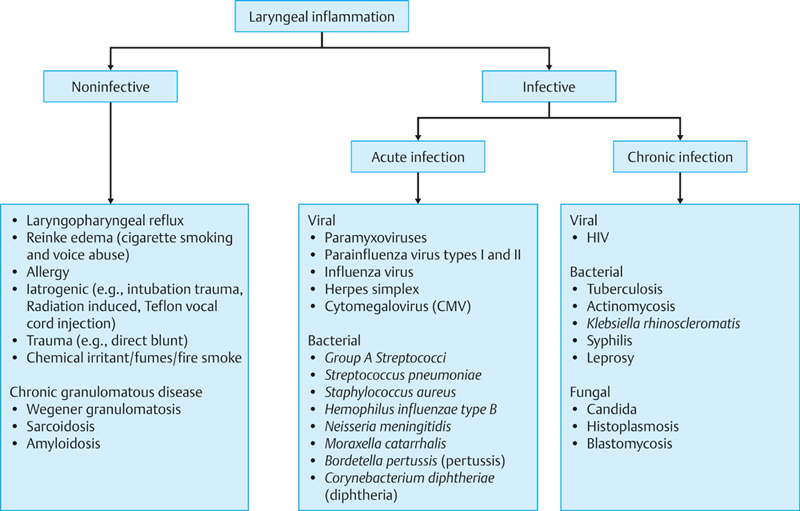
22 Acute Inflammatory and Infective Disorders of the Larynx The larynx is the narrowest part of the upper airway and is situated just anterior to the opening into the esophagus. This anatomical position means that the larynx is constantly exposed to the external environment, predisposing it to infection, environmental irritants, and potential gastric contents from gastroesophageal reflux. Edema or swelling of the larynx from inflammation can also potentially result in life-threatening upper airway obstruction. The causes of laryngeal inflammation can broadly be divided into noninfective and infective. This can be further classified as shown in Fig. 22.1. The majority of noninfective inflammatory conditions of the larynx are chronic and some are described here as they form part of the differential diagnosis when patients present acutely with a short history. Patients of all ages can present with symptoms and signs suggestive of laryngeal inflammation. History should specifically cover throat symptoms, past medical illnesses, medication history, smoking and alcohol history, and occupation. Laryngeal or throat symptoms include sore throat, dysphonia, dysphagia, odynophagia, globus sensation, repeated throat clearing, history of heartburn, cough, hemoptysis, and difficulty breathing or stridor. The patient may volunteer experience of laryngospasm during daytime or woken up from sleep at night. Any history of heartburn or gastroesophageal reflux disease and treatment regimen should be thoroughly explored. History of any weight loss is indicative of true dysphagia and may require radiological investigation such as contrast swallow. Dietary history is important and may be perpetuating laryngopharyngeal reflux (LPR). The oral cavity and oropharynx examination should be performed. Flexible nasolaryngoscopy examination of the tongue base, larynx, and hypopharynx is mandatory for diagnosis and for excluding malignancy. Photographic documentation is recommended for record and future comparison. Bilateral neck examination to exclude cervical lymphadenopathy and malignancy should also be performed. LPR1 is the backflow of gastric acidic refluxate, containing hydrochloric acid, pepsin, bile acids, bacteria, and pancreatic proteolytic enzymes, into the upper aerodigestive tract, resulting in damage to the thin laryngeal mucosa. The refluxate could take the form of either liquid or gas aerosol. Refluxate pepsinogen/pepsin attached to laryngeal mucosa has been shown to be the main culprit causing proteolytic tissue damage. Pepsinogen is converted to pepsin (active form) when pH drops below 4 and deactivated only when pH rises above 8. The resulting laryngeal mucosa damage may give rise to symptoms such as globus sensation, pseudodysphagia, need for repeated throat clearing, cough, postnasal drip or “catarrh,” sore throat, and dysphonia. Flexible nasolaryngoscopy examination reveals erythema and edema of both arytenoids, postcricoid region, and posterior commissure (Fig. 22.2). Vocal cord edema and pseudosulcus may also be visible. Diagnosis is usually by history and examination. Contrast swallow could be used if there was suspicion of pharyngeal pouch, obstructive lesions, or esophageal malignancy. The reflux symptom index (RSI) is a patient self-assessment tool with regard to the severity of LPR. The RSI score is useful in both diagnosis and monitoring response to treatment over time. Figure 22.2 Laryngopharyngeal reflux showing postcricoid edema and significant posterior commissure hypertrophy. (Image courtesy of Mr. Mark Watson.) All patients should be advised on lifestyle modifications, which have been shown to help. This includes avoiding food late at night, fatty food, and low pH drinks such as fizzy drinks and fruit juices. Depending on the severity of the disease, they could be prescribed liquid alginate preparation alone (to be taken after meal and before bedtime) or in combination with a low- or high-dose proton pump inhibitor (PPI; to be taken half an hour before meal and twice a day to ensure 24-hour cover). It may take up to 2 to 3 months before any benefit is realized and treatment may need to continue for up to 6 months. The dose of the PPI can be tailed off subsequently. For patients who fail to respond to antireflux medical treatment, it may be useful to consider 24-hour dual-channel pH monitoring or multichannel intraluminal impedance measurement to establish objective evidence of reflux before embarking on surgical management such as fundoplication. Clinical Pearl •A high degree of suspicion for neoplasm should be maintained in high-risk patients who may present with symptoms of LPR. Reinke edema from cigarette smoking and voice abuse2 is a form of chronic inflammation affecting the membranous portion of the vocal cords as a result of smoking and voice abuse. The inflammatory process results in fluid accumulation within Reinke space, hence Reinke edema. Reinke space is the potential space between the basement membrane of the nonkeratinizing stratified squamous epithelium and the superficial lamina propria. Patients are typically smokers and present with dysphonia with reduced pitch. Female patients may complain that they are regularly mistaken for a man when having telephone conversation. Flexible nasolaryngoscopy would reveal diffuse edematous vocal cords with redundant floppy vocal fold mucosa. Significant swelling from Reinke edema may also result in stridor and acute airway obstruction requiring intubation/tracheostomy and urgent surgery (microlaryngoscopy with cold-steel technique or laser) to drain fluid from Reinke space and reduce any excess mucosa, without damaging the superficial lamina propria and vocal ligaments. Clinical Pearl •Unilateral Reinke edema would warrant exclusion of neoplasm. Generalized allergic reaction or exposure to inhalants could trigger a type I hypersensitivity reaction leading to acute edema of the glottis or supraglottis, resulting in stridor and acute airway obstruction. Careful and close monitoring of respiratory function and pulse oximetry will be required. Immediate withdrawal and avoidance of the known allergen is indicated. Acute airway management with systemic steroids, intramuscular adrenaline, nebulized adrenaline, heliox, and antihistamine should be considered. Intubation (anesthetic involvement), cricothyroidotomy, and emergency tracheostomy may be required to secure airway. Toxic fumes and fire smoke can result in acute edema of the larynx. Black soot can be seen in the oral cavity and oropharynx following fire smoke inhalation. It is crucial that these patients’ airway is monitored closely since laryngeal edema can develop very quickly resulting in impaired visualization of the laryngeal inlet. At-risk patients should be intubated early in Accident and Emergency to secure their airway and to reduce the risk of intubation trauma while the laryngeal inlet is still visible. Blunt trauma of the larynx can result in hematoma and trigger an inflammatory response resulting in laryngeal soft-tissue swelling. Airway obstruction is a danger and acute airway management as per allergy is indicated. Unstable fractured laryngeal framework should be surgically repaired after airway is secured. The use of inhaled corticosteroids (ICSs)3 in the treatment of asthma and chronic obstructive airways disease (COAD) is widespread. Increased dose of ICS has a positive correlation with local and systemic side effects. Systemic side effects occur because 80% of the dose delivered by conventional metered-dose inhaler is swallowed.3 Symptomatic local side effects occur in up to 5 to 10% of patients treated with ICS.3 These include oropharyngeal and laryngeal candidiasis (described further in section “Fungal Infection” later in the chapter) and nonspecific inflammation of the laryngopharyngeal mucosa. These local side effects are multifactorial and related to the steroid preparations, proinflammatory effect of the propellant and lubricant constituents of the ICS, mechanical irritation because of cough, and possibly the intrinsic high susceptibility for inflammatory response of the upper airway in asthmatic and COAD patients. These patients tend to present with hoarseness, cough, and sore throat. Flexible endoscopy may reveal erythema and white patches on the larynx. Treatments include advising patients to rinse their mouth with clear water following ICS use, education on proper inhaler use technique, and using a spacer device. Improved inhaler device design with more effective delivery mechanism has been developed, such as the breath-actuated inhalers. Some patients will benefit from replacing the metered-dose inhalers with dry powder inhalers (DPIs) since DPI does not require propellants and rely on the patient’s inspiratory effort for drug delivery to the lungs. It is not uncommon to see laryngeal edema and erythema following chemoradiation of the laryngopharyngeal area. Flexible laryngoscopy shows pale or erythematous swelling of the supraglottic region and saliva pooling. It can sometimes be difficult to interpret between postradiation changes and possible residual or recurrent malignant disease. In addition, it could also be due to candidal infection.4 Postoncological magnetic resonance imaging and close monitoring with regular photographic evidence of the larynx for comparison during follow-up can help in deciding the need for biopsy. Empirical treatment of possible laryngeal candidiasis could also be tried. Severe persistent swelling following chemoradiation may be due to permanent impaired lymphatic drainage. It would be wise for the patient to stop smoking and keep adequate vocal hygiene. Antireflux medication can be considered. Short courses of high-dose steroids may help reduce laryngeal edema and temporarily improve breathing. The patient may have swallowing impairment, aspiration, and airway obstruction in severe cases requiring tracheostomy. At times, laryngectomy may be the only option for an incompetent nonfunctioning larynx. Teflon (polytetrafluoroethylene) injection in the past for vocal cord medialization has now been discontinued since the early 1990s given its high rate of complications including granuloma formation, implant migration, severe scarring, overinjection, and airway obstruction.5 Injection of Teflon into the vocal cords will allow it to infiltrate into all layers of vocal folds and laryngeal muscles causing foreign body granulomatous local inflammatory reaction, resulting in stiff vocal folds and subsequent poor voice outcome in the medium and long term. Surgical removal of Teflon granulomas was highly unsatisfactory given its diffuse presence and scarred vocal folds. Removal tends to be incomplete and associated with recurrent formation and granulomas requiring multiple surgeries.5 Apart from autologous fat, safer and more widely used implant materials nowadays include silicone, hyaluronic acid, bovine collagen, hydroxyapatite, and Gore-Tex (expanded polytetrafluoroethylene). This generally refers to Wegener’s granulomatosis and sarcoidosis. Management of these patients should involve a rheumatologist. Laryngeal involvement by Wegener’s typically affects the subglottic area. In the active phase, flexible laryngoscopy may reveal laryngeal erythema reflecting acute inflammation. Cytoplasmic antineutrophil cytoplasmic antibodies serology may be positive. Treatment is with corticosteroids or steroid-sparing immunosuppressants. Subglottic stenosis from scarring may result following resolution. Sarcoidosis is a systemic granulomatous disease. Involvement of the larynx can give rise to a granulomatous appearance mimicking laryngeal tuberculosis, fungal laryngitis, or squamous cell carcinoma. Chest imaging, serum angiotensin-converting enzyme level, and serum calcium level may help with the diagnosis. Treatment is with corticosteroids or steroid-sparing immunosuppressants. This is a viral infection of the respiratory tract that mainly affects children aged between 6 months and 6 years.6 Common pathogens are parainfluenza virus, respiratory syncytial virus, adenovirus, and influenza A virus. Diagnosis is clinical and they present with fever, coryza, and cough. Differential diagnoses to be considered include foreign body inhalation and epiglottitis. A chest X-ray may show subglottic edema characterized by the “steeple sign.” Nasopharyngeal aspirate for viral antigen detection can be considered. Most croups are mild with no airway compromise and can be treated with humidified air at home. A child with stridor and reduced saturation should be treated with care—avoid upsetting the child and keep the child in upright position, give oxygen, and administer oral corticosteroids and nebulized adrenaline.7 Intubation and ventilation may occasionally be required. Supraglottitis, including epiglottitis, is an acute bacterial infection of the supraglottis resulting in supraglottic inflammation, with the potential to progress rapidly to acute airway obstruction. Common pathogens include Haemophilus influenzae type b (Hib), Neisseria meningitidis, group A streptococci, Streptococcus pneumoniae, Staphylococcus aureus, and Klebsiella pneumoniae.8,9 The introduction of Hib vaccine in 1985 has resulted in marked decrease in the incidence of epiglottitis in children. The incidence of adult epiglottitis has remained relatively stable at 2.3/100,000 per year.10 The patient is typically systemically unwell with pyrexia and tachycardia. They present with sore throat, dysphagia, odynophagia, hoarseness, drooling, and respiratory distress. Flexible nasolaryngoscopy shows erythema, swelling, and blisters of the epiglottis and supraglottis (Fig. 22.3). The larynx is tender on palpation. Readers are reminded that it is not uncommon for patients with sore throat due to supraglottitis to be referred as “tonsillitis.” The cognizant doctor would always perform a flexible nasolaryngoscopy to examine the larynx and supraglottis when the tonsils appeared normal on oral and oropharynx examination.
Clinical Assessment
Noninfective Laryngitis
Laryngopharyngeal Reflux
Reinke Edema from Cigarette Smoking and Voice Abuse
Allergy
Environmental Irritants
Direct Trauma
Iatrogenic
Inhaled Corticosteroids
Chemoradiation-Induced Laryngitis
Foreign Body Reaction
Chronic Granulomatous Disease
Infective Laryngitis
Acute Viral Infection
Laryngotracheobronchitis (Croup)
Acute Bacterial Infection
Supraglottitis and Epiglottitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree