β-Adrenergic Receptor Antagonists
The adrenergic receptors are an important physiologic target, and within the eye these receptors have a major role in regulating aqueous humor dynamics (see Chapter 1). After the development of systemic β-adrenergic receptor antagonists, commonly called β-blockers, for cardiovascular applications, topical formulations of β-blockers were later developed for lowering intraocular pressure (IOP) in the treatment of glaucoma. The first commercially available β-blocker was propranolol, which was introduced in 1967 for the treatment of cardiac arrhythmias, angina pectoris, and systemic hypertension. This drug was found to reduce IOP when given orally, topically, or intravenously (1–3). Many of these compounds, however, caused adverse reactions, such as corneal anesthesia due to membrane-stabilizing activity, dry eye–related problems, subconjunctival fibrosis, corneal ulcers, and rash (2,4). With further development and research, several compounds in the β-blocker class of drugs were identified without these adverse reactions and were introduced into clinical use. α-Adrenergic receptor antagonists have also been developed, but this class of drugs appears to have minimal effects on aqueous humor dynamics and is not used in the long-term treatment of glaucoma.
β-ADRENERGIC RECEPTOR ANTAGONISTS
Mechanisms of Action
Aqueous humor flow is the main mechanism by which the β-blockers lower the IOP. Timolol has been shown to have its main IOP-lowering effect by reducing aqueous humor production based on studies using tonographic and fluorophotometric methods (5). The β-adrenergic receptors, predominantly of the β2 subtype, have been identified in ciliary processes (6–9). The influence of timolol on aqueous humor formation may be related to inhibition of catecholamine-stimulated synthesis of cyclic adenosine monophosphate (AMP), which has been demonstrated in rabbit studies (10,11).
The mechanism by which an adrenergic antagonist reduces aqueous production relates to the physiology of the sympathetic system in the ciliary processes and on aqueous humor dynamics (see Chapter 1). In patients with sympathetic denervation from postganglionic Horner syndrome, neither aqueous humor flow nor IOP is affected (12). The possibility that tone could arise from circulating catecholamines was not supported by the observation that patients with bilateral adrenalectomies do not influence the circadian rhythm of aqueous flow nor the daytime effect of timolol on the flow (13). Another interesting observation is that timolol does not appear to be effective in sleeping human participants during which time the aqueous flow is normally less than half the daytime flow rate (14). However, timolol does lower aqueous flow at night in humans receiving systemic epinephrine (15). Based on these clinical observations in certain diseases known to affect the sympathetic nervous system and normal physiologic conditions, the precise mechanisms by which the sympathetic system regulates aqueous humor dynamics is complex and not fully understood (see Chapter 1).
Overall, the outflow facility does not appear to be influenced by timolol (16,17). However, topical timolol was associated with a small myopic shift in one human study, suggesting that sympathetic innervation is involved in the resting tone of the ciliary muscle (18). Furthermore, the β-adrenergic receptors, primarily of the β2 subtype, have been demonstrated in human trabecular meshwork (19,20). A histologic study of the outflow apparatus in human eyes treated with timolol before enucleation for malignant melanoma revealed no morphologic changes suggestive of a pressure-lowering action by the drug (21). However, the trabecular meshwork in primates after long-term timolol therapy revealed degeneration of the trabecular cells, partial destruction of the beams, rarefaction of the meshwork, and disconnection of the trabecular lamellae from the ciliary muscle fibers (22).
The possible effect of β-blockers on ocular blood flow is complex and involves consideration of the various vascular beds, including the ciliary, retinal, choroidal, and retrobulbar vessels located within their respective tissues (23). There are conflicting effects of the topical β-blockers on ciliary systolic perfusion pressure (24). Carteolol and levobunolol were shown to increase ocular pulsatile blood flow (25,26). Another study showed that carteolol, compared with a placebo, had no significant effect on human retinal circulation with regard to changes in vessel diameter, maximum erythrocyte velocity, and volumetric blood flow rate (27). In a study of patients with normal-tension glaucoma, color Doppler imaging of orbital vessels showed an increase in end-diastolic velocity and a decrease in resistance index with betaxolol, but not with timolol (28). However, when the two drugs were evaluated in rabbits with an intraluminal microvascular corrosion casting technique, neither produced an observable vasomotor effect (29). With regard to ocular blood flow, levobunolol, betaxolol, and carteolol did not influence perimacular hemodynamics as determined by blue field entoptic simulation in normal volunteers, which the investigators thought suggested normal autoregulation (30). Whether β-blockers clinically influence ocular blood flow and whether there is a significant difference between nonselective and cardioselective agents is unclear.
Other possible mechanisms for the effect of timolol on lowering IOP have been examined. It does not appear that timolol significantly influences the blood–aqueous barrier. Simultaneous bilateral fluorescein angiography of the iris revealed no effect of timolol on dye leakage (31). It also appears that the timolol mechanism is not prostaglandin mediated, because it is not altered by concurrent therapy with indomethacin or flurbiprofen (32,33). In a study with rabbit eyes, there was a suggestion that timolol might act as a dopaminergic antagonist to lower blood flow to the ciliary body (34). However, metoclopramide, a dopamine-2 antagonist, did not affect the ocular hypotensive action of timolol in healthy volunteers (35).
Specific Agents
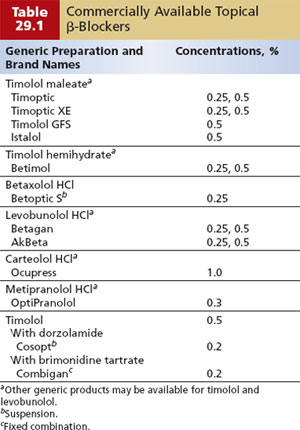
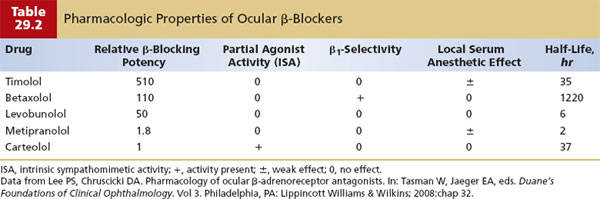
The first topical β-blocker available as a topical agent for the treatment of glaucoma was timolol (Fig. 29.1). (The commercially available β-blockers are discussed in the following text and summarized in Table 29.1.) Other β-blockers were subsequently developed, and in general, although comparable with timolol, they vary according to relative β-blocking potency, selectivity for specific β-receptor, and other characteristics (Table 29.2) (36).
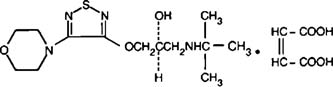
Figure 29.1 Chemical structure of timolol.
Timolol
Timolol is a nonselective, β1– and β2-adrenergic antagonist, which is produced by using various formulations. Timolol was found to lack the adverse effects related to corneal anesthesia and subconjunctival fibrosis compared with the earlier β-blockers (37). Rabbit studies revealed an IOP-lowering effect in both the treated and the fellow untreated eye (38,39). Primate studies have demonstrated a topical timolol effect on aqueous flow in the fellow, untreated eye, the degree of which is dose related (40). The contralateral effect of β-blockers has also been shown in patients with open-angle glaucoma and patients with ocular hypertension (41,42). The observation of the contralateral IOP lowering in the fellow untreated eye suggests that the drug is absorbed and exerts its effect through the systemic circulation (see “Side Effects”).
Single doses of timolol in normotensive individuals and in patients with chronic open-angle glaucoma (COAG) lowered the IOP (42,43). Short-term, multiple-dose trials with patients with open-angle glaucoma demonstrated a sustained reduction in the IOP (44–47).
Comparative studies have shown the IOP-lowering efficacy of timolol to be greater than that of epinephrine (45,48) and equal to or slightly weaker than various concentrations of combined epinephrine and guanethidine (49). Compared with pilocarpine, timolol had an equivalent or slightly greater IOP-lowering effect (50–53). In a comparative study of timolol twice daily compared with pilocarpine four times daily, more patients receiving pilocarpine discontinued the study because of inadequate IOP control, and patients receiving pilocarpine had significantly greater visual field deterioration (54). In another comparative study, echothiophate iodide was more effective than timolol in the treatment of glaucoma in eyes with aphakia (55).
With the availability of timolol in the gel-forming solution, several clinical studies have shown equivalence in IOP lowering for timolol gel dosed once daily and timolol solution dosed twice daily (56,57). Similar studies comparing once-daily dosing of timolol gel and timolol solution have not been reported. This issue of designing clinical studies to compare the efficacy of β-blockers is clinically relevant, because once-daily instillation of levobunolol provided similar IOP control to twice-daily use of the same drug (58,59), which is discussed later.
Betaxolol
Unlike timolol and the other β-blockers, betaxolol hydrochloride is a cardioselective, β1-adrenergic antagonist. It is currently available as a 0.25% suspension formulation. Although this drug is more selective on the β1-receptors, receptor occupancy studies of human aqueous from betaxolol-treated eyes suggest a role of β2-receptor blockade (60). The mechanism of ocular hypotension appears to be the same as that for timolol, with reduction of aqueous humor production and no effect on outflow resistance or pupillary diameter (61).
When compared with timolol at 0.25% and 0.5% doses, the magnitude of IOP reduction in most studies is slightly less with betaxolol, and there may be a greater need for adjunctive therapy than with timolol (62,63). In one study of 153 glaucoma patients whose IOPs were controlled on timolol, the 50% of patients who were switched to betaxolol in a masked and random fashion had a significant increase in IOP (64). However, when betaxolol, 0.5%, and timolol, 0.5%, both given twice daily, were compared in long-term, parallel trials of 18 to 30 months in patients with open-angle glaucoma, the timolol group had better IOP levels, but the betaxolol group had a more favorable course regarding retinal sensitivity as measured by static automated perimetry (65,66). (The possible explanation for this is discussed later.)
Several clinical studies have also compared the IOP-lowering efficacy of betaxolol and α-adrenergic agonists. In a 3-month comparative trial of betaxolol, 0.5%, and dipivefrin, 0.1%, IOP reductions were similar, with mean decreases of 4.1 and 3.5 mm Hg, respectively (67). In a 4-month masked, randomized trial comparing twice-daily treatment with betaxolol, 0.25%, or brimonidine, 0.2%, in 188 patients with glaucoma or ocular hypertension, IOP reductions measured near the peak effect of these drugs showed mean decreases of 5.9 mm Hg for brimonidine and 3.8 mm Hg for betaxolol (68).
Levobunolol
Levobunolol (1-bunolol), an analog of propranolol, is another nonselective β1– and β2-adrenergic antagonist. In short-term studies, the onset of an ocular hypotensive effect occurred within the first hour after instillation, peaked at 3 hours, and lasted up to 24 hours (69). In commercial bottles, a drop of the original levobunolol is significantly larger than that of timolol, which results from the dispensing system and the increased viscosity of levobunolol (70). However, the drop size does not appear to influence the efficacy or safety of the drug (71). Levobunolol is effective with once-daily administration in a high percentage of patients (72), with once-daily instillation of the 0.5% concentration providing similar IOP control to twice-daily use of the same drug and the 0.25% concentration given once daily providing adequate control in many cases (58).
In comparative short-term and long-term clinical studies, levobunolol in various concentrations was equivalent to timolol with regard to ocular hypotensive efficacy and side effects when the two drugs were administered twice daily (73,74). It was also shown to be equivalent to the nonselective β-blocker metipranolol (75) but had significantly greater pressure-lowering efficacy than betaxolol in a 3-month study (76). It has also been shown to provide additional IOP reduction when added to dipivefrin, with efficacy and safety comparable with concomitant timolol and dipivefrin therapy (77).
Carteolol
Carteolol is a nonselective β-adrenergic antagonist with intrinsic sympathomimetic activity. The latter feature produces an early, transient adrenergic agonist response that is not found in the other topical β-blockers. Studies with systemic β-blockers indicate that intrinsic sympathomimetic activity does not interfere with the therapeutic benefits of β-blockers (78). In most studies comparing carteolol and timolol, there was no significant difference in the effects on pulse or blood pressure (79,80). Although the intrinsic sympathomimetic activity of carteolol does not appear to protect against cardiovascular effects such as reduced pulse and blood pressure, there is evidence that it may decrease the cardiovascular risks associated with cholesterol abnormalities. A comparative trial of carteolol, 1%, and timolol, 0.5%, in 58 healthy, normolipidemic adult men confirmed the earlier findings with regard to timolol and showed significantly less effect of carteolol on high-density lipoprotein (HDL) cholesterol (81). Carteolol therapy was associated with a 3.3% decrease in HDL level and a 4% increase in total cholesterol–HDL ratio, compared with 8% and 10%, respectively, with timolol. Although the implications of these findings are not clear for glaucoma populations, it underscores the importance of recommending nasolacrimal occlusion to minimize systemic absorption of topical β-blockers.
In a vehicle-controlled trial, carteolol, 1%, and carteolol, 2%, produced mean IOP reductions of 23% and 26%, respectively (82). When compared with timolol, the ocular hypotensive efficacy and duration of action were comparable in most studies (79,80). Carteolol has been shown, however, to cause less ocular irritation than timolol in the first few minutes after instillation (79). Carteolol has also been studied as a fixed combination with pilocarpine. Various combinations of carteolol, 1% and 2%, with pilocarpine, 2% and 4%, and of timolol, 0.5%, with pilocarpine, 2% and 4%, gave mean IOP reductions of 24% to 40% (82,83). However, carteolol or timolol in combination with pilocarpine was slightly less effective than when the two drugs were given separately (83).
Metipranolol
Metipranolol is a nonselective β-blocker that has been shown in a placebo-controlled trial to significantly lower the IOP by reducing the rate of aqueous flow with no effect on outflow (84). Comparative studies have shown that it is comparable with timolol and levobunolol with regard to efficacy and safety. Metipranolol is commercially available in a 0.3% concentration (85) (Table 29.1).
D-Timolol
Previous reference to timolol in this chapter has been to l-timolol, or the (S)-enantiomer, which is the stereoisomer form of the drug currently used in the treatment of glaucoma. The d-timolol, the (R)-enantiomer, is a significantly less potent β-adrenergic antagonist with regard to both IOP reduction and systemic effects (86,87).
Atenolol
Atenolol is a selective β1-adrenergic antagonist with no intrinsic sympathomimetic or membrane-stabilizing properties (88). Oral atenolol, 25 to 100 mg, provided significant IOP reduction when compared with a placebo (89). Topical administration of atenolol, 2%, was similar to pilocarpine, 2% (90), and atenolol, 4%, was more effective than epinephrine, 1% (91). However, a long-term study showed that the initial pressure control gradually wore off in some patients (92).
Metoprolol
Metoprolol is a cardioselective β1-adrenergic antagonist that, like betaxolol, has reduced IOP without the adverse respiratory side effects of the nonselective β-blockers (93). Prolonged ocular hypotensive action has been demonstrated with both oral administration of 100-mg tablets or topical instillation of metoprolol, 1% to 5% (93,94). Metoprolol, 3%, was similar to pilocarpine, 2% to 4%, in lowering IOP in one study and had roughly the equivalent ocular hypotensive effect to that of timolol in another evaluation (95,96).
Pindolol
Pindolol is a potent β-adrenergic antagonist with an intrinsic sympathomimetic effect and is reported to provide a good ocular hypotensive effect (97). Pindolol, 0.5% to 1%, has been shown to provide prolonged IOP reduction without significant ocular or systemic side effects (98), although reports are conflicting regarding the influence of pindolol on corneal anesthesia (97).
Nadolol
Oral administration of nadolol, a nonselective β-blocker, 10 to 80 mg daily, has been shown to cause a significant, dose-related reduction in IOP (99). Topical preparations also produce a significant dose-dependent IOP reduction, which lasts more than 9 hours with the higher concentrations of 1% to 2%, but this effect was not maintained with continued use (100). To overcome the issue of poor corneal penetration, the prodrug analog of nadolol, diacetyl nadolol, was developed and found to be as effective as timolol in lowering the IOP up to 8 hours with less efficacy thereafter (101). However, diacetyl nadolol, 2%, had a lower incidence of tolerance than did timolol, 0.5%, in a 3-month study (102).
Befunolol
Befunolol, 0.25% and 0.5%, provided good IOP reduction in a 3-month study (103), with no significant diminution of effect during 1-year follow-up (104). In a preliminary study, changing from timolol, 0.5%, to befunolol, 0.5%, was associated with a significant additional decrease in IOP (105).
Administration
Concentrations
Commercially available β-blockers are formulated in various concentrations (Table 29.1). Early experience with patients with COAG indicated that the maximum IOP-lowering effect of timolol maleate is achieved with the 0.5% concentration (37,43). In other studies, however, the 0.25% concentration was equally or more efficacious than the 0.5%, although the latter provided a somewhat longer duration of action (106,107). Dose–response studies of aqueous humor formation in primates showed that a dose of timolol as small as 2.5 µg can suppress aqueous flow by a 20%, suggesting that standard clinical doses may be greater than necessary (108). Nevertheless, individuals with darker irides appear to require higher concentrations of timolol (109). In one study, timolol had a significant ocular hypotensive effect 1 hour after instillation in patients with blue irides but no effect in brown-eyed patients, which probably relates to nonspecific binding of the drug to pigment (110).
Frequency
Good corneal penetration of timolol has been demonstrated in rabbit and human eyes, with peak aqueous humor concentrations in human eyes occurring within 1 to 2 hours (111,112). The IOP-lowering effect peaks approximately 2 hours after administration and lasts for at least 24 hours (37,43,113). The optimum frequency of administration in most cases is twice daily, although once-a-day treatment has been shown to be adequate in many cases (114,115). One study found no significant difference whether timolol, 0.5%, was given in the morning or evening (116). Timolol in a gel vehicle was found to elicit a 1 to 2 mm Hg greater efficacy than the solution during 24 hours after instillation (117). When timolol use is discontinued after long-term therapy, aqueous humor flow does not increase significantly until the fourth day, and the IOP effect may still be seen 14 days later (118). This may reflect the concentration of the drug in melanotic tissues and the slow release. In rabbits receiving topical timolol for 42 days, the drug was still present in pigmented ocular tissues 42 days after withdrawal of the drug (119).
Long-Term Efficacy
Numerous long-term studies have confirmed the continued efficacy of long-term timolol therapy for many patients (120–126). In a significant number of cases, however, the pressure responsiveness to timolol will decrease with continued administration. This occurs in two phases, which Boger (127) called short-term escape and long-term drift.
Short-Term Escape
Many patients will experience a dramatic reduction in IOP with the initiation of timolol therapy. However, the pressure usually rises during the next few days and plateaus at a maintenance level (50,128–130). The 1-hour IOP response to timolol does not predict which patients will have a significant loss of responsiveness 3 to 4 weeks later (130). It has been demonstrated that the number of β-receptors in ocular tissues increases during the first few days of timolol therapy (131), which may explain this escape phenomenon. In any case, it is good clinical practice to wait approximately 1 month after initiating timolol to determine the efficacy of therapy.
Long-Term Drift
When the IOP levels off after the initiation of timolol therapy, control can be maintained in most cases. Some patients, however, have a slow decline in pressure response to timolol, usually beginning 3 months to 1 year after starting treatment (120–126,132,133). Fluorophotometric studies indicate that aqueous humor flow is higher in most patients after 1 year of timolol therapy compared with the value 1 week after initiating treatment (134). Some patients regain responsiveness to timolol after a washout period. In one study of 39 eyes showing a long-term drift with timolol, 0.5%, 23 eyes received dipivefrin (a prodrug of epinephrine) during a 30- or 60-day timolol holiday, and the remainder received artificial tears in place of the timolol (135). When the timolol was reinstituted, the dipivefrin-treated group had a mean IOP decrease of 8.2 mm Hg, compared with 3.9 in the non–dipivefrin-treated group, and the response to timolol was more prolonged in eyes treated for 60 days with dipivefrin. Based on this observation, a treatment strategy of pulsatile therapy, in which timolol, 0.5%, is given for 6 months and then alternates with dipivefrin for 2 months, was studied and shown to minimize long-term drift, compared with continuous use of timolol (136).
Drug Interactions and Multiple-Agent Formulations
Numerous clinical studies have been conducted to examine the effect of combining topical β-blockers, primarily with timolol, 0.5%, with other antiglaucoma therapy. However, when instituting fixed-combination versus multiple-drug therapy, the possibility of changes in ocular and systemic drug absorption, adherence, and cost of the therapy must be considered (137,138).
There are two commercially available forms of fixed combination drugs formulated with timolol, 0.5% (138). The combination of brimonidine tartrate, 0.2%, with timolol, 0.5% (Combigan), was developed because of the efficacy of IOP lowering with the individual components of the α2-adrenergic agonist brimonidine and timolol, 0.5% (139) (see Chapter 30). The other fixed combination is dorzolamide, 2.0%, with timolol, 0.5% (Cosopt; also available in generic formulation) (140). However, in general, there is greater efficacy in IOP lowering when combining timolol with the oral carbonic anhydrase inhibitors (CAIs) (141–143), compared with topical CAIs (see Chapter 31). (The interaction between timolol and the prostaglandin agents is discussed in Chapter 28.)
For timolol, the combined effect of timolol and a miotic is, for most patients, significantly greater than the effect of either medication alone (141,144–146). Although no longer available in the United States, a combined formulation of timolol, 0.5%, and pilocarpine, 2% to 4% (TP2 and TP4), administered twice daily, provides IOP reduction similar to timolol and pilocarpine when given separately (147).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


