Thorough evaluation of a patient presenting with nasal obstruction, including nasal endoscopy and a CT scan when indicated, is recommended to guide proper diagnosis and treatment. The rhinoplasty surgeon should be aware of the differential diagnosis of nasal obstruction and should proceed with thorough evaluation or refer the patient for appropriate complete evaluation.
Case report
A 57-year-old white female patient presented for consultation for improvement in her aesthetic nasal appearance and also for evaluation and treatment of nasal obstruction. She had a past history of external septorhinoplasty. She had no allergy symptoms and, in fact, had been tested for environmental allergies by her family doctor by a modified radioallergosorbent test (mRAST) blood test and was negative for significant allergies. She reported bilateral nasal obstruction. She was questioned about other related symptoms; she denied facial pain or pressure, but she did report recurrent sinus infections and postnasal drainage. She denied Afrin use. She did not smoke. She reported persistent nasal obstruction and persistent sinus symptoms despite the use of over-the-counter medications, such as oral decongestants, antihistamines, mucolytics, and saline nasal spray. She also reported no benefit from nasal steroid sprays or other prescription medications.
Physical examination revealed alar retraction and nasal valve collapse. She had middle vault collapse with an inverted V abnormality as well. A modified Cottle maneuver resulted in partial improvement of her nasal obstruction. Anterior rhinoscopy revealed normal inferior turbinates and a left deviated septum. Topical anesthesia with Afrin and Pontocaine was followed by rigid nasal endoscopy. This revealed a leftward deviated septum causing significant nasal obstruction. Superiorly, at the point of maximal deviation, the nasal endoscope could not be passed on the left. The endoscope could be passed along the floor of the nose only on the left. On the right, examination was notable for an enlarged middle turbinate. There were small left unilateral polyps in the middle meatus but no other masses or concerning lesions. The nasopharynx was clear.
A coronal sinus CT scan was obtained ( Fig. 1 ). This revealed the deviated septum, a markedly enlarged and aerated middle turbinate (concha bullosa), and evidence of chronic sinusitis.
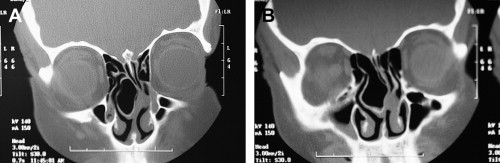
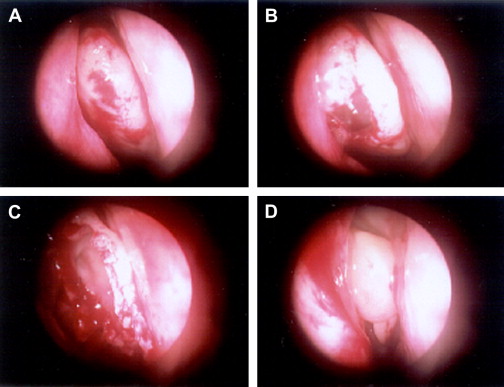
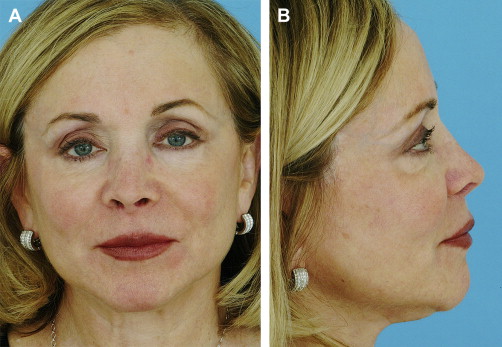
The patient underwent revision external septorhinoplasty, endoscopic sinus surgery, and ear cartilage harvest for cartilage grafting. She underwent bilateral placement of spreader grafts, bilateral alar batten graft placement, and aesthetic corrections as well. At the time of surgery, the surgeon was prepared to undertake endoscopic revision septoplasty if necessary, but it was noted that a thorough septoplasty had been performed. A large portion of the septum was membranous only, without intervening cartilage or bone. On excision of the lateral aspect of the concha bullosa, the deviated septum straightened because it was apparently being held leftward by the large concha bullosa ( Fig. 2 ). After surgery, the patient reported resolution of her nasal obstruction without the need for medical therapy. She was also pleased with her aesthetic appearance 1 year after surgery. Fig. 3 shows the patient preoperatively and Fig. 4 show the patient 1 year postoperatively.

Discussion
Nasal Obstruction Differential Diagnosis
It is important to keep in mind the differential diagnosis of conditions causing nasal obstruction when treating patients with this complaint ( Box 1 ). In the senior author’s rhinoplasty practice, problems causing nasal obstruction have included chronic sinusitis with and without polyps, deviated septum, inferior and middle turbinate hypertrophy, adenoid hypertrophy, tumors, concha bullosa, internal and external valve collapse, and other conditions.
Allergic rhinitis
Rhinosinusitis
Rhinitis medicamentosa
Atrophic rhinitis
Deviated septum
Nasal valve collapse
Nasal polyps
Adenoid hypertrophy
Choanal atresia
Nasal tumors
Inferior turbinate hypertrophy
Middle turbinate hypertrophy
Viral infection (upper respiratory infection)
Septal hematoma
Septal abscess
Nasal foreign body
Overresection or overnarrowing after osteotomies
Nasal Obstruction History and Physical Examination
A detailed history and physical examination, including intranasal examination with and without topicalization with a decongestant and nasal endoscopy, are critical aspects in the evaluation and treatment of every patient presenting with a complaint of nasal obstruction. In patients seeking rhinoplasty, the history should elicit the presence of nasal obstruction, chronic or recurrent sinusitis, postnasal drip and cough, facial pressure or pain, ear pressure or pain, hearing loss, loss of sense of smell or taste, halitosis, and other pertinent findings. A history of prior sinus surgery, rhinoplasty, or other nasal surgery should be noted. The patient should be questioned and, when appropriate, evaluated for allergies.
All medications taken, including aspirin and aspirin-containing products and herbal medicines, such as gingko biloba, that can increase intraoperative bleeding, should be carefully recorded. A history of topical nasal decongestant abuse may lead to the diagnosis and treatment of rhinitis medicamentosa.
External nasal examination is important in all patients with nasal obstruction. Internal and external nasal valve collapse should be recognized when present. A narrow middle third of the nose may be an indication of internal nasal valve compromise. The Cottle maneuver may be helpful in the identification of internal nasal valve collapse. The classic description of this maneuver involves pulling the cheek laterally, resulting in improved nasal breathing. Lateralizing the cheek secondarily moves the nasal soft tissue and widens the nasal valve. A more direct approach is to lateralize the nasal soft tissue gently using a small curette or other straight probe. This must be done before topicalization. Improvement of nasal breathing after minimal (1–2 mm) lateralization of the nasal sidewall suggests that nasal valve abnormality contributes to nasal obstruction. There is the possibility of a false-positive result with this test; thus, the surgeon must be careful to lateralize the nasal sidewall in a realistic manner.
External nasal valve collapse also should be recognized when present. Evidence of prior nasal surgery with excessive reduction and narrowing of the internal and external nasal valve may be immediately evident or it may be subtle.
Intranasal examination should be performed before and after topicalization with a vasoconstricting agent. When indicated by the patient history or by findings on anterior rhinoscopy, a nasal endoscopic examination is also performed. Abnormalities not appreciated on rhinoscopy may be noted on careful endoscopy by a skilled endoscopist in the office after appropriate topicalization and may be of great use in identifying physical findings.
Nasal Obstruction Imaging
In this setting, the physician may also consider obtaining a coronal sinus CT scan, especially in the patient with a history of chronic nasal obstruction. Chronic nasal obstruction is the most common presenting symptom of anterior ethmoid sinus disease. A CT scan may demonstrate evidence of chronic sinusitis, including obstruction of the osteomeatal complex or the presence of polyps, and also of other causes of nasal obstruction, such as concha bullosa or a posterior septal deviation, which may occasionally be unappreciated without an endoscopic examination or CT scan.
Nasal Obstruction Endoscopic Examination
Levine reported that 39% of patients with a complaint of nasal obstruction had findings on endoscopic examination that were not identified with traditional rhinoscopy. Many of Levine’s patients had seen other physicians for this problem and had not received appropriate treatment.
Lanfranchi and colleagues reported on the importance of diagnostic nasal endoscopy in patients with nasal obstruction who present for septorhinoplasty. In their report, a retrospective chart review was undertaken on all patients presenting to the senior author from April 1997 through July 1999 for septorhinoplasty who reported a history of nasal obstruction. Patients seeking cosmetic rhinoplasty without functional complaint were excluded from the study. All patients requesting septorhinoplasty who complained of any degree of nasal obstruction underwent nasal endoscopy. In some cases, a CT scan was additionally undertaken. Findings identified by anterior rhinoscopy were recorded, and additional findings not identified on anterior rhinoscopy were recorded. Ninety-five patients, including 83 undergoing primary rhinoplasty and 12 undergoing revision rhinoplasty, were included in the study.
Nasal examination, including anterior rhinoscopy, revealed obstruction attributable to a deviated septum, nasal valve compromise, and inferior turbinate hypertrophy. Nasal endoscopy revealed additional pathologic findings, including obstructing adenoids, enlarged middle turbinates with concha bullosa, choanal stenosis, nasal polyps, and chronic sinusitis refractory to medical therapy. Additional surgical therapy was undertaken in 28 patients because of findings on endoscopic examination (nine patients underwent partial middle turbinectomy for concha bullosa, 13 underwent endoscopic sinus surgery, two required adenoidectomy, one underwent repair of nasal stenosis, and three required endoscopic septoplasty for persisting posterior septal deviation despite prior septal surgery).
Based on these results, the senior author recommends that patients presenting for septorhinoplasty who note nasal obstruction should undergo anterior rhinoscopy followed by nasal endoscopy. In a significant number of patients (such as the one presented here), nasal endoscopy allows identification of clinically significant pathologic findings and thereby alters surgical therapy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


