Acute Mastoiditis
Michael J. McKenna
Roland D. Eavey
Acute mastoiditis remains a contemporary disease with significant morbidity and even mortality. The clinical diagnosis of this disorder is so entrenched within the fabric of otolaryngology that it almost symbolizes the specialty. In the preantibiotic era, most patients with acute mastoiditis required surgical drainage. Although most cases can now be managed medically, morbidity and complications of acute mastoiditis continue to be reported.
With the development of newer antibiotics and modern imaging techniques, the diagnosis and treatment of acute mastoiditis and its complications is in constant evolution. Paradoxically, however, because of the comparative diminution in frequency of the disease, studies to test the efficacy of the newer antibiotics are more difficult. Therefore treatment cannot be standardized but must be based on the logical use of an expanding armamentarium.
Acute mastoiditis is defined in variable terms throughout the literature. Although different degrees of mastoid inflammation accompany episodes of acute and chronic otitis media, for purposes of this discussion acute mastoiditis is defined as an acute bacterial infection of the mastoid, often in association with a preceding acute otitis media, that exceeds mere mucosal involvement. Untreated, acute mastoiditis results in osteolytic changes of the mastoid trabeculae and cortex and extension beyond the tympanomastoid space.
As is the case with other bacterial infections, antibiotics have greatly reduced the morbidity and sequelae associated with acute otitis media. Prior to the advent of antibiotics, acute mastoiditis was among the most common admission diagnoses to a hospital. Davison (1) reported that the number of simple mastoid operations for acute mastoiditis at Geisinger Memorial Hospital in Pennsylvania dropped from 119 in 1937 to only 6 from 1951 to 1954, which he attributed to the use of sulfa drugs and, later, penicillin. In 1936, 45.9% of patients admitted to Los Angeles County Hospital with acute otitis media required mastoidectomy as compared with 17.6% of patients in 1946 (2). In 1959 the incidence of acute mastoiditis arising from acute otitis media was as low as 0.4% in a series of 12,000 cases reported by Palva et al. (3). An excellent analysis of the influence of sulfa drugs and penicillin on acute mastoiditis was provided by Rudberg in 1954 (4). With conservative therapy of acute otitis media, the percentage of patients who required surgery in various series ranged from 9.3% to 69.5%. With the introduction of sulfa drugs, the need for mastoidectomy dropped to a range of 1.5% to 28% for the same institutions.
The incidence of serious complications due to acute mastoiditis, including brain abscess and meningitis, has also declined substantially since the introduction of antibiotics (5). Improved imaging modalities in the form of computed tomography (CT) and magnetic resonance imaging (MRI), along with improved surgical technique, have significantly reduced the fatal and serious neurologic sequelae associated with brain abscesses and meningitis.
Despite the influence of antibiotics on the overall incidence of acute mastoiditis, it is by no means a rare disorder of only historical significance. The emergence of resistant strains of bacteria, an increased incidence of gram-negative infections, and a reduced clinical experience justify the consideration of acute mastoiditis as among the most serious and life-threatening infectious disorders of the head and neck. In addition, present concerns surrounding the overuse of antibiotics and even the need to treat acute otitis media with antibiotics may lead to a resurgence of complications (6,7).
RELEVANT ANATOMY OF THE MIDDLE EAR AND MASTOID
The middle ear and mastoid are contiguous spaces connected by the aditus ad antrum. Pneumatization of the temporal bone begins at birth with aeration of the eustachian tube and tympanic cavity. By 4 weeks of age, a central antral air cell is present. If undisturbed by infection or inflammation, pneumatization will proceed with expansion from the antrum and epitympanum into the zygomatic root, mastoid process, and perilabyrinthine areas. Mastoid pneumatization progresses by resorption of bone adjacent to aerated spaces. Details of the pneumatized spaces of the temporal bone are
described in Chapter 11. Pneumatization may be slowed or arrested by infection, which disturbs the physiologic relationship between the mucosa and underlying bone. This arrest of pneumatization may have a partially protective effect in limiting the spread of infection to surrounding structures. In the infant, the lateral mastoid cortex over the mastoid antrum is cribriform in character, and hence infections of the middle ear and antrum readily spread to the postauricular soft tissue.
described in Chapter 11. Pneumatization may be slowed or arrested by infection, which disturbs the physiologic relationship between the mucosa and underlying bone. This arrest of pneumatization may have a partially protective effect in limiting the spread of infection to surrounding structures. In the infant, the lateral mastoid cortex over the mastoid antrum is cribriform in character, and hence infections of the middle ear and antrum readily spread to the postauricular soft tissue.
The stylomastoid foramen in the infant is in a lateral position, unprotected by the mastoid process, which begins to develop during the second year of life. Therefore the standard postauricular incision must be modified to avoid injury to the facial nerve.
PATHOPHYSIOLOGY OF ACUTE MASTOIDITIS
Acute mastoiditis most commonly results as the sequela of acute otitis media or, less commonly, complicates chronic otitis media with cholesteatoma (8), leukemia, mononucleosis, sarcomatous lesions of the temporal bone, and Kawasaki’s disease (9, 10, 11, 12). With prolonged inflammation, the mucoperiosteum becomes hyperemic and edematous, causing obstruction and sequestration of the infection. Obstruction may occur in the aditus ad antrum or in other smaller periantral tracts. As pus begins to accumulate under pressure, active bone remodeling with osteoclastic bone resorption occurs. As a result, much of the calcified trabecular network and periosteal bone may be replaced by noncalcified woven bone, which is soft and richly vascularized, and may simulate necrotic bone and granulation tissue. At this stage the radiographic appearance of the mastoid begins to change; it is often referred to as the coalescent stage of acute mastoiditis. These bony changes involve the mastoid trabeculae, as well as the thin plates of cortical bone that separate the mastoid air cells from the middle cranial fossa, the sigmoid sinus, the external auditory canal, and the postauricular soft tissues. The clinical diagnosis of acute mastoiditis is usually made when the infection spreads beyond the tympanomastoid space to the soft tissues of the postauricular region. Complications of acute mastoiditis are the result of spread of infection to the intracranial cavity, the sigmoid sinus, the labyrinth, the fallopian canal, or the soft tissues of the neck.
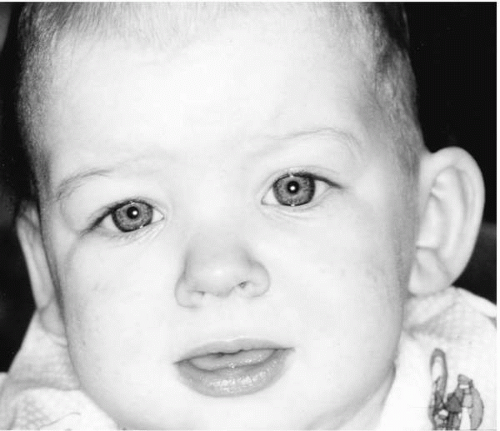
Acute mastoiditis may occur in the absence of an obvious middle ear infection when an aditus block segregates the middle ear and the mastoid air cells. Usually there is an antecedent acute otitis media with apparent resolution of the middle ear process followed by activation of a smoldering mastoid infection. Extension through the postauricular cortex results in a cellulitis of the postauricular soft tissues with protrusion of the auricle (Fig. 16.1). When breakthrough occurs in the zygomatic root, the auricle is deflected inferiorly by cellulitis or abscess formation. Extension through the posterior wall of the external auditory canal results in sagging of the external canal skin. When the tympanic membrane is intact, this presentation may be confused with an acute external otitis. A Bezold abscess occurs deep to the sternocleidomastoid muscle when infection breaks through the mastoid tip.
MICROBIOLOGY
The organisms responsible for acute mastoiditis are not identical to those found in acute otitis media.
In one series of 35 consecutive cases of acute mastoiditis reported in 1987 by Maharaj et al. (13), mixed cultures of aerobes and anaerobes were the most common. Occasionally, anaerobes were the sole organism isolated. Most common anaerobes included gram-positive cocci, gram-positive bacilli, and gram-negative bacilli. The most common aerobes were group A beta-hemolytic Streptococcus, Staphylococcus aureus, Proteus mirabilis, Staphylococcus epidermidis, and Pseudomonas aeruginosa. Haemophilus influenzae and Streptococcus pneumoniae, common in acute otitis media, were uncommon in acute mastoiditis.
Other investigators have reported less disparity between cultures in acute otitis media and acute mastoiditis. In a study of 30 children with acute mastoiditis between 1973 and 1984, cultures were positive for S. pneumoniae in 7, S. epidermidis in 5, H. influenzae in 3, group A beta-hemolytic Streptococcus in 3, anaerobes in 3, S. aureus in 3, and P. aeruginosa in 1 (14). Predominance of S. pneumoniae was found by Prellner and Rydell (15). However, the remaining organisms were almost evenly divided between H. influenzae, beta-hemolytic Streptococcus, S. aureus, P. mirabilis, and Pseudomonas and Bacteroides species. The bacterial spectrum of acute otitis media has changed radically in the last half of the twentieth century. Prior to 1940, almost half the cases of acute mastoiditis were caused by a group A
beta-hemolytic Streptococcus compared with a 0% to 10% incidence from 1970 to 1983. In addition, there is evidence to suggest the serotypes of pneumococcus isolated from patients with acute otitis media have changed over time (16). Although the incidence of acute mastoiditis caused by Mycobacterium tuberculosis has declined, there has been an increase in acute otitis media and mastoiditis caused by Mycobacterium fortuitum (17) and Mycobacteria chelonae (18). It is also uncertain whether these changes are in part responsible for the decline in the incidence and severity of acute mastoiditis.
beta-hemolytic Streptococcus compared with a 0% to 10% incidence from 1970 to 1983. In addition, there is evidence to suggest the serotypes of pneumococcus isolated from patients with acute otitis media have changed over time (16). Although the incidence of acute mastoiditis caused by Mycobacterium tuberculosis has declined, there has been an increase in acute otitis media and mastoiditis caused by Mycobacterium fortuitum (17) and Mycobacteria chelonae (18). It is also uncertain whether these changes are in part responsible for the decline in the incidence and severity of acute mastoiditis.
DIAGNOSIS AND MANAGEMENT OF UNCOMPLICATED ACUTE MASTOIDITIS
Diagnosis, Signs, and Symptoms
In its most classic presentation, acute mastoiditis is readily diagnosable (19). The clinical diagnosis is based heavily on history and physical examination. It occurs more commonly in children than adults and may occur with or without a history of recurrent infections. Physical findings include pain, swelling, and tenderness over the mastoid process with proptosis of the auricle. Other common findings include fever and sagging of the superior external canal skin. At times this clinical picture may be difficult to distinguish from severe external otitis with retroauricular extension. However, diffuse pain and inflammation of the external canal is usually a more prominent feature in external otitis than in acute mastoiditis. Evaluation of the patient should include a complete physical examination in addition to otolaryngologic evaluation. Neurologic evaluation should include examination of the cranial nerves; relevant motor, sensory, and cerebellar examination; and a search for meningeal signs and nystagmus. Acute mastoiditis occurs without obvious abnormalities of the tympanic membrane or middle ear in 10% to 20% of cases. This unusual finding results from blockage of the aditus ad antrum from edematous mucosa, causing an anatomic partition of the tympanomastoid compartment with resolution of infection within the tympanic cavity.
Laboratory Investigation
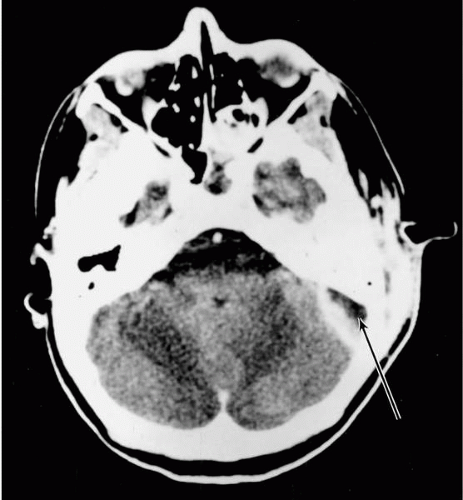
Mastoid radiographs are of limited value in confirming the diagnosis, particularly early in the course of the disease. Radiologic evidence of coalescence of the mastoid trabeculae occurs late in the course of the acute illness and days after active remodeling has begun. CT scans usually demonstrate clouding of the mastoid air cells, a nonspecific finding that also occurs in serous, acute, and chronic otitis media (Fig. 16.2). The greatest utility of CT and MRI is in the evaluation of possible complications such as epidural abscesses (Fig. 16.3), brain abscesses, and lateral sinus thrombosis (Fig. 16.4).
Audiometry or auditory evoked response testing should be obtained if the patient’s condition permits. Laboratory examination should include a complete blood cell count (CBC) with a differential white cell count and blood cultures.
 FIG. 16.2 CT scan of an infant with acute mastoiditis demonstrating the single mastoid cell involvement (arrow). |
Because there is a broad spectrum of organisms and antibiotic sensitivities in acute mastoiditis, an attempt should be made to obtain pus for Gram stain and aerobic and anaerobic culture and sensitivity. In cases with accompanying otorrhea, the ear canal should be cultured after gentle cleansing with sterile saline. In cases with an intact tympanic membrane and evidence of middle ear effusion, a wide
myringotomy ideally should be performed, followed by culture of the middle ear contents. Insertion of a tube can assist with drainage, as will administration of a topical antibiotic. In the mildest cases, especially if the middle ear is not yet involved, empirical antibiotic selection is appropriate.
myringotomy ideally should be performed, followed by culture of the middle ear contents. Insertion of a tube can assist with drainage, as will administration of a topical antibiotic. In the mildest cases, especially if the middle ear is not yet involved, empirical antibiotic selection is appropriate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree