20 Advanced Cutaneous Malignancies in the Elderly
 Introduction and Epidemiology
Introduction and Epidemiology
Skin cancer is the most commonly diagnosed malignancy in the United States.1 The term cutaneous malignancy represents a diverse group of epithelial and nonepithelial cancers, but, generally speaking, the majority tend to be the result of cumulative sun exposure. As a person ages, the amount of ultraviolet (UV) light exposure accumulates, thus making age and cumulative UV exposure difficult to distinguish as independent risk factors. In a 2003 study by Godar et al, Americans were estimated to receive 22.73% of their lifetime UV exposure by the age of 18, 46.53% by the age of 40, and 73.71% by age 59; this study assumed a lifespan of 78 years, at which point it is assumed one would have received 100% UV dose. With current life expectancies of over 80 for men and women, sun exposure likely exceeds well beyond the maximum “dose.”2 This also argues for vigilant sun protection precautions regardless of age.
Age alone is recognized as a risk factor for developing certain cutaneous malignancies, particularly with regard to melanoma. The National Cancer Institute (NCI) Surveillance, Epidemiology and End Results (SEER) Program reports that 44.5% of newly diagnosed melanomas occur in individuals aged 65 years or older, with an additional 22% of new cases occurring in those 55 to 64 years.3 Although accurate epidemiological data on nonmelanoma skin cancers are not available, it is generally felt that this pattern of increasing incidence with age is also true for other cutaneous malignancies, such as squamous cell carcinoma (SCC) and basal cell carcinoma (BCC). It is worth making special mention of Merkel cell carcinoma (MCC) given its increasing incidence and association with advancing age. The incidence of MCC tripled from 1986 to 2001, and quadrupled by 20064,5; SEER data indicate an incidence of 0.6 per 100,000 annually in the United States. The majority of MCCs occur in the elderly, with a mean age of 72 years at diagnosis; only 5% of MCCs occur in patients younger than 50 years.6 Although sun exposure has been associated with MCC, more recently the Merkel cell polyomavirus has been implicated in the majority of MCCs. Although exposure to this virus tends to occur earlier in life, it is postulated that failure of immune surveillance with increasing age predisposes to the development of this malignancy.
Cutaneous malignancies tend to be readily curable when diagnosed early and treated with definitive surgery; the vast majority of these early cases are treated by dermatologists, never entering the purview of the otolaryngologist. More advanced skin cancers of the head and neck do require the expertise of head and neck surgeons for both resection and reconstructive surgery. Surgery remains the mainstay of treatment for most cutaneous malignancies and can range in extent from simple wide local excision to sentinel lymph node biopsy (SLNB), to parotidectomy and neck dissection. Reconstructive options may include skin grafts, local flaps, regional flaps, and free tissue transfer. Adjuvant radiation or chemotherapy may be considered, depending on final tumor stage and comorbidities.
This chapter focuses first on the management of the geriatric patient with an advanced cutaneous malignancy, reviewing the available literature to provide practical guidelines for perioperative care. This is followed by a brief review of the specifics of the major subtypes of skin cancer, including staging and treatment considerations.
 Preoperative Concerns
Preoperative Concerns
Many surgeons may experience reticence when evaluating an elderly patient for major surgery. Although a nonagenarian on the preoperative clinic schedule may inspire some trepidation, it is important to remember that chronological age is not as important as functional age. An 80-year-old retired professor who still walks the golf course is a different surgical candidate compared with a 70-year-old who is wheelchair-bound following a cerebral vascular accident. There are several tools for assessing surgical risk reasonably well in geriatric patients, and these would also apply to surgical risk for cutaneous malignancy: activities of daily living, instrumental activities of daily living, gait speed, exercise tolerance, frailty, and the comprehensive geriatric assessment. With respect to the specific risk advanced age poses to the surgical care of patients with advanced cutaneous malignancy, it is possible to draw some conclusions and make recommendations based on recent investigations for head and neck surgical care in the elderly.
Genther and Gourin recently investigated the outcomes of major head and neck surgery in the elderly, particularly with respect to the effect of comorbidity.7 Their retrospective analysis of a large sample of elderly head and neck cancer patients in the Nationwide Inpatient Sample sought to evaluate the impact of frailty in the surgical care of this group of patients. They accurately point out that age alone is not a good marker for health status and therefore sought to investigate the impact of “frail elderly” status on both short-term outcomes and cost of health care. Frail elderly is defined by the U.S. Census Bureau as “people 65 years or older with significant physical and cognitive health problems.”8 Genther and Gourin adapted this to be defined as patients 65 or older with a comorbidity score of 2 or higher using the Romano adaptation of the Charlson comorbidity index. In their sample of 61,740 patients, patients 80 years and older were more likely to have advanced comorbidity (most commonly cardiovascular and chronic pulmonary diseases); however, postsurgical complications did not differ significantly by comorbidity score and were reported at an overall rate of 11%. This includes no significant difference in wound complications or postoperative infections based on comorbid status alone. Frail elderly patients are indeed at an increased risk of acute medical complications as evidenced by the finding that these occur in only 18% of elderly patients without comorbidity, in 32% of patients with a comorbid score of 1, in 49% of those with a score of 2, and in 63% of those with a score of 3 or more (p < 0.01). Frail elderly patients were noted to be at significantly greater risk of acute cardiac and pulmonary events, acute renal failure, stroke, sepsis, pneumonia, and urinary tract infection. On multiple logistic regression analyses, risk of in-hospital death was associated with both age over 75 years and frail elderly status, as well as weight loss, major ablative procedures, and the use of pedicled or free flap reconstruction. Interestingly postoperative surgical complications were not associated with frail elderly status, although acute medical complications were. Finally, frail elderly status was significantly associated with greater length of stay (LOS) and increased hospital-related costs and need for advanced care following discharge, among other variables.7
Extrapolating this information to the treatment of advanced head and neck cutaneous malignancy in the elderly is not perfect for obvious reasons, but it may help define some guidelines when counseling patients for surgery. The Genther and Gourin study defined neck dissection alone as a “minor procedure.”7 If it is assumed that parotidectomy is not more complicated than neck dissection alone in terms of overall operative risk, then it follows that most surgery performed for head and neck cutaneous malignancy is indeed on the more “minor” end of the head and neck surgery spectrum in terms of overall operative risk and complications. This study noted that both in-hospital mortality and postsurgical complications were significantly associated with major ablative procedures and with cases requiring major flap reconstruction (both regional and free tissue transfer) in this elderly study group. This does not appear to be the case with more “minor” ablative surgery, such as neck dissection or parotidectomy, let alone SLNB and wide local excision. Thus there does not appear to be a robust reason to recommend against “minor” ablative surgery in the elderly based on procedure alone. That said, frail elderly status was associated with in-hospital death and acute postoperative medical complications; as always, functional age and comorbidity remain important considerations in assessing surgical risk.9,10
Generally speaking, it is recommended that healthy older patients with little to no comorbidity be treated no differently than younger patients who present with the same clinical stage and prognosis, because the literature does not support that age alone impacts outcome. For frail elderly patients however, standard of care treatment recommendations may bring risks that are not in line with the patient and family’s goals for treatment and quality of life. The literature cited earlier, while not specifically studying advanced cutaneous malignancies, gives surgeons a rough framework to begin the discussion of risks of perioperative death, acute medical complications, and need for advanced aftercare that many elderly patients are concerned about as they consider surgery for their advanced cutaneous malignancy. A frank discussion of prognosis, with respect to both the malignancy and any comorbidity, is imperative. Geriatric medicine consultation can be invaluable to help assess for coexisting geriatric syndromes and assist with advising the patient and family in decision making. A more palliative approach to treatment may be very appropriate in some frail elderly patients, but these alternative treatment strategies are best developed under the auspices of a multidisciplinary cutaneous malignancy team, which includes dermatologists, head and neck surgical oncologists, radiation oncologists, and medical oncologists.
 Operative Considerations
Operative Considerations
Although the various operative procedures for advanced cutaneous malignancy are not necessarily technically different when performed in the elderly, the operative management of these diseases is particularly well suited to the older patient. BCC and SCC are easily resected under local anesthesia as an office procedure in many cases. Mohs micrographic surgery is a well-established, safe operative technique for these malignancies as well. Although the dermatology literature is similar to the head and neck literature in its lack of prospective assessment of elderly patients, there are some early efforts to establish safety in Mohs for older patients.11,12 In many cases, wide local excision with margin analysis is all that is needed for treatment and, with same-day or staged reconstruction, can be performed under local anesthesia with or without conscious sedation, and entirely on an outpatient basis.
For the patients with melanoma and MCC, SLNB at the time of wide local excision may be indicated to assess for early regional metastases. Again, this is in many ways a procedure ideally suited to the elderly patient because it requires only a brief general anesthetic event and is routinely performed on an outpatient basis. The primary defect is reconstructed secondarily once final margins are cleared, and this can often be performed under local anesthesia, with or without sedation, as an outpatient, or at the time of completion lymphadenectomy should the sentinel node(s) be positive for metastasis.
If a patient requires parotidectomy and/or neck dissection for known regional metastasis, this is of course performed under general anesthesia and most often involves a short inpatient or observation stay. Working efficiently to minimize general anesthesia time is important in reducing operative risk, particularly in frail elderly patients.
Occasionally, patients with advanced cutaneous malignancy will require major head and neck reconstruction to address their ablative defect; in many institutions these are addressed with microvascular free tissue transfer. The literature for both ablative and free tissue transfer surgery in the elderly cutaneous malignancy patient is limited. The few cohort studies of free tissue use in elderly head and neck mucosal surgery patients are limited by low patient numbers and retrospective design, and only conclude that elderly patients are at higher risk for postoperative morbidity and require a thorough preoperative work up of any comorbid conditions.13 The need for free tissue transplant indicates an advanced primary malignancy requiring a lengthy surgical procedure. Involving geriatric medicine consultants in these cases is important in optimizing medical comorbidities prior to a major surgical event.
 Postoperative Care and Other Considerations
Postoperative Care and Other Considerations
As with the preoperative management of elderly advanced cutaneous malignancy patients, postoperative care must look beyond simple wound issues. The stress of surgery may unveil previously well-compensated issues, be they hearing loss, early dementia, or depression. Awareness of well-described geriatric syndromes (see Chapter 3) assists in safely managing patients through the perioperative period. Early consultation of geriatric medicine provides for effective multidisciplinary care. Occupational therapy and physical therapy are also excellent resources for patients who may experience temporary or permanent disability in the aftermath of their surgery.
Finally, thoughtful postoperative consideration of reconstruction and donor site choices in this patient population is very important. No two older patients will be quite alike; thus attention to the details of their overall functional status is critical to their quality of life and safety. For example, older patients tend to require glasses. Most of us would be unable to complete simple activities of daily living without being able to see, but in the elderly, this can be a safety issue as well. A patient who has had a paramedian forehead flap for nasal reconstruction may ultimately be pleased with her cosmetic result but will suffer if she cannot put on glasses for the weeks during which inosculation is taking place. The patient who requires a partial auriculectomy might have a similar issue not being able to wear a long-standing hearing aid while bolster dressings are in place and wound healing is ongoing. Optometrists and audiologists can offer adjustments to help patients get through the perioperative period of time safely and mitigate impact on quality of life.
 Disease-Specific Considerations
Disease-Specific Considerations
With the risk of cutaneous malignancy increasing with advancing age, a general review of diagnosis, staging, and treatment recommendations is helpful when approaching any patient with these cancers. There are many types of cutaneous malignancy; this chapter focuses on BCC, SCC, Merkel cell carcinoma, and melanoma.
Nonmelanoma Skin Cancer (NMSC)
Nonmelanoma skin cancer (NMSC) is the most common cancer in the United States, accounting for more malignancies than all other cancers combined. In 2006, ~ 2.1 million people were diagnosed with NMSC, compared with 1.4 million people with all other cancer types. Despite the high incidence of NMSC, these cancers are responsible for less than 0.1% of all cancer deaths.14,15
Basal Cell Carcinoma (BCC)
Basal cell carcinoma (BCC) is the most common cutaneous malignancy, accounting for ~ 80% of NMSCs. These lesions are of particular importance to the otolaryngologist because 80% of all BCC occurs in the sun-exposed head and neck region.16 The most important risk factor associated with the development of BCC is sun exposure in fair-skinned patients. In contrast to squamous cell carcinoma, which is related to cumulative sun exposure, basal cell carcinoma is more strongly related to intense intermittent UV exposure during childhood and adolescence. Other known risk factors include male gender, red or blond hair, light eye color, and immunosuppression. A personal history of BCC increases the risk of developing another BCC by a factor of 10.17
The most common form of BCC is nodular, which accounts for over 75% of all cases. These classic lesions present as a pearly papule or nodule with overlying telangiectasia and a rolled border with or without central crusting or ulceration. Superficial BCC is the second most common type, but it is usually seen on the trunk and extremities. The morpheaform type is rare, but almost all cases are found in the head and neck. It is characterized by invasion deeper into the dermis and is more aggressive than the nodular and superficial types. Other rare types include micronodular, infiltrative, and basosquamous, all of which are more aggressive variants associated with higher rates of local recurrence.
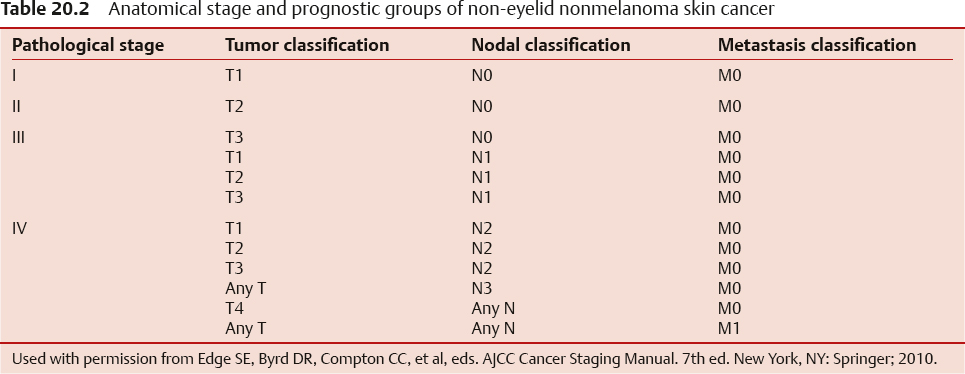
The American Joint Committee on Cancer (AJCC) staging of BCC is the same as for NMSC and is reviewed in Tables 20.1 and 20.2.17 The National Comprehensive Cancer Network (NCCN) stratified BCC into low-risk and high-risk groups based on their possibility for local recurrence—these risk factors are reviewed in Table 20.3.18 The risk of regional metastasis is quite low, ranging from 0.0028 to 0.55%.19
Table 20.1 TNM classification of non-eyelid nonmelanoma skin cancer
Tumor classification (T) | Characteristics |
T1 | ≤ 2 cm and < 2 high-risk features |
T2 | > 2 cm or ≥ 2 high-risk features |
T3 | Invasion of maxilla, mandible, orbit, or temporal bone |
T4 | Invasion of skeleton or perineural invasion of skull base |
Nodal classification (N0) |
|
N0 | No lymph node metastases |
N1 | Metastasis to single ipsilateral node ≤ 3 cm in greatest dimension |
N2a | Metastasis to a single ipsilateral node, 3–6 cm in greatest dimension |
N2b | Metastasis to multiple ipsilateral nodes, ≤ 6 cm in greatest dimension |
N2c | Metastasis to bilateral or contralateral nodes, ≤ 6 cm in greatest dimension |
N3 | Metastasis to a lymph node > 6 cm in greatest dimension |
Metastasis classification (M) |
|
M0 | No distant metastases |
M1 | Distant metastases |
Used with permission from Edge SE, Byrd DR, Compton CC, et al, eds. AJCC Cancer Staging Manual. 7th ed. New York, NY: Springer; 2010. Note: High risk features include > 2 mm thickness, Clark level ≥ IV, perineural invasion, primary site on the ear, primary site on nonhair-bearing lip, and poorly differentiated or undifferentiated. | |
Table 20.3 Risk factors for recurrence of basal cell carcinoma
H&P | Low risk | High risk |
Location/size | Area L < 20 mm Area M < 10 mm Area H < 6 mm1 | Area L ≥ 20 mm Area M ≥ 10 mm Area H ≥ 6 mm1 |
Borders | Well defined | Poorly defined |
Primary versus recurrent | Primary | Recurrent |
Immunosuppression | No | Yes |
Site of prior radiation therapy | No | Yes |
Pathology |
|
|
Subtype | Nodular,2 superficial | Agressive growth pattern3 |
Perineural invasion | No | Yes |
Adapted with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Basal Cell Skin Cancer V.1.2015. © 2015 National Comprehensive Cancer Network, Inc. All rights reserved. The NCCN Guidelines® and illustrations herein may not be reproduced in any form for any purpose without the express written permission of the NCCN. To view the most recent and complete version of the NCCN Guidelines, go online to NCCN.org. NATIONAL COMPREHENSIVE CANCER NETWORK®, NCCN®, NCCN GUIDELINES®, and all other NCCN Content are trademarks owned by the National Comprehensive Cancer Network, Inc. Area L: trunk and extremities (excluding pretibia, hands, feet, nail units, and ankles). Area M: cheeks, forehead, scalp, neck, and pretibia. Area H: “mask areas” of face (central face, eyelid, eyebrow, periorbital, nose, lips [cutaneous and vermilion], chin, mandible, preauricular and postauricular skin/sulci, temple, and ear, genitalia, hands, and feet). 1Location independent of size may constitute high risk in certain clinical settings. 2 Low risk histologic subtypes include nodular, superficial and other non-aggressive growth patterns such as keratotic, infundibulocystic, and fibroepithelioma of Pinkus. 3 Having morpheaform, basosquamous (metatypical), sclerosing, mixed infiltrative, or micronodular features in any portion of the tumor. | ||
Early and small tumors may be treated with simple excision or curettage and electrodissection. Because it is a common, slow-growing malignancy, the majority of BCC is treated by family physicians and dermatologists. However, locally aggressive tumors that are in proximity to functionally important and cosmetically sensitive anatomical structures are frequently referred to otolaryngologists. Surgical resection is the mainstay of treatment for lesions that are not amenable to curettage and electrodissection. Low-risk BCC should be excised with 4 mm margins. High-risk BCC may be treated with excision with wider margins and comprehensive intraoperative margin control. Mohs surgery remains the preferred treatment of high-risk BCC, because it allows intraoperative assessment of all margins and a 5-year disease-free survival rate of 99%. As is the case with all of the cutaneous malignancies discussed in this chapter, surgical margins should be discussed, because individual patient preferences may guide the treatment goals. In some cases, patients will accept closer margins to preserve function or cosmesis. In other cases, patients will decline surgery altogether and opt for radiation or targeted agents. Radiation therapy is usually reserved for patients with uncontrollable margins or for those who are poor surgical candidates.18
Patients with metastatic, multiply recurrent, or locally advanced BCCs now have another potential treatment modality in the form of a drug called vismodegib. Almost all BCCs have a loss of inhibition of the smoothened homologue (SMO) protein in the hedgehog signaling pathway, leading to uncontrolled proliferation of basal cells. Vismodegib is a novel targeted agent inhibitor of SMO that recently obtained Food and Drug Administration (FDA) approval based on the results of a phase 2 trial in patients with advanced BCC who had been previously treated with surgery, radiotherapy, and/or other systemic therapies. The metastatic disease response rate was 30%, and the locally advanced disease response rate was 43%. Both groups responded for a mean duration of 7.6 months, and 21% had complete responses. This hedgehog pathway inhibitor has been studied only in advanced, recurrent, and metastatic disease, and further study will elucidate its role, if any, in less advanced BCCs.20
Squamous Cell Carcinoma (SCC)
SCC is less common than BCC, representing ~ 10% of cutaneous malignancies. The risk of SCC is related to chronic, cumulative UV radiation exposure and is more commonly found in patients of northern European descent with fair skin (Fitzpatrick 1 and 2 skin types), light eye color, and a history of multiple sunburns.21 SCC incidence is increased in sunny climates close to the equator, and increased risk of SCC is noted in the elderly, in those with a history of previous cutaneous malignancy or premalignant lesion, and in male patients. Risk of SCC is also higher in patients with a history of previous radiation treatment or occupational radiation exposure22; elderly patients may have a history of radiation treatment to the skin for treatment of acne because this was a common approach to acne treatment between 1920 and 1960. Arsenic exposure is associated with an increased risk of both SCC and BCC; although not commonly seen as an etiologic agent, some geriatric patients may have been exposed to Fowler’s solution (potassium arsenic) in their youth, because this was a popular general tonic through the 1930s. SCC may also arise in the context of previous trauma, particularly burns and scars (e.g., Marjolin ulcer). Immunosuppression is widely recognized as a risk factor for SCC and portends more aggressive behavior of the cancer with increased rates of recurrence and metastasis.23 Human papilloma virus (HPV) has also been associated with the development of SCC, particularly in immunosuppressed populations.
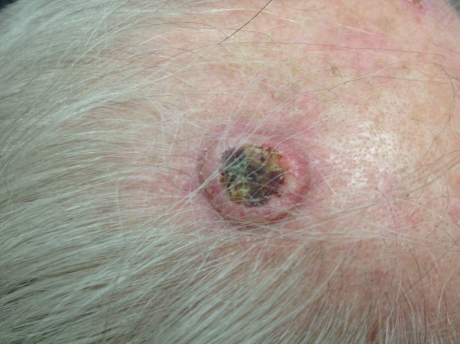
Clinically, SCC typically presents as an ulcerated, crusting lesion, often with a surrounding area of raised induration (Fig. 20.1). Staging of SCC is identical to that of BCC and is reviewed in Tables 20.1 and 20.2. SCC has a higher risk of both regional and distant metastasis compared with BCC, with a 10% occult metastasis rate24; nonetheless over 95% of nonmelanoma cutaneous malignancy will present as local disease only. The National Comprehensive Cancer Network (NCCN) has sought to define risk factors for aggressive behavior in SCC to help guide management. Most SCCs are low-risk and are diagnosed and treated at an early stage and under the auspices of dermatologists. Treatment of low-risk lesions would include definitive wide local excision, as well as judicious use of cryotherapy, electrotherapy, or photodynamic therapy in patients with early or in situ disease. High-risk SCC in the head and neck includes tumors that are 1 cm or larger on the cheeks, forehead, scalp, and neck, and tumors that are 6 mm or larger on the mask areas of the face, the chin/jawline region, and the periauricular region (Fig. 20.2). High-risk SCC parameters recognized by the NCCN also include the following: recurrent tumors; those with diffuse, poorly defined clinical borders; immunosuppression; previous radiation; rapid tumor growth; neurological symptoms or pathological perineural or perivascular invasion; and depth of tumor ≥ 2 mm. Poorly differentiated tumors and those of the adenoid, adenosquamous, and desmoplastic subtypes are also considered as potentially more aggressive.23,25