17
25-Gauge Vitrectomy for Macular Surgery
Steve Charles
Sutureless, 25-gauge (25G) vitrectomy was initially utilized by most surgeons for epimacular membranes, macular holes, and vitreomacular traction syndromes, as well as for procedures now shown to be ineffective: branch vein decompression and radial optic neurotomy. Virtually all techniques utilized for 20-gauge (20G) vitrectomy can be utilized with 25G vitrectomy (1–18) using new tools and technique modifications discussed in this chapter. Some techniques to be discussed are applicable to 25G surgery and selected 23-gauge (23G) and 20G procedures as well.
ADVANTAGES OF 25G VITRECTOMY
There are many advantages to eliminating both scleral and conjunctival sutures, including reduced discomfort, photophobia, tearing, squeezing, conjunctival hyperemia, and bleeding. Faster visual recovery occurs because astigmatism from the sclerotomy sutures is eliminated and the ocular surface suffers less trauma. Although faster visual improvement does not translate into better long-term visual outcomes, it is important if there is impaired vision in the other eye. Elimination of sutures and conjunctival incisions greatly reduces damage to the conjunctiva, Tenon’s capsule, and episclera, which is crucial for eyes with a glaucoma filtering procedure and eyes likely to have glaucoma surgery in the future. Reduced conjunctival damage is also advantageous for patients with ocular surface disorders.
It was initially thought that 25G fluidics would be limiting but this has not proven to be the case. As will be discussed later in this chapter, 25G fluidics are safer than 20G or 23G fluidics.
The new series of 25+™ (25 Plus) instruments from Alcon allows complex surgical maneuvers such as membrane peeling using cutter rather than a forceps, avoiding the use of scissors. The high cut rate (up to 5000 cpm), strong aspiration and escellent IOP control of the Constelation® system allows shaving the vitreous base with negligible traction to the surrounding tissues and retina. In the 25+™ vitrectomy probe design, the tip has been redesigned to place the port closer to the distal end of the probe, allowing vitreous shaving closer to the retina.
The port size has also been enlarged to increase aspiration rate, And the shaft has been stiffened to reduce flexure and improve control (Figs. 17-1 and Figs. 17-2).
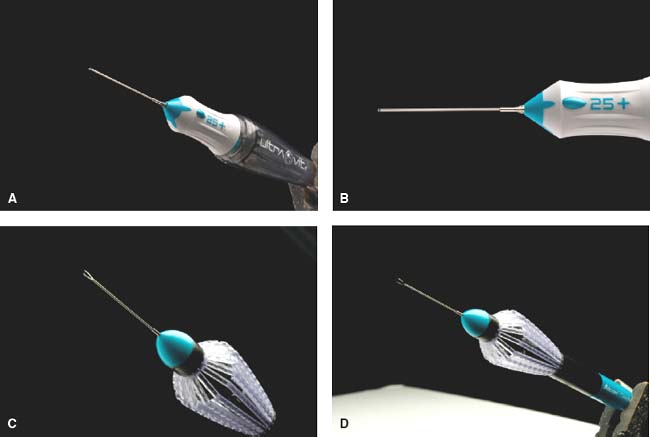
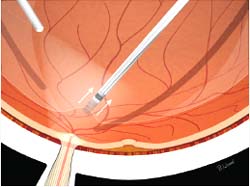
Figure 17-1. A and B: Shows new vitrctomy probe 25-G Plus. C and D: Shows Grieshaber 25-G Plus disposable forceps.
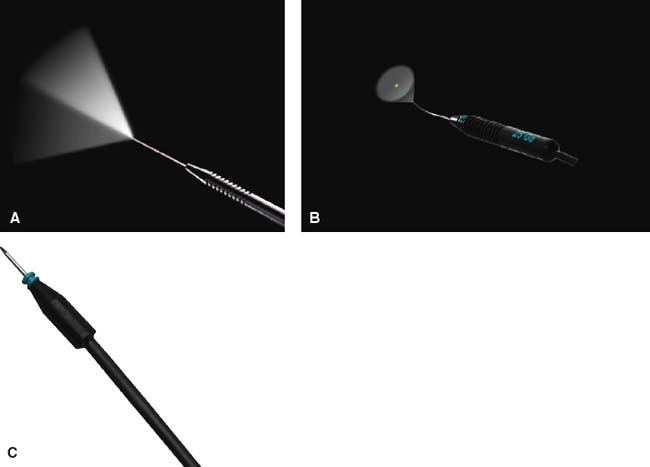
Figure 17-2. A: Illuminated pick 25-G Plus B: Illuminated fotocoagulation probe 25-G Plus C: Chandelier –w-sleeve –close 25-G Plus.
WOUND CONSTRUCTION
Displacement of the conjunctival wound relative to the sclerotomy site before insertion of the trocar cannula ensures that conjunctiva will cover the self-sealed sclerotomy (Fig. 17-3). Although the author initially utilized straight-in sclerotomies supplemented with fluid-air exchange, experimental leak pressure data from Kupperman and histological data from Kaiser made it clear that angulated wound construction was safer. Angulated (oblique, near-tangential) sclerotomies are not biplanar, although the motion of the trocar cannula needed to construct these incisions suggests this. The trocar should be inserted nearly tangential to the sclera until the polyimide cannula contacts the conjunctiva; the trocar should then be tilted up until closer to perpendicular to the scleral surface; and the insertion should be continued until the hub is flush with the conjunctiva, compressed against the sclera. This biplanar trajectory approach ensures creation of a scleral tunnel while preventing damage to the retina and choroid, especially in soft eyes and eyes with retinal detachments or choroidals.
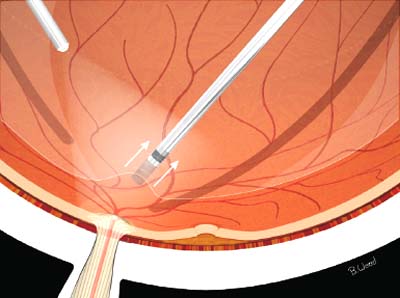
Figure 17-3. Displacement of the conjunctival wound relative to the sclerotomy site before insertion of the trocar-cannula ensures that conjunctiva will cover the self-sealed sclerotomy.
Sclerotomy placement is an often overlooked detail; the superotemporal site should be on a virtual line extending from the lowest point of the supraorbital rim to the center of the pupil. The superonasal site should be on a virtual line extending from the lowest point of the bridge of the nose to the center of the pupil. This approach reduces tool flex, especially when accessing the periphery and viewing with the binocular indirect ophthalmomicroscope (BIOM). The inferotemporal infusion site should be placed just inferior to the 3 or 9 o’clock position to prevent contact with the lower lid. Pathology-specific pre- and intraoperative head positioning facilitates surgical access and reduces tool flex as well.
At the end of the case, the cannulas should be removed in a tangential manner with the intraocular pressure (IOP) at approximately 20 mm Hg, while pressing on the wound with the smooth, rounded back of the plug forceps to ensure tight apposition of the inside and outside scleral tunnel layers (Fig. 17-4). Every effort must be made to reduce vitreous in the sclerotomies to reduce postoperative vitreous collagen contraction resulting in peripheral retinal breaks. Vitreous wick is a major risk factor in postoperative endophthalmitis; intentionally leaving vitreous in the wound to reduce wound leaks is a dangerous idea. Always use subconjunctival antibiotics. Cataract surgeons operate in the anterior chamber and where topical antibiotics are effective, but topical antibiotics do not produce minimum inhibitory concentrations (MICs) in the vitreous cavity of phakic or pseudophakic eyes. Antibiotics should be injected well away from the sclerotomies to prevent reflux into the vitreous cavity and retina damage. Povidone iodine (Betadine) prep is essential to reduce the risk of endophthalmitis. Vitreous wicks are a far more important risk factor for endophthalmitis than wound leaks.

Figure 17-4. At the end of the case, the cannulas should be removed in tangential manner with the intraocular pressure (IOP) at approximately 20 mm Hg while pressing on the wound with the smooth, rounded back of the plug forceps to ensure tight apposition of the inside and outside scleral tunnel layers.
FLUIDICS AND CUTTING RATES
High cutting rates create resistance at the port because of frequent interruption of flow. Smaller lumens also restrict flow because resistance is proportional to the 4th power of the diameter of the lumen. The author coined the term “port-based flow limiting” to describe the effects of higher resistance at the port. Port-based flow limiting decreases pulsatile traction on attached retina. High cutting rates also decrease uncut collagen fiber travel, thereby reducing the likelihood of iatrogenic retinal breaks. Vitreoretinal traction is also reduced by moving the cutter to the vitreous, rather than sucking vitreous to port, an approach termed “continuous engage and advance vitrectomy.” Vitreoretinal traction is the result if the cutter is pulled back while cutting; it should always be advanced while suction force is applied. Many surgeons inappropriately use lower cutting rates during core vitrectomy; the best practice is to always use the highest setting and increase proportional vacuum until vitreous removal begins, with the port applied to the vitreous-infusion fluid interface.
NECESSITY OF CORE VITRECTOMY
Core vitrectomy should not be omitted because patients complain bitterly about floaters if the vitreous is not removed. Although the author developed the approach of performing macular surgery without core vitrectomy this was abandoned because it was not shown to reduce postoperative retinal detachment or cataract. Nuclear sclerosis progression is almost certainly due to higher oxygen tension after vitrectomy, as shown independently by Holekamp and Chang.
MACULAR HOLE SURGERY
25G vitrectomy is ideal for macular hole surgery. Core vitrectomy should be performed with the highest possible cutting rate and by moving the port to the vitreous, not sucking the vitreous to the port.
Posterior vitreous detachment (PVD) creation using an anteroposterior motion of the cutter without cutter activation at the superior, inferior, and nasal disk margins, (Fig. 17-5), not over the cup, theoretically reduces the risk of peripheral retinal breaks compared to lateral motion of the soft-tip cannula. PVD creation never presents a problem with 25G cutters when using anterior motion at the disk margins.
The specific mechanism of macular hole formation is not well understood but is related in some way to PVD formation. The Gass classification system is of minimal clinical value, while the ocular coherence tomography (OCT) is essential to determine if the hole is of full or partial thickness. It is clear that peeling of residual vitreous cortex, epiretinal membranes, and the internal limiting membrane (ILM) increase success rates. The author recommends ILM peeling in all cases, but believes that indocyanine green (ICG) increases the risk of toxicity and phototoxicity and is unnecessary when using end-opening forceps peeling of the ILM. There are an increasing number of reports suggesting that ICG is toxic and its use is decreasing. The BIOM and other wide-angle systems decrease axial and lateral resolution and are probably a factor in the use of ICG, trypan blue, and triamcinolone to improve ILM visualization. There are anecdotal reports that triamcinolone reduces closure rates in macular hole surgery. The flat contact lens provides far superior resolution and should be used for all macular surgery. The Tornambe Torpedo and other chandeliers provide diffuse illumination, which makes visualization of ILM more difficult; focal illumination with a standard Alcon 25G, 78-degree endoilluminator (Fig. 17-6) is preferred by the author.
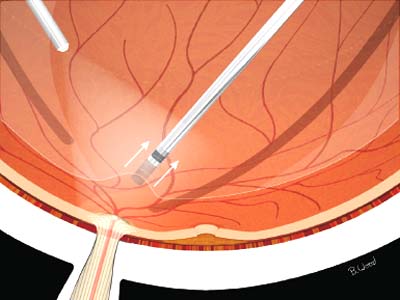
Figure 17-5. Posterior vitreous detachment (PVD) creation using anteroposterior motion of cutter without cutter activation at the superior, inferior and nasal disk margins, not over the cup, theoretically reduces the risk of peripheral retinal breaks compared to lateral motion of the soft-tip cannula.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


