Purpose
To correlate the clinical, radiographic, histopathologic, and immunohistochemical features of 5 primary periorbital intraosseous cavernous vascular malformations.
Design
Retrospective interventional case series.
Methods
Clinical and operative records and radiographic images were reviewed. Histopathologic slides were evaluated with hematoxylin-eosin, trichrome, and elastin stains. Immunohistochemical studies were performed with a spectrum of monoclonal antibodies directed at antigens of vascular cells.
Results
Three men and 2 women ranged in age from 36 to 64 years. Vision was unaffected and there was no proptosis or globe displacement. The slow-growing lesions measured 13–25 mm in greatest diameter (mean 16.4 mm). Computed tomographic studies revealed that 2 lesions were situated in the maxillary bone, 2 in the frontal, and 1 in the zygoma, all anteriorly and with circumscribed, lucent, honeycombed, or sunburst characteristics. Histopathologically the lesions were composed of cavernous or telangiectatic channels; 1 showed advanced fibrotic vascular involution. Immunohistochemistry demonstrated CD31/34 positivity for vascular endothelium and D2-40 negativity for lymphatic endothelium. A typically thin mural myofibroblastic cuff was smooth muscle actin positive, weakly calponin positive, and desmin negative. Glucose transporter-1 and Ki-67 were negative in the endothelium.
Conclusions
Intraosseous vascular lesions resemble orbital cavernous venous malformations (not true hemangiomas), except that their vascular walls are thinner owing to the constraints imposed by neighboring bone spicules, which limit the amount of interstitium from which mural myofibroblasts can be recruited. The bony trabeculae conferred the honeycomb or sunburst appearances observed radiographically. En bloc excision of these lesions was successful and avoided complications (mean follow-up, 46 months).
Primary intraosseous vascular lesions account for fewer than 1% of bone “tumors.” They subsume both neoplasms and malformations, and tend to occur preferentially in the vertebral column and calvarium. Over 50 cases of periorbital vascular/bony lesions have been reported. The most commonly affected orbital bones are the frontal and zygoma, followed by the sphenoid and the maxilla. Periorbital intraosseous vascular lesions are typically seen in adults in their fourth and fifth decades of life, although infants and septuagenarians can be affected. In previous reports they have been more frequently encountered in female subjects than in male by a ratio of 3:2. Despite sporadic case reports and 1 series of 5 cases, an in-depth evaluation of a series of periorbital cases with extensive radiographic and immunohistopathologic investigations has not been reported. This study characterizes 5 cases of intraosseous cavernous vascular malformations and their multifaceted features.
Methods
This retrospective study was conducted under the auspices of the Massachusetts Eye and Ear Infirmary Institutional Review Board (project #482489-4) and in compliance with the rules and regulations of the Health Insurance Portability and Accountability Act and in adherence to the Declaration of Helsinki and all relevant federal and state laws. The cases were identified by searching through the records of the David G. Cogan Laboratory of Ophthalmic Pathology at the Massachusetts Eye and Ear Infirmary from 2007 to 2013 for orbital specimens with the diagnoses of intraosseous hemangioma or vascular malformation (5 cases). The clinical records of the physical examination, operative reports, clinical photographs, radiologic imaging studies, and pathologic slides stained with hematoxylin-eosin were reviewed. Archived formalin-fixed, paraffin-embedded tissue blocks were retrieved and 5-μm tissue sections were obtained for additional staining.
Special stains for Trichrome Blue II (a modified version of the Masson trichrome stain; Ventana Medical Systems, Tucson, Arizona, USA) and Verhoeff-Van Gieson for elastin (Ventana Medical Systems) were processed on a NexES special stainer (Ventana Medical Systems) at Integrated Oncology (New York, New York, USA). Immunohistochemical (IHC) stains for CD31, CD34, D2-40, glucose transporter-1, smooth muscle actin, desmin, calponin, and Ki-67 ( Table 1 ) were processed on a Leica Bond III autostainer (Leica Biosystems, Melbourne, Australia) in the Diagnostic Immunopathology Laboratory of the Department of Pathology at the Massachusetts General Hospital (Boston, Massachusetts, USA). The stains were developed with the immunoperoxidase technique using the chromogen diaminobenzidine. The tissues were counterstained with hematoxylin. Appropriate controls were included to validate antibody quality. The tissue slides were visualized using light microscopy.
| Marker | Molecular Properties | Cell/Tissue/Tumor Specificity | Staining Pattern | Source |
|---|---|---|---|---|
| CD31 | Platelet endothelial cell adhesion molecule-1 (PECAM-1), a 130-kDa glycoprotein | Vascular endothelium | Cell membrane and cytoplasm | Mouse monoclonal (Dako, Carpinteria, California, USA) |
| CD34 | Transmembrane sialomucin protein, a 110-kDa glycoprotein | Vascular and lymphatic endothelium, early hematopoietic tissue | Cell membrane and cytoplasm | Mouse monoclonal (Leica Biosystems, Newcastle Upon Tyne, UK) |
| D2-40 | Podoplanin, O-linked transmembrane sialoglycoprotein, 38-kDa | Lymphatic endothelium, fetal testis | Cell membrane and cytoplasm | Mouse monoclonal (Dako, Carpinteria, California, USA) |
| Glut-1 | Glucose transporter-1, 45 or 55 kDa depending on the extent of glycosylation | Widely distributed in fetal tissues; in adults found in erythrocytes, endothelial cells of the blood-brain barrier, and actively proliferating endothelium | Cell membrane and cytoplasm | Rabbit Polyclonal (Thermo Fisher Scientific, Fremont, California, USA) |
| Smooth muscle actin | Alpha-smooth muscle isoform of contractile actin | Smooth muscle cells in blood vessels, gut wall, and myometrium; smooth muscle, myoepithelium; myofibroblasts | Cytoplasm | Mouse monoclonal (Biocare Medical, Concord, California, USA) |
| Desmin | Muscle-specific type III intermediate filament, 53 kDa, for anchoring contractile filaments | Cardiac muscle, skeletal muscle, smooth muscle, desmoplastic small round cell tumor; absent in myofibroblasts | Cytoplasm | Mouse monoclonal (Leica Biosystems, Newcastle Upon Tyne, UK) |
| Calponin | A calcium-binding protein, 34 kDa, regulating smooth muscle contraction | Smooth muscle cells, myoepithelium and myofibroblasts | Cytoplasm | Mouse monoclonal (Dako, Carpinteria, California, USA) |
| Ki-67 | Antigen Ki-67, a large nuclear protein, two isoforms of 345 and 395 kDa, associated with cellular proliferation | Cells in all active phases of the cell cycle (G 1 , S, G 2 , and M-phases), absent in resting cells (G 0 -phase) | Nucleus | Mouse monoclonal (Dako, Carpinteria, California, USA) |
Results
Clinical Findings
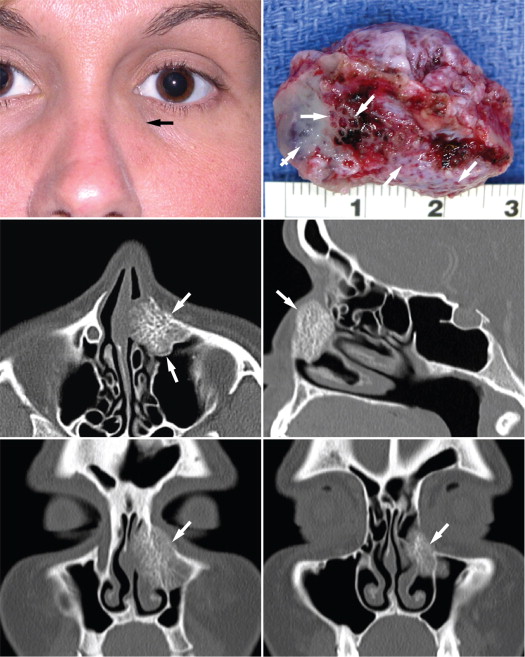
The clinical features of the 5 cases in this study are summarized in Table 2 . There were 2 female and 3 male patients. Their ages at presentation ranged from 36 to 64 years (mean of 51 years). They were either asymptomatic or were exhibiting only mild symptoms. Four patients presented with a slowly growing periorbital mass ( Figure 1 , Top left and Top right). Three complained of mild intermittent pain, and 2 had epiphora. The mean duration of symptoms was 22 months (range of 2 months to 6 years and median of 7 months). One patient who was asymptomatic had a lucent intraosseous lesion, which was incidentally found on a computed tomographic (CT) scan that was performed for unrelated medical reasons. Four of the 5 patients had no history of prior trauma to the involved periorbital area. Patient 3 had suffered a nondisplaced complex zygomatic facial fracture 5 years prior to presentation. A CT scan performed at that time also revealed an expansion of the right zygomatic bone suggestive of fibrous dysplasia. On physical examination, the masses were generally firm and fixed, with a slightly irregular surface and occasional mild tenderness to palpation. The remainder of the ophthalmic examinations were unremarkable. All patients underwent local surgical excision, either for cosmetic reasons or to obtain a definitive pathologic diagnosis. En bloc resection was successful in all cases. Intraoperative blood loss was recorded as “minimal” in 3 cases, and no patient lost more than 30 mL. Bone wax was not required to achieve hemostasis. No recurrence has been reported after an average follow-up of 46.2 months, ranging from 21 to 85 months.
| Patient# | Age/Sex | Side | Visual Acuity | Symptoms/Duration | Other Relevant Features | Radiologic Location | Radiologic Features | Treatment | Blood Loss | Follow-up/Recurrence |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 36/F | L | 20/20 | Mass, pain, epiphora; 6 y | None | Frontal process of the maxillary bone | “Honeycomb” or “sunburst” pattern | Complete excision | 20–30 mL | 45 mo/none |
| 2 | 59/F | L | 20/25 | Mass, pain, epiphora; 6 mo | None | Frontal process of the maxillary bone | Nodular mass with internal calcification | Complete excision | <5 mL | 53 mo/none |
| 3 | 64/M | R | 20/20 | Mass, pain; 8 mo | Prior injury, fibrous dysplasia | Zygomatic body | “Honeycomb” pattern | Complete excision | Minimal | 85 mo/none |
| 4 | 50/M | R | 20/20 | No symptoms | None | Frontal bone, just superior to the frontozygomatic suture | Lucent lesion with 1 small focus of internal calcification | Complete excision | Minimal | 21 mo/none |
| 5 | 45/M | R | 20/25 | Mass; 2 mo | Fibrous dysplasia | Frontal bone, just superior to the frontozygomatic suture | Slightly lucent lesion with detectable bony spicules | Complete excision | <25 mL | 27 mo/none |
Radiographic Findings
CT scanning was performed with contrast in 4 cases and without contrast in 1. Two lesions were located at the frontal process of the maxillary bone. In Patient 1 ( Figure 1 , Top left and Top right), a contrast-enhanced CT orbital scan revealed an expansile bony lesion, measuring 25 × 22 × 20 mm, centered in the nasal process of the left maxilla ( Figure 1 , Middle left and Middle right, Bottom left and Bottom right). It extended laterally into the maxillary sinus, posteriorly into the nasolacrimal duct, superiorly into the lower orbit, and inferiorly into the inferior meatus. It had a classic “honeycomb” and “sunburst” pattern of radiating trabeculae with speckled calcifications in a hypodense lesion. Clinically, the patient complained of epiphora with an increased tear lake on the affected side (8 mm on the left vs 3 mm on the right). Lacrimal irrigation through the inferior canaliculus revealed 10% flow and 90% reflux through the superior canaliculus. Nasal endoscopy disclosed a left submucosal yellow round mass in the middle meatus extending from the lateral nasal wall in the anterior portion of the nose. Based on clinical presentation and radiographic features, this lesion was thought most likely to represent an intraosseous vascular lesion.
In Patient 2 ( Figure 2 , Top left and Top right), CT scanning of the orbit with contrast revealed a nodular soft tissue mass with internal calcifications, measuring 12 × 11 × 10 mm. Its medial aspect abutted the frontal process of the maxilla and the upper nasolacrimal duct; its inferior aspect approached the medial aspect of the orbital floor. There was some suggestion of mottling or erosion of the underlying bone. Despite the close proximity to the nasolacrimal duct, lacrimal irrigation showed 100% patency, indicating that the mass was extrinsic to the lacrimal sac. The lesion in Patient 3 arose from the frontal process of the zygoma, just inferior to the frontozygomatic suture ( Figure 2 , Middle left and Middle right). CT scanning with contrast demonstrated a 17-mm oval-to-round expansile lesion involving the right zygoma that extended to the lateral wall of the right orbit. The lesion had a trabeculated “honeycomb” appearance and was associated with a spiculated periosteal reaction laterally. An intraosseous vascular lesion was diagnosed.
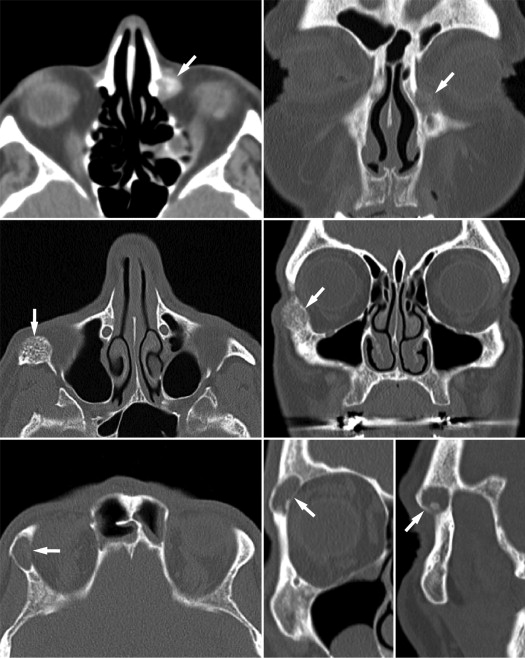
The last 2 lesions were discovered in the frontal bone, just superior to the frontozygomatic suture. In Patient 4, a CT scan without contrast disclosed an incidental finding of a well-circumscribed lucent lesion in the frontal bone, measuring 15 × 15 × 8 mm ( Figure 2 , Bottom left and Bottom right). It had no diffuse bony matrix but only 1 small focus of internal calcification. A partial arc of sclerotic bone was seen along the anteroinferior border. In Patient 5, contrast-enhanced CT scan demonstrated a small, poorly delineated, subtle bony anomaly that arose from the frontal bone and measured 13 mm in greatest dimension. The lesion appeared similar to the surrounding normal bone, consisting of outer cortex and inner marrow with faintly discernible bony spicules, but had slightly less overall density than the surrounding bone, which conferred a cystic or lytic appearance. The area was mildly expanded compared to the contralateral frontal bone. The posterior margin of the lesion was slightly elevated and deformed the bony cortex of the normal bony outline. In addition, a small incidental lucent lesion with ground-glass appearance was identified in the left nasal bone, consistent with fibrous dysplasia.
Histopathologic and Immunohistochemical Findings
The lesions measured 13–25 mm in greatest dimension and grossly consisted of oval-to-round friable masses with streaks of white bone interspersed with speckled red foci representing the vascular spaces ( Figure 1 , Top right). Paraffin sections stained with hematoxylin-eosin disclosed variably thick and thin, and often interconnecting, bony trabeculae enclosing large (“cavernous”) vascular spaces ( Figure 3 , Top left). For the most part, the trabeculae did not exhibit either osteoclastic or osteoblastic activity. In 3 lesions the circumscribed border was incompletely formed by fibrous tissue ( Figure 3 , Top left inset), in 2 by a partial thin or thick bony perimeter ( Figure 3 , Top right), and 1 was focally delimited by sinus mucous and associated submucosal glands on which the tumor abutted ( Figure 3 , Middle left and inset).
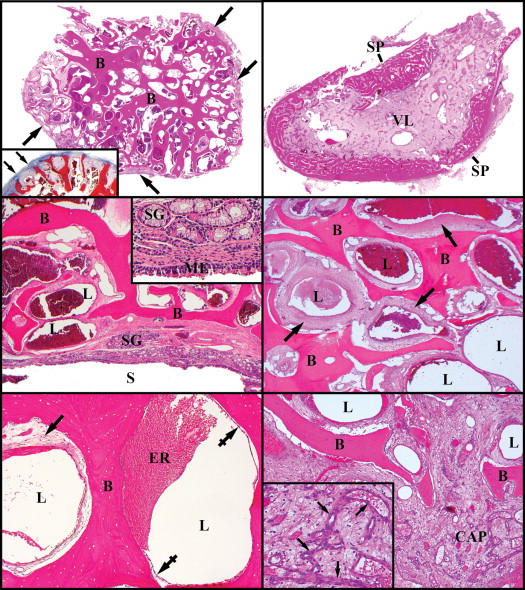
Four of the 5 lesions were composed of cavernous vascular channels that appeared completely viable ( Figure 3 , Middle right). They did not contain any phleboliths or thrombi in their lumens. Telangiectatic vessels with a negligible wall ( Figure 3 , Bottom left) were prominent in 2 of the lesions. In these instances the endothelial cells often rested directly upon the bony trabeculae without the interposition of any mural cells or stroma. When there was a conspicuous vascular wall, the trichrome stain demonstrated moderate reddish (fuchsinophilic) staining of the cytoplasm of the constituent spindle cells, suggesting myoid differentiation.
The Verhoeff-van Gieson stain failed to identify an elastic lamina. Free bundles of smooth muscle cells in the interstitium were not observed. Smaller capillary-size vessels ( Figure 3 , Bottom right and inset) were discovered focally in the interstitium and sometimes appeared to anastomose with the cavernous channels. One lesion (Case 4) manifested signs of advanced involution ( Figure 4 , Top left and inset). This was the mass that radiographically ( Figure 2 , Bottom left and Bottom right) and histopathologically manifested an outer sclerotic rim ( Figure 3 , Top right). Erythrocytes were only occasionally found in the cavernous lumens of this lesion; the vascular walls were sclerotic and devoid of cells ( Figure 4 , Top left). The lumens were frequently obliterated by loose fibrous tissue; and the stroma almost completely lacked cells, as well as bony trabeculae. Within this stroma there were sclerotic, smaller-caliber vessels as well. The trichrome strikingly accentuated the dense collagenous vascular walls ( Figure 4 , Top left inset). In the hyperostotic margin, patent vessels were found between the thickened trabeculae.
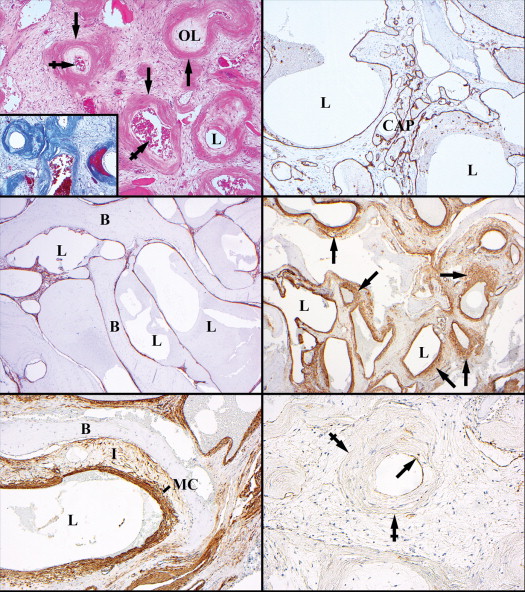
Immunohistochemical studies established that endothelial cells of the cavernous channels and the smaller interstitial capillary-type vessels were both CD31 and CD34 positive ( Figure 4 , Top right) but glucose transporter-1 negative. D2-40 for lymphatic endothelium was negative in all types of vessels. Smooth muscle actin immunostained only the endothelial cells of the telangiectatic spaces that were applied against the bony trabeculae ( Figure 4 , Middle left). When there was more interstitium between the trabeculae, the cavernous spaces progressively acquired thicker mantles of smooth muscle–like, actin-positive mural cells ( Figure 4 , Middle right). Only rarely were actin-positive stromal cells (myofibroblasts) detected away from the vessels ( Figure 4 , Bottom left). The small interstitial capillary vessels also reacted positively for smooth muscle actin. Smooth muscle actin variably immunostained some of the endothelial cells of the involuting lesion; CD31 could also be identified only in trace amounts in scattered endothelial cells ( Figure 4 , Bottom right). No mural cells stained for smooth muscle actin. Calponin but not desmin was found in focal mural cells and scattered cells in the interstitium of the 4 viable lesions, whereas it was absent in the involuting lesion. Ki-67 was not detected in the nuclei of any of the endothelial cells in the viable cavernous channels or in the interstitial capillary proliferations.
Results
Clinical Findings
The clinical features of the 5 cases in this study are summarized in Table 2 . There were 2 female and 3 male patients. Their ages at presentation ranged from 36 to 64 years (mean of 51 years). They were either asymptomatic or were exhibiting only mild symptoms. Four patients presented with a slowly growing periorbital mass ( Figure 1 , Top left and Top right). Three complained of mild intermittent pain, and 2 had epiphora. The mean duration of symptoms was 22 months (range of 2 months to 6 years and median of 7 months). One patient who was asymptomatic had a lucent intraosseous lesion, which was incidentally found on a computed tomographic (CT) scan that was performed for unrelated medical reasons. Four of the 5 patients had no history of prior trauma to the involved periorbital area. Patient 3 had suffered a nondisplaced complex zygomatic facial fracture 5 years prior to presentation. A CT scan performed at that time also revealed an expansion of the right zygomatic bone suggestive of fibrous dysplasia. On physical examination, the masses were generally firm and fixed, with a slightly irregular surface and occasional mild tenderness to palpation. The remainder of the ophthalmic examinations were unremarkable. All patients underwent local surgical excision, either for cosmetic reasons or to obtain a definitive pathologic diagnosis. En bloc resection was successful in all cases. Intraoperative blood loss was recorded as “minimal” in 3 cases, and no patient lost more than 30 mL. Bone wax was not required to achieve hemostasis. No recurrence has been reported after an average follow-up of 46.2 months, ranging from 21 to 85 months.



