Glaucomas Associated with Elevated Episcleral Venous Pressure
EPISCLERAL VENOUS PRESSURE
The episcleral venous pressure is one factor that contributes to the intraocular pressure (IOP). The normal episcleral venous pressure is approximately 8 to 10 mm Hg (1–5), although recorded values vary according to the measurement technique used. (The instruments for measuring episcleral venous pressure are described in Chapter 2 (1,2,4,5).)
It is commonly thought that for every mm Hg increase in episcleral venous pressure, there is an equal rise in IOP, although the magnitude of IOP rise may be greater than the rise in venous pressure (6). Studies of chronic open-angle glaucoma have revealed no significant abnormality of episcleral venous pressure (2,5,7). In one study, however, the episcleral venous pressure was slightly higher in patients with primary open-angle glaucoma (12.1 mm Hg) or normal-tension glaucoma (11.6 mm Hg) than in control eyes (9.5 mm Hg) (8). There are, in fact, various conditions in which elevated episcleral venous pressure can produce characteristic forms of associated glaucoma. These conditions are the subject of this chapter.
GENERAL FEATURES OF ELEVATED EPISCLERAL VENOUS PRESSURE
The following findings are common to most eyes with abnormally elevated episcleral venous pressure.
External Examination
The most consistent feature is variable degrees of dilatation and tortuosity of the episcleral and bulbar conjunctival vessels. Additional findings may include chemosis, proptosis, orbital bruit, and pulsations over the orbit; however, these findings are inconsistent and depend on the underlying cause of the elevated episcleral venous pressure.
Intraocular Pressure
The rise in IOP is approximately equal to the rise in episcleral venous pressure. The resultant tension is typically in the mid-20s to mid-30s, and the ocular pulse amplitude is often increased (9).
Gonioscopy
The anterior chamber angle is typically open, and the only abnormality may be blood reflux into the Schlemm canal. However, the latter feature is of limited diagnostic value, because it is found inconsistently in eyes with elevated episcleral venous pressure and may be seen in healthy eyes.
Tonography
The facility of aqueous outflow is characteristically normal. A study with monkeys revealed that elevated venous pressure was associated with increased outflow (10), which may partly result from a widening of the Schlemm canal. However, prolonged elevation of episcleral venous pressure often leads to reduced outflow facility, which may persist after the venous pressure has normalized (9).
CLINICAL FORMS OF ELEVATED EPISCLERAL VENOUS PRESSURE
The various causes of elevated episcleral venous pressure may be considered to fall into three categories: obstruction to venous flow, arteriovenous fistulas, and idiopathic episcleral venous pressure elevation (5).
Venous Obstruction
Thyroid-Associated Ophthalmopathy
Thyroid-associated ophthalmopathy is also referred to as endocrine exophthalmos or Graves ophthalmopathy. The precise hormonal basis for the condition is uncertain, although the ocular pathology consists of orbital infiltration, including the extraocular muscles, with lymphocytes, mast cells, and plasma cell. This is the most common cause of unilateral and bilateral proptosis. In addition to glaucoma, other serious complications of thyroid-associated ophthalmopathy include corneal exposure due to proptosis or lid retraction and optic nerve compression from the orbital mass.
The glaucoma may occur by several mechanisms. The episcleral venous pressure may be elevated in severe cases of thyroid-associated ophthalmopathy with marked proptosis and orbital congestion due to obstruction of venous flow through the orbit (Figs. 20.1 and 20.2). This increases the IOP. A less common mechanism of glaucoma is anterior chamber inflammation, which may result from corneal exposure and ulceration.
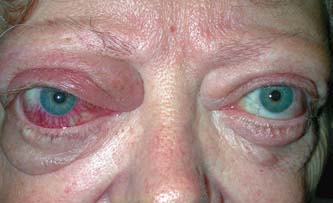
Figure 20.1 Asymmetrical exophthalmos, with congestive features greater in the right eye, in a patient with thyroidassociated ophthalmopathy. (Courtesy of Julie A. Woodward, MD.)
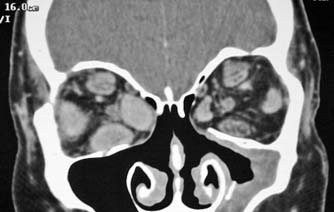
Figure 20.2 Orbital computed tomography scan of the patient in Figure 20.1 with thyroid-associated ophthalmopathy. Note the massively enlarged rectus muscles in the right orbit. (Courtesy of Julie A. Woodward, MD.)
Contracture of extraocular muscles, which occurs in the later, fibrotic phases of the infiltrative ophthalmopathy, may affect the IOP in different fields of gaze. Typically, fibrosis of the inferior rectus muscle causes resistance to upgaze, which is associated with a rise in the measured IOP when the patient looks up. In some cases, an artificial pressure elevation may be recorded with gaze in the usual straight-ahead position, and the patient should be allowed to change the direction of gaze to their “resting” position (11). Ideally, the IOP should be measured in several fields of gaze to avoid this potential artifact of testing. Thyroid dysfunction may be associated with abnormal scleral rigidity; the IOP in patients with thyroid dysfunction should be measured by using applanation tonometry or another tonometer that affects scleral rigidity only minimally (as described in Chapter 2).
Superior Vena Cava Syndrome
Lesions of the upper thorax may obstruct venous return from the head, causing elevated episcleral venous pressure in association with exophthalmos, edema, and cyanosis of the face and neck, and dilated veins of the head, neck, chest, and upper extremities (12).
Orbital Amyloidosis
Rare cases of localized orbital amyloidosis with secondary glaucoma related to elevated episcleral venous pressure have been reported (13,14). Nelson and colleagues (14) postulate that perivascular infiltration of amyloid around extraocular vessels may contribute to raising the episcleral venous pressure. Other conditions that may occasionally obstruct orbital venous drainage include retrobulbar tumors and cavernous sinus thrombosis.
Arteriovenous Fistulas
Carotid–Cavernous Sinus Fistulas
Carotid–cavernous sinus fistulas can be subdivided into two categories. About three fourths of these fistulas are caused by trauma and are characterized by a direct vascular communication and high blood flow. The remaining cases occur spontaneously and typically have an indirect or dural communication with low flow (15).
Traumatic Fistulas
The typical trauma is severe head injury, which results in a large fistula between the internal carotid artery and the surrounding cavernous sinus venous plexus. This condition is characterized by pulsating exophthalmos, a bruit over the globe, conjunctival chemosis, engorgement of epibulbar veins, restriction of motility, and evidence of ocular ischemia (15–18). The shunting of blood through the internal carotid–cavernous sinus fistula increases blood flow and produces high venous pressure (15,19).
Spontaneous Fistulas
Spontaneous carotid–cavernous sinus fistula occurs most often in middle-aged or older women with no history of trauma. A small fistula in these cases is fed by a meningeal branch of the intracavernous internal carotid artery or external carotid artery, which empties directly into the cavernous sinus or an adjacent dural vein that connects with the cavernous sinus (19,20). The mixing of arterial and venous blood leads to a reduction in arterial pressure and an increase in orbital venous pressure, which increases the episcleral venous pressure. Patients with this condition have prominent episcleral and conjunctival veins—often their reason for seeking care—but they have minimal proptosis and no pulsations or bruit. The small fistula results in low-flow, low-pressure shunting (19). Most patients have elevated IOPs. The condition has been called red-eyed shunt syndrome (19) or dural shunt syndrome (20).
Orbital Varices
The condition of orbital varices is characterized by intermittent exophthalmos and elevated episcleral venous pressure, usually associated with stooping over or the Valsalva maneuver (6,21). Because venous pressure is typically normal between episodes, associated glaucoma is uncommon. However, glaucomatous damage has been reported to occur, and it has been suggested that management with antiglaucoma medications may be effective and should be tried before surgical intervention is considered (6).
Sturge–Weber Syndrome
One mechanism of IOP elevation in Sturge–Weber syndrome is believed to be elevated episcleral venous pressure due to the episcleral hemangiomas with arteriovenous fistulas (22,23). (The Sturge–Weber syndrome is discussed in more detail in Chapter 21.)
Idiopathic Episcleral Venous Pressure Elevation
Several reported cases have involved dilated episcleral veins (Fig. 20.3) and open-angle glaucoma without exophthalmos or any explanation for the venous congestion (24–30). The typical patient is elderly with no family history of the condition, although it may be seen in young adults and has been described in a mother and daughter (24). Most cases are unilateral, and those in which episcleral venous pressure has been measured have all had elevated venous pressures (24,27,30). The cause of the elevated episcleral venous pressure is unknown. In one series of five patients with unilateral elevation of episcleral venous pressure and open-angle glaucoma, venous outflow was determined to be normal by orbital venography, and the mechanism was presumed to be a localized venous obstruction in the region of the extraocular muscles (30). The associated glaucoma may be severe, with advanced glaucomatous damage.
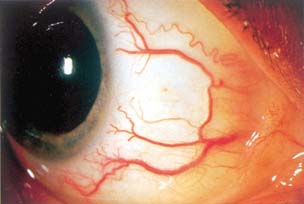
Figure 20.3 Temporal quadrant in a patient with idiopathic elevated episcleral venous pressure. Note how the episcleral veins begin as small, tapered vessels just behind the limbus and become larger as they coalesce and course posteriorly. This contrasts with anterior ciliary arteries, which are more tortuous than the episcleral veins in the normal state and end abruptly just behind the limbus. One such artery is seen in the upper portion of the image. Although arteries normally are more prominent than episcleral veins are, the opposite is true in eyes with elevated episcleral venous pressure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


