Steroid-Induced Glaucoma
A certain percentage of the general population responds to repeated instillation of systemic or ocular corticosteroids with a variable increase in the intraocular pressure (IOP) (see Chapter 11). This appears to have been reported first by McLean in 1950, after administration of corticotropin (ACTH) and cortisone systemically (1), and then by François (2), after local administration of cortisone. It occurs more commonly in individuals who have chronic open-angle glaucoma (COAG) or a family history of the disease. There are many unknown facets regarding the pressure response to steroids, such as the precise distribution of steroid responders in the general population, the reproducibility of these responses, and hereditary influences. Nevertheless, the critical fact is that certain people do manifest this response to long-term steroid therapy, whether given by the topical, systemic, periocular, or intraocular route, and the IOP elevation can lead to glaucomatous optic atrophy and loss of vision. Such a condition is referred to as steroid-induced glaucoma.
CLINICAL FEATURES
The typical clinical presentation of steroid-induced glaucoma is associated with topical, periocular, intraocular, or oral steroid therapy, although it can occur with any type of steroid administration. IOP elevation usually develops within a few weeks with potent topical or intraocular corticosteroids or in months with the weaker steroids (3,4). The clinical picture resembles that of COAG, with an open, normal-appearing anterior chamber angle and absence of symptoms. Much less often, the condition may have an acute presentation, and pressure rises have been observed within hours after steroid administration in eyes with open angles (3,5). This reaction has been seen with intensive systemic steroid therapy, with the topical use of potent corticosteroids, and with the use of intravitreal triamcinolone in patients with pseudophakia.
Although children appear to have a lower incidence of positive steroid responses than adults do (6), IOP elevation has been reported with treatment of external diseases in infants with corticosteroids, with nasal and inhalational steroids, and with corticosteroid eyedrops after strabismus surgery in children younger than 10 years (7–9). After strabismus surgery and the use of topical dexamethasone, IOP increased in a dose- and age-dependent manner in Chinese children; children younger than 6 years were especially at high risk (10). However, long-term, low-dose oral prednisone therapy in children was not associated with higher-than-normal IOPs in one study (11).
IOP elevation may occur in the first few weeks after a trabeculectomy despite a good filtering bleb, possibly because of the influence of topical steroid therapy (12). Steroid-induced glaucoma may also mimic low-tension glaucoma when the steroid-induced pressure elevation has damaged the optic nerve head and visual field in the past, but the IOP has subsequently returned to normal with cessation of steroid use (13).
Since the early 1990s, with the advent of laser refractive surgery and concomitant use of postoperative steroids, cases of severe IOP elevation and serious optic nerve damage have been reported (14,15). One explanation for this may be a failure to recognize the elevated IOP because of refractive surgery–induced errors in the accuracy of applanation tonometry (16). Reasons for a falsely low IOP reading after refractive surgery that can mask steroid-induced glaucoma include central corneal thinning, ocular rigidity changes, corneal edema, or fluid accumulation beneath a laser in situ keratomileusis (LASIK) flap (17,18).
IOP elevation secondary to steroid use has also been reported as a mechanism for glaucoma after Descemet-stripping endothelial keratoplasty (19).
THEORIES OF MECHANISM
It is generally agreed that the IOP elevation due to steroid administration results from reduction in facility of aqueous outflow. (Detailed references in this regard can be found in review articles by Jones and Rhee (4) and Kersey and Broadway (20).) The precise mechanism responsible for the obstruction to outflow is unknown, but the following observations and theories have been reported.
Nuclear Transport of Glucocorticoid Receptor
Glucocorticoids have been shown to alter trabecular meshwork cell morphology by causing an increase in nuclear size and DNA content (21). Experiments on cultured human trabecular meshwork cells exposed to dexamethasone have demonstrated that the FK506-binding immunophilin FKBP51 mediates nuclear transport of the human glucocorticoid receptor GRbeta (22), suggesting that this plays a role in increased glucocorticoid responsiveness.
Influence on Extracellular Matrix
François (23–25) postulated that glycosaminoglycans in the polymerized form become hydrated, producing a “biologic edema” that may increase resistance to aqueous outflow. Hyaluronidase in lysosomes depolymerizes hyaluronate, and corticosteroids stabilize the lysosomal membrane, which may lead to an accumulation of polymerized glycosaminoglycans in the trabecular meshwork.
Animal and tissue culture and organ perfusion experiments have demonstrated outflow obstruction in response to corticosteroids. Topical dexamethasone–induced IOP elevation in rabbits was associated with an increase in chondroitin sulfate in the aqueous outflow pathway but a decrease in hyaluronic acid (26). Dexamethasone can decrease the synthesis of collagen in normal human trabecular meshwork explants and decrease the extracellular activity of tissue plasminogen activator (27,28). In cultured human trabecular meshwork cells, glucocorticoids increased the expression of the extracellular matrix protein fibronectin, glycosaminoglycans, and elastin, increased depositions of which are also seen in the outflow pathways of patients with COAG (29,30).
Influence on Phagocytosis
Endothelial cells lining the trabecular meshwork have phagocytic properties, which may help to clean the aqueous of debris before it reaches the inner wall of the Schlemm canal. Corticosteroids are known to suppress phagocytic activity, and suppressed phagocytosis of the trabecular endothelium may allow debris in the aqueous to accumulate in the meshwork and act as a barrier to outflow (31). In support of this are experiments that demonstrate the formation of cross-linked actin networks in the trabecular meshwork cytoskeleton with exposure to dexamethasone (32). This theory of reduced phagocytic activity is also consistent with ultrastructural studies showing marked depositions of amorphous and fibrous or linear material in the juxtacanalicular meshwork of eyes with steroid-induced glaucoma (33,34).
Genetic Influences
With the discovery that mutations in several genes are associated with familial COAG and with the knowledge that patients with COAG and their relatives are at increased risk for steroid-induced IOP elevation, there has been interest in searching for the involvement of these genes in humans and in animal models of steroid-induced glaucoma. Studies have shown no evidence for a link between myocilin or optineurin mutations and steroid-induced ocular hypertension (35). Microarrays and macroarrays have been used to study differential gene expression between cultured human trabecular meshwork cells, with and without exposure to dexamethasone. These experiments, which require confirmation, have revealed multiple genes that may be involved in protective and damaging mechanisms with IOP elevation that are upregulated with dexamethasone (in addition to myocilin): α1-antichymotrypsin, pigment epithelium–derived factor, cornea-derived transcript 6, prostaglandin D2 synthase, growth arrest specific 1, decorin, insulin-like growth factor binding protein 2, ferritin light chain, and fibulin-1C (36–38). Much more work needs to be done to determine which of these genes are upregulated in vivo and which of these and other genes play a role in increasing outflow resistance in response to steroid application.
Outflow Obstruction by Steroid Particles
In a case series by Singh and colleagues, three patients experienced a rapid rise in IOP after receiving intravitreal triamcinolone injections for diabetic macular edema (39). All three patients had pseudophakia and required surgical intervention to control their IOP. A peculiar finding was the presence of white crystals in the angle of one patient, suggesting direct physical obstruction of the trabecular meshwork with crystalline steroid particles. Another study that monitored the elevation of IOP after administration of a single dose of intravitreal triamcinolone noted that four of six eyes requiring topical administration of IOP-lowering agents after the injection had postinjection abnormalities in the inferior angle—characterized by pigmented particulate matter—that had not been present at the baseline examination (40).
Animal Models
Animal models of steroid-induced glaucoma have been reported in monkeys, beagles, and sheep, although the pathogenic mechanisms are unclear (41–43).
PREVENTION
To avoid loss of vision from steroid-induced glaucoma, physicians must know how to prevent or minimize the chances of its occurrence. This requires close attention to the patient’s history and to the selection and use of steroids.
Patient Selection
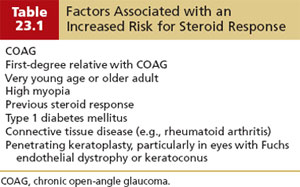
Individuals with COAG or a family history of the disease are more likely than other persons to respond to long-term steroid therapy with a significant rise in IOP. The same is true for young children and older adults, and persons with highly myopic eyes, diabetes mellitus, or connective tissue disease (especially rheumatoid arthritis) (Table 23.1) (44–49). All such persons who undergo long-term steroid treatment are therefore at increased risk for steroid-induced glaucoma. However, because it is impossible to predict which individuals will have a pressure rise, all patients should be observed closely. Physicians should avoid steroid use when a safer drug will suffice. If a steroidal agent must be used, the patient should receive the lowest possible amount of drug over the shortest duration needed. In addition, it is wise to establish a baseline IOP before initiation of corticosteroid therapy, and the tension should be monitored closely for the duration of the therapy.
Drug Selection
When corticosteroid therapy is required for any disorder, the optimum drug is the one that can achieve the desired therapeutic response by the safest route of administration in the lowest concentration and with the fewest potential adverse reactions. With regard to the IOP response, the following observations should be considered.
Routes of Administration
Topical Therapy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


