measures from audiometric examinations and markers from a genomewide scan.49 The scan identified multiple chromosomal locations with evidence of linkage to presbycusis, with some of these locations corresponding with genes implicated in congenital deafness. The analysis revealed three distinct regions on chromosome 11 (2, 79, 143 cM), as well as a region on chromosomes 10 (171 cM), 14 (126 cM), and 18 (116 cM) that showed evidence of linkage.
Heritability of audiometric shape parameters and the familial aggregation of different types of presbycusis were investigated in siblings.50 The authors found higher heredity for severe types of presbycusis compared with moderate or mild types, and low heredity for “concavity.”
The association between the magnitude of hearing loss and self-reported family history was explored in a study conducted in a population 50 years or older in Sydney, Australia.51 The prevalence of hearing loss was 33%, with 68.2% classified as mild and 31.8% classified as moderate to severe. Of the 2,669 subjects, 46.7% gave a family history of hearing loss. Participants who reported a family history of hearing loss were younger than those who reported no family history. Participants with increased severity of hearing loss were also more likely to report a family history of hearing loss among parents or siblings. After adjusting for known risk factors (age, sex, history of noise exposure, diabetes, smoking) a positive family history was shown to be strongly associated with hearing loss. This association was true regardless of whether the loss was reported in the mother, father, or siblings. The findings from this study support a strong association between family history and presbycusis, with the association seemingly stronger with more severe hearing loss. Strong associations were found between maternal family history and moderate to severe hearing loss in women and paternal family history and moderate to severe hearing loss in men.
A study of monozygotic and dizygotic twins explored the relative importance of genetic and environmental factors in self-reported reduced hearing among an older Danish population.52 That study showed that probandwise concordance rates (probability of disease for one twin given that the partner is affected) and odds ratios (the increased risk of reduced hearing for one twin given the presence vs. the absence of reduced hearing in the partner twin) were higher in the monozygotic twin pairs than in the dizygotic twin pairs, indicating a heritable effect. The heritability was estimated to be 40%.
Members of the National Academy of Sciences–National Research Council (NAS-NRC) twin panel underwent a linkage analysis for presbycusis.53 This study highlighted a region of chromosome 3 mapped to the DFNA18 locus and showed a heritability of 61% for presbycusis. Individuals carrying two mutations of gap junction gene, GJB2, are at increased risk of developing early presbycusis.54
In another effort to identify specific ARHL genes, a genetic association study was performed with 2,418 samples from across nine European countries.55 One gene, the grainyhead-like 2 gene (GRHL2), was found to be associated with ARHL in this population.55 In contrast, no positive association was found between GRHL2 polymorphisms and ARHL in Han Chinese.56 Therefore, population differences might be a key factor in genetic expression.
Mitochondrial DNA mutations also have been implicated in the development of presbycusis. Mitochondrial function is essential for tissues with high metabolic activity such as the cochlea. Mutations in the mitochondrial genome accumulate with age; and once they reach a threshold level, oxidative phosphorylation and tissue function are compromised. Bai and colleagues reported that the Common Deletion (CD, a 4,977 base pair deletion most commonly associated with aging) was found in a higher frequency in temporal bones from individuals known to have been affected by presbycusis compared with those unaffected.57 Consistent with this finding, Markaryan and colleagues reported that with increasing age, the quantity of the CD increased and that the amount of the CD directly and significantly correlated with the severity of hearing loss at 8,000 Hz.58 Mitochondrial mutation and deletion have been shown to contribute to the development of ARHL in a rodent model of presbycusis.59 On the other hand, ARHL in humans was not associated with mitochondrial mutations in a large sample of 200 patients with ARHL.60
Oxidative stress is one possible mechanism for the aging process,61 and cochlear oxidative stress has been implicated in mouse models of ARHL.62,63 The dismutase 2 (SOD2) gene encodes a ubiquitous mitochondrial superoxide dismutase enzyme (manganese superoxide dismutase [MnSOD]) crucial for maintenance of reactive oxygen species homeostasis and has been implicated in the pathology of aging. SOD2 expression is reported to increase along a basal-to-apical gradient in cochlear spiral ganglion cells in a manner consistent with the known gradient of hair cell loss in ARHL.64 A genetic association between different polymorphisms in the SOD2 gene and noise-induced hearing loss has also been described.65 A role of common SOD2 promoter variation on SOD2 promoter regulation has been described, and SOD2 has been linked to ARHL risk in men, further implicating mitochondrial genes.66
Antioxidant enzymes include those involved in glutathione metabolism, such as glutathione S-transferase (GST) and N-acetyltransferase (NAT), which are involved in the metabolism and detoxification of cytotoxic and carcinogenic compounds as well as reactive oxygen species (ROS). Individuals carrying polymorphisms of GSTM1, GSTT1 null genotype,67 and a NAT mutant allele68 are at increased risk of developing presbycusis. In fact, individuals with the GSTT1 null genotypes are almost three times more likely to develop presbycusis.67 The association of audiometric patterns and polymorphisms of antioxidant enzymes have also been explored in ARHL.69 Mutant alleles for GSTT1 are more likely to have a high-frequency, steeply sloping audiogram, suggesting that the basal turn of the cochlea is susceptible to GSTT1-regulated oxidative stress.
On the threshold of the era of personalized medicine, identification of specific genetic factors may render gene therapy a possible treatment for presbycusis. For example, the introduction of the developmental gene Math1 has resulted in the recovery of hearing abilities of mature deaf mice.70 In the more proximate future, however, knowledge of genetic susceptibility may allow individuals with a family history of presbycusis to take preventive measures from a young age to help avoid or delay the development of hearing loss by addressing modifiable risk factors for ARHL. Steps that could particularly help these at-risk individuals include healthier diet, not smoking, minimization of noise exposure, and management of aggravating comorbidities such as diabetes and vascular disease.
Modifiable Risk Factors
The influence of genetics is likely to be modulated by a set of nongenetic factors. Cross-sectional studies have identified several associations between chronic health conditions and hearing loss, although longitudinal analyses have failed to support consistently the association of some of these risk factors with incidence of ARHL. Cardiovascular disease71–75 and diabetes76–80 are well recognized as risk factors. Hypertension is also linked to hearing loss in some studies,11,81 but not consistently.82 Older persons with moderate-to-severe hearing loss have a significantly higher likelihood of reporting previous stroke; but unlike sudden hearing loss, age-related hearing loss is not predictive of increased risk of stroke, at least over a 5-year follow-up.83 Chronic kidney disease76,84 and systemic inflammation may contribute to progression of ARHL,85 although the latter may affect ARHL more actively in its early phases.86 A common thread among these disorders is vascular disease/arteriosclerosis. Along this line, it has been suggested that hearing loss precedes clinical manifestations of ischemic heart disease and may be an important “early marker” of a vascular or generalized arteriosclerotic process.87
Although these conditions are risk factors for prevalence of hearing loss (cross-sectional studies), they are not always found to be predictive of incidence of hearing loss (longitudinal studies).11 Some studies may fail to implicate these risk factors because they are only weakly associated with hearing loss such that their effect is obscured by other factors.82
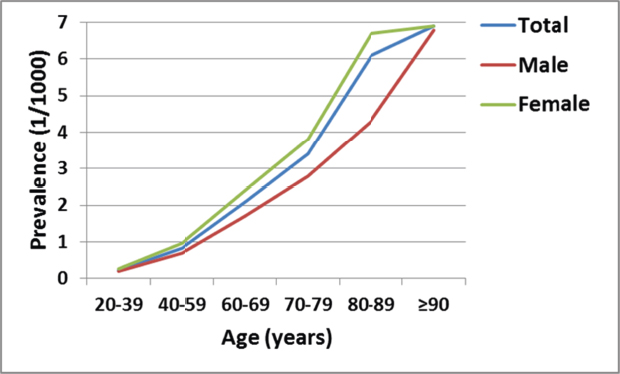
Besides systemic disorders, otologic disease can also impact hearing in the aged. In one study, chronic otitis media was found in 13.8% of the cases, otosclerosis in 3.8%, and Ménière disease in 1.3%.88 A more recent study found the prevalence of middle-ear diseases resulting in conductive or mixed hearing loss to be 6.1 to 10.3%, 1 to 3% for otosclerosis and 1.2% for Ménière disease.89 Hearing impairment in Ménière disease appeared to increase linearly with the duration of the disease for patients < 50 years of age; but in older subjects, the effect of the duration of the disease decreased.90 The difference that occurred at the onset of the disease remained until presbycusis in the better ear reached the hearing level of the worse ear. There is an increase in the prevalence of otosclerosis in those older than 60 years of age, reaching its peak in the age group above 80 years (Fig. 6.1).91 A significant deterioration in the hearing level has been reported in otosclerotic ears as a function of age,91 but the rate of age-related sensorineural hearing loss in stapedectomy-treated ears is similar to that expected from presbycusis.91–93 Demineralization of the cochlea has been associated with sensorineural hearing loss in bone diseases, including Paget disease and cochlear otosclerosis. The extent to which Paget disease and cochlear otosclerosis interact with ARHL to affect hearing has not been described. An association between femoral neck bone mass and ARHL in a population of rural women aged 60 to 85 years has been reported.94 This finding suggests that demineralization of the otic capsule in conjunction with age-related bone mass loss might be one biological factor contributing to hearing loss in the geriatric population. However, no consistent relationship was found between bone density and hearing sensitivity in a population-based sample.95
Besides disease-related risk factors, there is also a set of modifiable environmental factors that have been identified. Noise exposure and cigarette smoking73,81,96,97 are the best established risk factors. Smoking-related worsening of hearing loss with age is likely mediated by vascular disease. Those with a history of noise exposure typically display more accelerated ARHL,98–100 although vulnerability to deleterious effects of noise exposure is not uniform across the population,101 and not all studies are in agreement on the effect of noise on ARHL.10,102 There is experimental evidence that early noise exposure can lead to accelerated age-related hearing loss in a mouse model.103 Among older adults, a history of exposure to workplace noise raises the risk of cardiovascular disease and angina, and severe exposure was associated with incident stroke (OR 3.44).104 Long-time smokers with occupational noise exposure tend to have a higher risk of permanent sensorineural hearing loss (SNHL).105
Another recognized risk factor is history of exposure to ototoxic drugs. For example, chemotherapeutic agents such as cisplatin are used commonly in management of oncological disease, the incidence of which increases with age. Persons over 70 account for 45% of newly diagnosed malignancies.106 Not surprisingly, many cancer patients have ARHL before introduction of chemotherapeutic regimens.107 All markers of oxidant stress, lipid peroxidation, glutathionylation, and nitrosylation of proteins increase, whereas the measures of antioxidant defenses, mitochondrial apoptosis-inducing factor, and superoxide dismutase 2 (SOD2) decrease with age.108 Similarly, ototoxicity in general is believed to involve accumulation of ROS, leading to apoptosis.109,110 Therefore, at least theoretically, the dual demand on the antioxidant scavenger system might be expected to lead to poorer hearing outcomes.111 It is not known whether a synergistic interaction between ARHL and cisplatin ototoxicity is present. There is only one study that hints at possible outcomes. Older patients appear to show significantly greater incidence of audiometric changes after cisplatin treatment.112 However, this study did not have adequate controls to be conclusive. The experimental finding that intratympanic dexamethasone has otoprotectant properties against cisplatin-induced ototoxicity might imply that the antioxidant scavenger system might have sufficient reserve to prevent a negative interaction between ARHL and ototoxins.111
Because oxidative stress has been linked to ARHL, several studies have examined whether an antioxidant-rich diet can delay the progression of ARHL in animal models of presbycusis, with mixed results.113–115 Caloric restriction has been shown to suppress apoptosis in the cochlea and prevent presbycusis in a mouse model.116 Diet and nutrition certainly appear to influence human ARHL. Increased levels of dietary vitamin E and A (antioxidants) are associated with a reduced likelihood of prevalent hearing loss, but they do not affect risk of incident hearing loss in 5 year follow-up.117 There is an inverse association between higher dietary intake of long-chain omega-3 fatty acids and regular weekly fish consumption.118 Overall, healthy diets tend to be associated with better high-frequency thresholds in adults.119 High body mass index97 and central obesity, as measured by waist circumference, is an independent risk factor for age-related hearing loss in women older than 55.120 Moderate alcohol consumption is inversely correlated with hearing loss in the high, as well as in the low frequencies.97
Chronic sun exposure, as measured by facial wrinkles, is positively associated with age-related hearing loss.121 Sunlight, a source of ultraviolet radiation, may be a source of systemic oxidative stress, which may be an underlying mechanism for presbycusis. Chronic sun exposure is more likely to produce hearing loss in those with low levels of antioxidants but without occupational noise exposure.121 Chronic low-level lead exposure may be an important risk factor for ARHL.122 On the other hand, higher educational attainment appears to be negatively associated with hearing impairment.123
People born in more recent years are less likely to have hearing impairment at a given age than those born in earlier years.124 Over a typical generational span of 20 years, the prevalence of hearing impairment declined by 42% and 23% for men and women, respectively. This birth cohort effect likely is secondary to increased awareness of deleterious effects of noise and is consistent with the view that environmental and modifiable factors may be associated with the development of hearing impairment. Given concern about early exposure to noise resulting in accelerated age-related hearing loss,103 the decline in hearing impairment may be reversed with the popularity of personal listening devices among youth today. Indeed, the users of these devices have been demonstrated to exhibit elevated extended highfrequency (9–16 kHz) audiometric thresholds and reduced otoacoustic emission amplitudes, an early finding of noise-induced hearing loss.125
 Relationship of Audiogram Characteristics to Cochlear Pathology
Relationship of Audiogram Characteristics to Cochlear Pathology
Audiometric evaluation for ARHL relies principally on the pure-tone threshold audiogram. It should be acknowledged that a standard audiometric evaluation is not a purely sensory test. Patient decisions about having heard a signal are governed by a set of self-generated rules that lie along a continuum from stringent to lenient. A patient who adopts a strict approach will respond only when absolutely certain that a signal was heard. In contrast, when lenient rules are adopted the patient will respond whenever presence of a signal is suspected. The decision variables reflect the central processes within listeners that mediate all stimulus-response tasks. The notion of a cognitive component for threshold testing (i.e., “did I hear the tone or not”) is supported by Gates and colleagues, who reported that pure-tone thresholds were worse in those with poorer executive function scores when they compared normal subjects to those with mild memory impairment but without other signs of dementia and to those with an established diagnosis of AD.126
For the purpose of the present discussion, cognitive implications of threshold testing will be set aside to focus on peripheral processes of ARHL. As highlighted in the preceding discussion, there are numerous factors that can affect hearing in old age and reflect history of genes, noise exposure, vascular health, diet, medications, and other factors. Therefore, it is not surprising that patients with ARHL do not present with a characteristic audiometric pattern or onset in a fixed age range. Whereas the conventional audiogram evaluates hearing thresholds up to 8 kHz, testing higher frequencies (i.e., extended high frequency) allows detection of elevated hearing thresholds at a younger age.10,127,128 This suggests that ARHL is a progressive sensorineural degenerative process whose onset may actually precede “old age.”
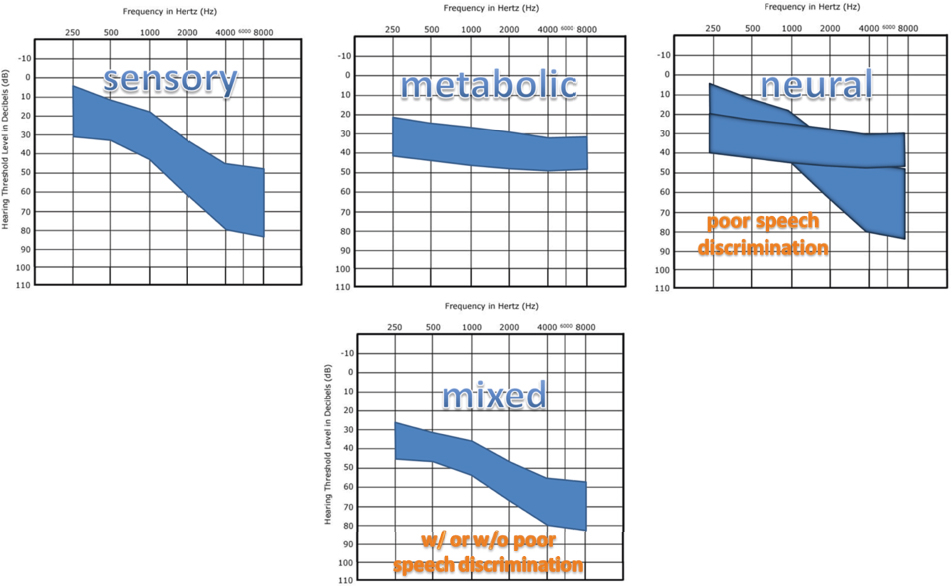
Given the diversity in presentation of ARHL, types of ARHL have been classified based on audiometric profile (Fig. 6.2). Perhaps the best-known scheme is that of Schuknecht, who correlated postmortem cochlear histopathology and pure-tone threshold audiogram findings to propose four main types of presbycusis: neural—associated with spiral ganglion loss; metabolic—associated with stria vascularis changes; sensory—associated primarily with hair cell loss; and conductive—not associated with a clear pathological correlate.129,130
Sensory presbycusis appears to be from disruption or loss of outer hair cells, in the basal turn of the cochlea. Histologically, as hair cells and supporting cells undergo apoptosis, flattening and atrophy of the organ of Corti are seen. Microscopic examination of cochlear tissue reveals accumulation of lipofuscin intracellularly, a marker of senescence. The audiogram associated with sensory presbycusis typically shows a sharply sloping, high-frequency loss extending beyond the speech frequency range, with a slow, symmetric and bilateral progression of hearing loss over the years.
Neural presbycusis is associated with a loss of spiral ganglion cells and axons within the spiral osseous lamina, beginning in the basal turn of the cochlea. The organ of Corti in this type of presbycusis may show little sign of age-related degeneration. These changes disrupt transmission of the electrochemical signal from the cochlea into the auditory pathway via cranial nerve (CN) VIII, as reflected in increased thresholds of compound action potentials and dyssynchronous neural activity, which may be related to synaptic abnormalities.131 Classically, audiograms of patients with neural presbycusis show a moderate downward slope into higher frequencies with gradual worsening over time. A severe loss in speech discrimination out of proportion to the threshold loss is often described, making amplification difficult due to poor comprehension.
Strial or metabolic presbycusis occurs with deterioration or atrophy of the stria vascularis. It is slowly progressive and often genetic within families. Functionally, the stria can be thought of as the “battery” of the cochlea that maintains endolymphatic potential. Audiograms classically associated with strial presbycusis show a flat loss with slow progression and good speech discrimination with no loudness recruitment. Although structurally intact, the function of the hair cells and consequently the spiral ganglion is disrupted by the inability to maintain endolymphatic potential. Significant improvement is possible with hearing aid amplification because speech discrimination is not usually affected. Strial loss usually occurs in small, focal lesions in the extreme ends of the apex and lower basal turns of the cochlea, but it can spread to involve larger segments or diffuse strial loss. Localized areas with only 20 to 30% loss may not result in much functional change, but > 50% loss leads to decreased endolymphatic potential and poor cochlear amplification with loss of gain (20 dB in the cochlear apex up to 60 dB in the base).
Vascular and noise-induced presbycusis are among other proposed categories of presbycusis that reflect threshold elevations correlated to hypertension, cardiac disease, and stroke, or threshold elevations related to the intensity, duration, and frequency of noise exposure. In clinical practice, most cases of presbycusis do not separate into a specific type but have mixtures of these pathologies (mixed presbycusis), and ~ 25% of all cases of presbycusis show none of the foregoing characteristics. This latter group was classified as indeterminate presbycusis.130 Based on histological observations, Schucknecht and Gacek highlighted the importance of stria vascularis atrophy and neuronal losses over sensory cell losses.130
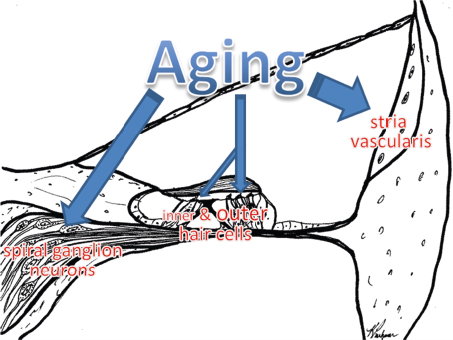
Other studies looking specifically at these classic categories have failed to establish a correlation between a pure-tone threshold pattern and structural abnormalities in the cochlea.132 For example, flat audiograms were associated with strial atrophy in Schucknecht’s scheme. However, Nelson and Hinojosa reported that this audiographic pattern was infrequently associated with strial atrophy, and more often occurred with outer hair cell loss alone or in combination with inner hair cell and spiral ganglion loss.132 In contrast, the classic downward-sloping audiogram has been associated with the extent of degeneration of the stria vascularis, inner and outer hair cells, and spiral ganglion cells.133 Ultrastructural features such as deformation of the cuticular plate in surviving hair cells134 or a peripheral neurite loss pattern135 may need to be considered in a full characterization of cochlear changes in presbycusis. Regardless of the debate on cochlear pathology–audiogram correlation, the notion that presbycusis arises from disruption of one or more of the key cochlear functional elements, including the inner and outer hair cells, spiral ganglion cells, and stria vascularis is widely accepted (Fig. 6.3).
Efforts at classification of audiograms of patients with age-related hearing loss can be aided by findings from animal models.136 The gerbil model of presbycusis has demonstrated that age-related hearing loss is not a sensory but a metabolic disorder. That is, hair cell losses are attributed to noise exposure; and in the absence of noise damage, age-related strial changes result in decreased endocochlear potential, which reduces cochlear sensitivity to a greater extent in the basal cochlea than in the apex. Using physiological findings in quiet-aged and furosemideexposed gerbils as the conceptual framework, the main audiometric phenotypes (sensory, metabolic, and mixed sensory/metabolic) are believed to be consistent with predictions from animal findings associated with sensory and strial pathology.136
 Central Presbycusis
Central Presbycusis
Peripheral changes are expected to produce secondary central changes. This would be consistent with a model of “maladaptive” neural plasticity in which degeneration of spiral ganglion afferents133 induces slow secondary neural loss further up the auditory pathway. Well-described peripheral auditory declines in the cochlea have been shown in mouse models of presbycusis to have direct and indirect consequences on the loss of neurons in the central auditory nuclei and potential reorganization of tonotopic mapping in the primary auditory cortex and multiple associated cortices.137–141 In older human listeners, there is a linear relationship between hearing thresholds and gray matter volume in the primary auditory cortex, suggesting that even moderate declines in peripheral auditory acuity lead to a systematic downregulation of neural activity during the processing of higher-level aspects of speech and may also contribute to loss of gray matter volume in the primary auditory cortex.142 In fact, individual differences in hearing sensitivity appear to predict the degree of language-driven neural recruitment during auditory sentence comprehension in the bilateral superior temporal gyri (including primary auditory cortex), thalamus, and brainstem for older listeners.142
However, not all of the central changes are due to hearing loss. For example, by controlling for hearing loss, one study demonstrated that age alone substantially reduces spatial release from masking.143 The finding that aging can affect the ability to use spatial and spectrotemporal cues to separate competing speech streams suggests age-related changes in the cortical and/or subcortical structures essential for spatial hearing are independent of hearing loss and points to the importance of central processing.
Perception comes from the Latin word percepio (to receive) and implies organization of sensory input. Perception leads to cognition, which comes from the Latin word cognoscere (to learn or know), implying interpretation and assigning meaning. To move from signal detection to signal recognition and interpretation requires cognitive processing, which occurs through interaction of subcortical auditory pathways and multiple cortical regions. These interactions are collectively referred to as central auditory processing. Central auditory processing is used for successful completion of more challenging auditory tasks such as detection of a signal in background noise. Such tasks become more complex in understanding speech, during which the listeners must perceive and attend to relevant speech features, such as the pitch, timing, and timbre of the speaker’s voice. Background or competing noise increases complexity of the task, further taxing central mechanisms. Performance of these tasks would be expected to be influenced by age-related changes in central auditory processing, as well as in cognitive function.
Although cognitive skills such as processing speed, memory functioning, and ability to divide attention diminish with age, older adults with normal hearing can compensate successfully for degradations in speech perception.144 It is believed that this compensation arises from linguistic skills and a lifetime of accumulated vocabulary. In addition, slowed speech bestows additional restoration benefit because it provides older listeners more time to process noisy speech and to use available cues from the speech signal more effectively. It is believed that older people use context effectively145 toward this goal. On the other hand, older listeners with sensorineural hearing loss demonstrate deficits in the ability to compensate for degraded speech, and the severity of this deficit appears to be determined by the severity of the hearing loss.146 Saija and colleagues suggest that newly demonstrated top-down restoration skills of older individuals may lead to the development of new cognitive training methods to cope with complex listening environments of everyday life,144 as in perception of interrupted speech.147
Functional magnetic resonance imaging (fMRI) has identified a core sentence-processing area located in the perisylvian region of the left cerebral hemisphere and an associated network of brain regions that support the working memory and other resources needed for comprehension of long or syntactically complex sentences in normal healthy older adults.148 This finding suggests that brain plasticity and compensatory neural recruitment contribute to maintenance of language comprehension with age. There are specific differences in activation of the auditory pathways observed through fMRI testing of speech listening in young and old listeners.149 Geriatric listeners show decreased activation of the auditory cortex compared with younger listeners, with even greater differences during speech listening in white noise compared with quiet listening. Specific sites of decreased activation included the anterior and posterior regions of the superior temporal gyrus bilaterally with particularly distinct differences within the posterior left superior temporal gyrus. Corpus callosum degeneration and resulting decreased interhemispheric neural transfer has also been implicated in asymmetric interaural responses during dichotic listening, with right-ear dominance frequently resulting.149
Further support for compensatory age-related changes in auditory processing comes from a recent study correlating hearing in quiet and noise with cortical structures evaluated with magnetic resonance imaging (MRI).150 In older adults, a decline in the relative volume and cortical thickness of the prefrontal cortex was associated with a declining ability to perceive speech in a naturalistic environment. This finding is consistent with the decline–compensation hypothesis, which states that a decline in sensory processing caused by cognitive aging can be accompanied by an increase in the recruitment of more general cognitive areas as a means of compensation.150 These compensatory mechanisms were also investigated using fMRI to compare neural processing of degraded speech between young and older adults.151 Older adults adapted to degraded speech at the same rate as young listeners, although their overall comprehension of degraded speech was lower, driven by a reduced dynamic range. Neurally, both older and young adults relied on the left anterior insula for degraded more than clear speech. However, older adults relied on the middle frontal gyrus in addition to a core speech comprehension network. Once again, these findings lead to the conclusion that older adults recruit cognitive control networks as a compensatory mechanism.151 The foregoing studies suggest that older listeners appear to be able to compensate for the impact of aging per se on the brain, so long as age-related pathological processes such as significant peripheral threshold elevations and possibly cerebrovascular and cognitive disorders (yet to be discussed) are not present.
In one of the earliest studies of central presbycusis, the progressive loss in central auditory competence measured by simultaneous binaural challenges and frequency and temporal distortion tests correlated with age.152 It was suggested that central presbycusis, in addition to the peripheral form, further compounds hearing disorders in older patients and accounts for hearing disability in noise or speech competitive environments. Although some of the difficulties of hearing in noisy environments can be accounted for by loss of peripheral sensitivity, age-related deficits in interhemispheric information processing also contribute.153 In older individuals when speech-in-noise perception is poor, deficiencies in the subcortical spectrotemporal representation of speech, including low-frequency spectral magnitudes and the timing of transient response peaks, can be demonstrated.154
A recent authoritative review emphasized that accumulating evidence supports the existence of central presbycusis as a multifactorial condition that involves age- and/or disease-related changes in the auditory system and in the brain.155 Dysfunction of central auditory processing is believed to contribute more significantly to the pathology of late presbycusis,126 making up a large component of presbycusis in people over 70 years of age.156
Some patients with central auditory processing disorder perform better with a single hearing aid in the better ear than with binaural aids.157 In noise, 71% of geriatric patients perform better with one hearing aid, rather than two.158 This might be due to an imbalance or asynchrony in binaural signal or a cognitive processing deficit and serves to highlight the importance of dichotic tests when evaluating any older patient with hearing loss.
Given the preceding implications of central presbycusis, the standard approach of treating ARHL through compensation of peripheral functional deficits (i.e., hearing aids and cochlear implants) may not be optimal. Some have promoted a more comprehensive management strategy for ARHL consisting of diagnostic evaluation that goes beyond conventional audiometric testing and includes measures of central auditory function, such as dichotic tasks and speech-in-noise testing.159 A more comprehensive approach is expected to bestow substantial advantages on rehabilitation of the geriatric patient with ARHL.160
Although a better understanding of central presbycusis is compelling because of its profound implications for auditory rehabilitation, the importance of this age-related process is further highlighted by the implications of the inherent relationship between central presbycusis and cognitive function. Gates and colleagues have shown that poor performance on the Synthetic Sentence Identification with an Ipsilateral Competing Message (SSI-ICM), one measure of central processing disorder, is common in people with AD.161 Using the SSI-ICM, in another study, a subset of older people from the Framingham Heart Study with normal cognitive screening test results on the Mini-Mental State Examination were identified to have very poor performance on the SSI-ICM (< 50% correct), yet normal word recognition in each ear. In this subset, the odds ratio for later diagnosis of dementia was over 12. This finding was interpreted as a common mechanism for AD and central processing disorder. Gates and colleagues reasoned that, because executive functioning is abnormal in people with AD and that many of the elements involved in central auditory processing, such as short-term memory, attention to task, and inhibition of unwanted signals, might involve executive functioning and undertook an examination of executive functioning and central auditory processing in another cohort. In that cohort, the significant relation of central auditory test results and the neuropsychiatric tests persisted even after adjustment for age, education, and pure-tone hearing thresholds, as well as, exclusion of AD cases.126 The prevalence of a poor central auditory test (including SSI-ICM) was 33% for the cognitively normal group, 80% for the memory-impaired group, and 90% for the AD group.
In summary, all “hearing” is a cognitive activity and difficult hearing environments (e.g., in the presence of background noise) can overload the cognitive aspects of understanding, especially when age and disease limit cognitive resources. Attention to central processes in evaluation of hearing loss has the potential to refine the current approach to rehabilitation and should include cognitive screening.
 Epidemiological Impact of Hearing Loss in Older Adults
Epidemiological Impact of Hearing Loss in Older Adults
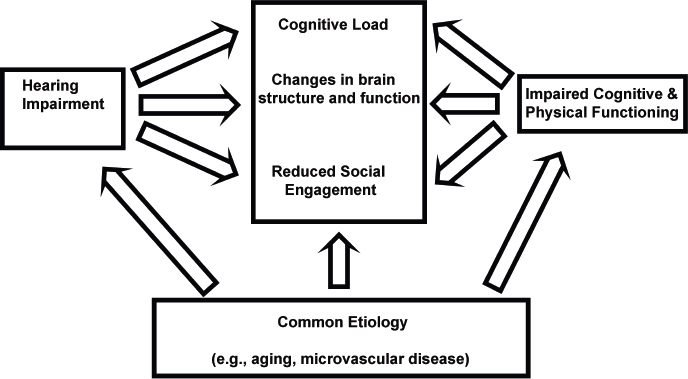
As already noted, a growing number of epidemiological and clinical research studies have demonstrated strong associations between hearing impairment and measures of cognitive functioning and health outcomes. A conceptual model through which ARHL could be mechanistically associated with these downstream outcomes that are critical to aging and public health is depicted in Fig. 6.4. Investigating the potential mechanisms that underlie these associations begins with an understanding that age-related hearing loss reflects progressive damage to cochlear structures from aging and other factors (e.g., noise, vascular risk factors) that results in poorer encoding of sound by the cochlea. Earlier, we identified common factors that could underlie a simple correlation between hearing and aging outcomes, such as age, vascular risk factors (e.g., diabetes, smoking), and demographic or social factors (e.g., education). In contrast, mechanistic pathways through which hearing impairment could contribute to poorer functioning include the effect of hearing impairment on cognitive load, brain structure, and decreased social engagement.