Acquired Deformities of the Auricle
Mack L. Cheney
Tessa A. Hadlock
PRINCIPLES
Reconstruction of the auricle poses many challenges for the reconstructive surgeon. The goals of reconstruction are to achieve normal appearance and sensation of the structure. It should be symmetric with the contralateral ear in size, shape, and orientation; it should be in proper relation to the periauricular skin and scalp; and the postauricular sulcus should be preserved. However, the intricate anatomy of the auricle makes these goals quite difficult to attain. The auricle’s complex, three-dimensional convolutions are supplied by limited and inconsistent vascularization, and the ratio of cartilage to skin is high. In addition to the inherently complex anatomy of the “typical” ear, there exists a wide degree of variation among individuals (1, 2, 3).
The presence of supple and well-vascularized skin is essential for success in auricular reconstruction. Cutaneous resurfacing is often necessary in the management of acquired auricular deformities, because auricular injuries are often combination injuries to the skin and underlying cartilage. In this situation, the scar tissue that affects the skin must be excised and replaced to allow for adequate three-dimensional reconstruction. The reconstruction of auricular defects after oncologic surgery requires special consideration because reconstructive plans are influenced by the nature of the excisional defect, the presence or absence of an irradiated field, and the need for careful clinical monitoring of the area.
Although auricular reconstruction poses unique challenges to the surgeon, many of the principles of reconstruction of other areas of the head and neck also apply to the auricular region. Anatomic landmarks such as the vermilion border, eyebrow, nasal alar margin, and ear constitute free margins due to the discontinuity of skin borders surrounding these structures. Because such margins offer little or no resistance to tension created by surgical procedures in adjacent soft tissue, the immediate and delayed consequences of tissue manipulation must be anticipated. The helix of the ear does not have the same cosmetic importance as other free margins of the face, because slight asymmetries are not always noticeable or can be camouflaged by changes in hairstyling. On the other hand, auricular cartilage is very supple and soft tissue contraction forces will tend to distort the ear if attention is not paid to primary closure and to local tissue tension.
Reconstruction in the auricular area must take into account hair-bearing scalp in the proximity to avoid placing hair-bearing skin over the auricle. The hairline above the site of the proposed reconstruction is usually high enough to avoid interfering with accurate positioning of the ear. The exception to this is when placing hair-bearing skin is necessary to achieve normal height with respect to the contralateral ear.
ANALYSIS OF THE AURICLE
Analysis of the dimensions and proportions of the external ear are important for planning reconstructive procedures (4). Leonardo da Vinci first noted that the vertical height of the ear is approximately equal to the distance between the lateral orbital rim and the root of the helix at the level of the brow. Ear width is approximately 55% of its length, the helical rim protrudes 1 to 2.5 cm from the skull, and the angle of the protrusion from the skull averages 25 to 30 degrees. The vertical axis of the ear is inclined posteriorly at an angle of approximately 20 degrees from the vertical. When planning the reconstruction, however, it is most important to use the contralateral side as a template because individual variation is the rule rather than the exception in anatomic auricular features and location (5) (Table 46.1).
TABLE 46.1 Average length and width of the normal auricles | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
ANATOMY AND EMBRYOLOGY
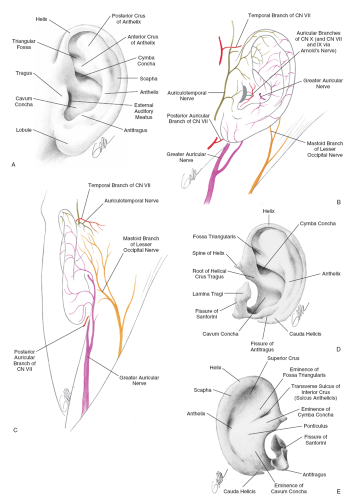
Anatomic landmarks of the auricle are important when considering reconstructive options (7). Topographic landmarks of the auricle are illustrated in Fig. 46.1. The cartilaginous framework of the auricle must be thought of in terms of three-dimensional components. The cartilaginous units, starting medially, are the conchal complex, the anthelical and antitragal complex, and the helical and lobular complex.
Embryologically, the auricle arises from the first (mandibular) and second (hyoid) arches. The helix appears in these arches during the sixth week of gestation. The anterior hillocks give rise to the tragus, the root of the helix, and the superior helix, whereas the posterior hillocks become the anthelix, tragus, and lobule.
The arterial supply to the auricle is derived from branches of the superficial temporal artery and the postauricular artery, both of which arise from the external carotid artery. The venous drainage is via the postauricular vein into the external jugular system, with additional support from the superficial temporal and retromandibular veins.
The auricle is innervated by the great auricular nerve (C2-3), auriculotemporal nerve (V3), lesser occipital nerve, and greater branch of the vagus nerve (Arnold’s nerve).
USE OF COSTAL CARTILAGE AS A FRAMEWORK FOR AURICULAR RECONSTRUCTION
By fashioning a new auricle or portions of it from autogenous costal cartilage, the surgeon can avoid the use of auricular prostheses or alloplastic implants. Prostheses pose a problem with adherence to the skin, and patients tend to prefer reconstructions that utilize autogenous materials. Additionally, alloplastic implants have been shown in many reports to exhibit an unacceptably high extrusion and infection rate. Although autogenous tissue reconstructions are preferable, the ribs become more brittle and ossified with age, so reconstruction utilizing costal cartilage must be carefully considered in patients more than age 50 years.
The cartilaginous components of the sixth, seventh, and eighth ribs provide the raw material for the creation of the framework. The synchondrosis between the sixth and seventh ribs serves as the body of the framework, whereas the helix is fashioned from the eighth rib. As with the techniques used in microtia repair, determination of the appropriate size and individual shape of the framework is taken from a pattern of the contralateral auricle. The cartilage framework is stabilized and properly positioned based on preoperative measurements. A temporoparietal fascial flap is commonly used to cover the cartilage framework to ensure viability and to accept a split-thickness skin graft.
TEMPOROPARIETAL FASCIAL FLAP
In the cover of the cartilaginous framework in auricular reconstruction, the tissue used should be thin, vascular, hairless, and capable of accepting skin grafts of a good color match. The temporoparietal fascial flap (9, 10, 11, 12, 13, 14) satisfies these requirements, with the added advantages that the anatomy of the flap is well known to the head and neck surgeon (15,16), a large quantity of tissue (14 by 12 cm) can be harvested, it can be rotated to cover a wide range of auricular defects, and the flap may be transferred to the contralateral auricular region using microvascular techniques (17).
The temporoparietal fascia, also known as the superficial temporal fascia, is continuous with the superficial musculoaponeurotic system, as well as the galea (Fig. 46.2). It lies deep to the skin and subcutaneous tissue to which it is firmly bound (particularly in the area of the temporal line). This fascia should not be confused with the fascial layer surrounding the temporalis muscle proper. The temporoparietal fascia attaches to the zygomatic arch, whereas the temporalis muscular fascia passes deep through the arch to insert on the coronoid process of the mandible. Measuring on average 2 to 3 mm in thickness over the parietal area, the temporoparietal fascia is highly vascular, with an abundant and consistent supply from the superficial temporal artery and vein.
In harvesting the flap, care must be taken to keep the hair follicles and subcutaneous fat on the lateral aspect of the flap under direct vision. Careful avoidance of the hair follicles prevents the iatrogenic complication of alopecia. The medial plane of flap elevation is over the temporalis muscular fascia in the loose connective tissue separating the temporoparietal fascia from the muscular fascia.
Once the vascular pedicle has been identified and protected, the elevation can proceed anteriorly to the edge of the hair-bearing scalp, thus protecting the frontal branch of the facial nerve. The posterior margin of the flap should capture the posterior branch of the superficial temporal artery and vein and can be back cut to the vascular pedicle to facilitate flap rotation.
SYSTEMATIC APPROACH TO AURICULAR RECONSTRUCTION BASED ON ANATOMIC LOCATION
Most acquired auricular deformities are partial defects. This section considers the techniques most useful for repairing specific acquired defects of the auricle based upon anatomic location (19).
Preauricular Defects
The most common preauricular defects occur secondary to excision of cutaneous lesions located in this area. The function of the facial nerve should be carefully examined prior to the removal of lesions in this location and monitored intraoperatively. Surgical options for the repair of preauricular defects include preauricular rotation flaps, VY advancement flaps, and simple cheek advancement flaps (Fig. 46.3). With careful planning, the resultant scar can be placed within the preauricular crease with minimal deformity.
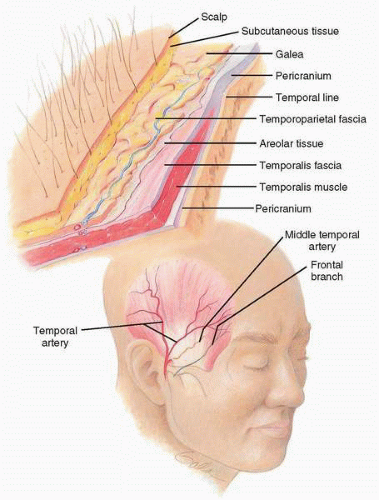 FIG. 46.2 Anatomy of the temporoparietal flap. (From Cheney ML. Facial surgery: plastic and reconstructive. Baltimore: Williams & Wilkins, 1997.) |
Defects of the Conchal Bowl and Root of the Helix
Seen either secondary to cutaneous lesions or after otologic surgery, defects of the conchal bowl or root of the helix can be reconstructed with a helical advancement flap (Fig. 46.4).
In cases in which there is skin loss of the conchal bowl, repair is most successful with skin grafts, as they provides adequate coverage while also allowing for careful monitoring of the area (Fig. 46.5).
Upper Third Defects
Although the upper third of the auricle can be concealed by hair, it is functionally important in the wearing of eyeglasses. Several surgical options are available for the correction of upper third defects; primary closure, helical advancement flaps, and autogenous cartilage framework with temporoparietal fascial coverage. Both primary closure and helical advancement flaps are reserved for smaller, less complicated auricular
defects. The helical advancement flap is preferred over primary closure when the defect is limited to the helix. Primary closure is ordinarily used when the defect extends from the helical rim into the body of the auricle. Reconstruction using a temporoparietal fascial flap with autogenous cartilage framework is indicated in cases where large composite portions of the upper third of the auricle have been removed (Fig. 46.6). Lateral skin defects of the upper and middle third of the auricle can be closed with simple rotation advancement flaps (Fig. 46.7). This technique (20) is preferred over skin grafts or primary closure because skin color is well matched, the alteration of free margins of the upper auricle is not affected, and the incisions are well hidden in the scapha.
defects. The helical advancement flap is preferred over primary closure when the defect is limited to the helix. Primary closure is ordinarily used when the defect extends from the helical rim into the body of the auricle. Reconstruction using a temporoparietal fascial flap with autogenous cartilage framework is indicated in cases where large composite portions of the upper third of the auricle have been removed (Fig. 46.6). Lateral skin defects of the upper and middle third of the auricle can be closed with simple rotation advancement flaps (Fig. 46.7). This technique (20) is preferred over skin grafts or primary closure because skin color is well matched, the alteration of free margins of the upper auricle is not affected, and the incisions are well hidden in the scapha.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree